Chapter 6
Clinical Audit
Aims
This chapter aims to explain the principles of clinical audit and how the process of clinical audit can be used as a quality improvement tool. It also aims to give examples of audits where there has been a demonstrable improvement in performance as a result of carrying out the audit.
Outcome
Having read this chapter, the reader should be aware of the importance of clinical audit as a quality improvement tool and understand how the principles of audit may be applied to clinical practice.
Introduction
Clinical audit is an important quality improvement process, and a most effective tool for clinical governance. In the UK, the Department of Health described clinical audit (and peer review) as “a central pillar of clinical governance” and all dentists practising within the NHS were required to participate in a rolling programme of audits/peer reviews. This improvement in quality will be reflected in:
-
improved care of patients
-
consistent care of patients
-
enhanced professionalism of staff
-
efficient use of resources
-
more effective administration
-
accountability to those outside the profession
-
increased patient satisfaction.
It is not a new process; as early as 1750 BC, King Hammurabi of Babylon involved clinicians in audit, with financial penalties being imposed in the event of poor performance.
Audit has been defined in the UK by both the National Institute for Health and Clinical Excellence (NICE) and the Healthcare Commission as: “A quality improvement process that seeks to improve the patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structures, processes and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual, team, or service level and further monitoring is used to confirm improvement in healthcare delivery.”
Audits can take a retrospective or prospective sample. Retrospective audit looks at past care. It is particularly useful where there has been a critical incident such as a patient complaint, adverse outcome or litigation. Such incidents usually prompt an urgent review of processes and standards and audit provides the mechanism.
Prospective audit looks at future care. Unlike retrospective audit, it reflects current practice and allows for accurate real time accrual of data, which means that the data should be accurate both in terms of detail and volume.
The Audit Cycle
Clinical audit is often described as a cycle or a spiral (Fig 6-1).
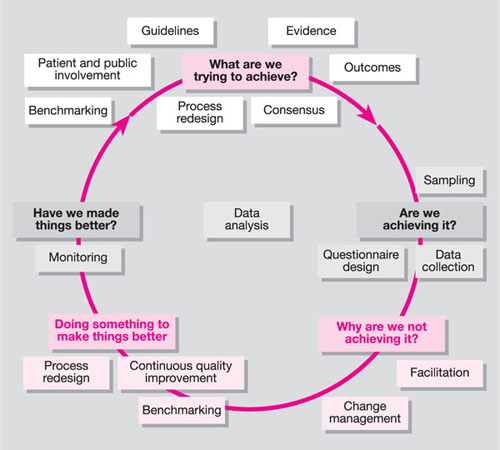
Fig 6-1 The audit cycle. Taken from: National Institute for Clinical Excellence. Principles for best practice in clinical audit. Oxford: Radcliffe Medical Press, 2002.
Selecting an Audit Project
An audit project may be selected on the basis of:
-
high volume
-
high risk
-
high profile
-
high cost
-
known weaknesses.
We should ask the following questions:
-
Is there any evidence of a serious quality problem?
Are there patient complaints or high post-operative patient return/complication rates? -
Is good evidence available to inform standards?
Standards will need to be identified – we need to know where we can source these. -
Is the identified problem amenable to change?
If there is limited scope for change, then the value of the audit is limited because it may not be possible to achieve sustainable improvement. -
Why is the topic a priority for the practice?
Why should this topic be selected above others? -
Will team members recognise the value of the audit?
The team must recognise the importance and the value of the topic. Team buy-in is important to implement effective change.
Undertaking the Audit
To undertake the audit, we need to address the following questions:
-
Will the data be collected retrospectively or prospectively?
-
What is the sample size?
-
What are the sample criteria to be?
-
What data do you want to collect?
-
Who will collect the data?
-
Who will analyse the data?
-
How will data be collected, i.e. using a computer or by hand?
Review the Findings
Having collected and analysed your data, you will need to identify what areas may need changing. This can be done by:
-
summarising your findings in a form that is easy to digest
-
arranging a team meeting to discuss the audit results
-
adopting an agreed strategy for change.
Implementation of Change
Having decided what changes are needed, you will have to consider a reasonable time frame in which to implement the changes. This means:
-
agreeing on a d/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


