Aggressive Periodontitis and Occlusal Trauma

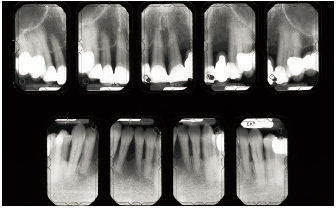
Fig 6-1a Aggressive periodontitis in a 50-year-old, otherwise healthy male patient experiencing stress at work. He is an occasional smoker. A partial denture replaces the missing maxillary left central incisor. Cultural analysis disclosed Prevotella intermedia (14.7%) and Fusobacterium nucleatum (2.4%). Infection type is commensal.
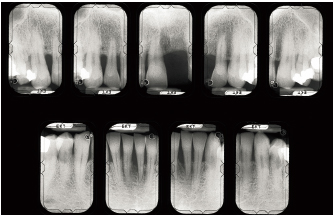
Fig 6-1b Bone destruction is irregularly distributed and is locally terminal around the maxillary right central and lateral incisors and is severe around the mandibular left central incisor. Severity factors: Significant plaque buildup; occlusal trauma induced by partial denture. Risk factors: Predisposition, stress.

Fig 6-1c Global treatment strategy: Local treatment (removal of toothborne plaque, scaling and root planing), functional treatment (provisional crown and extraction of the maxillary right central incisor and left lateral incisor), occlusal rehabilitation (elimination of occlusal discrepancy on the mandibular left central incisor), antibiotic therapy (metronidazole 500 mg tid for 8 days), and periodontal surgery.
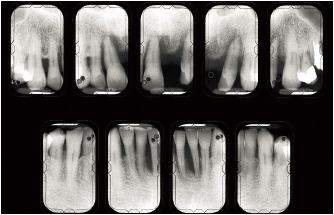
Fig 6-1d Endodontic treatment is carried out on the maxillary right canine and lateral incisor and the left canine to reduce the crown-root ratio. Note the significant repair occurring around the right lateral incisor and left canine.

Fig 6-1e After prosthetic rehabilitation and supportive therapy three times a year, the patient is able to monitor accumulation of plaque.
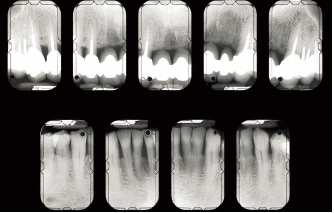
Fig 6-1f Favorable response potential (bone repair, attachment gain, reduction of pocket depth, and reduction of mobility) is easy to observe around the mandibular left central incisor.
Aggressive Periodontitis and Loss of Posterior Occlusal Support
Fig 6-2a Aggressive periodontitis in a 49-year-old, otherwise healthy, nonsmoking female patient. Clinical signs: Few deposits, mild inflammatory signs, incisor migrations and egressions (newly onset diastema 1 year ago), mobility, pockets, no posterior contacts, functional disturbance, partial denture to replace the mandibular right central incisor. Cultural analysis: P intermedia (13.8%), F nucleatum (0.1%), Capnocytophaga spp (0.1%), Campylobacter rectus (0.1%); high plaque scores.
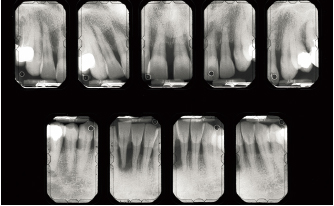
Fig 6-2b Radiographic signs: Significant, irregular bone destruction (terminal around the mandibular right central incisor before it was extracted). Severity factors: Local factors, functional factors (collapse of posterior occlusion). Risk factors: Possible predisposition. Diagnosis: Aggressive periodontitis involving infection by commensal flora.

Fig 6-2c Initial treatment: Oral hygiene instructions, removal of dental plaque and calculus, provisional occlusofunctional rehabilitation and restoration of lateral occlusion, scaling and root debridement. Clinical signs indicate improvement: the diastema is narrowing.

Fig 6-2d After a course of antibiotic therapy (amoxicillin 500 mg tid for 8 days), undertaken because of persistent bleeding in deep pockets, surgery is performed in areas where persistent pockets display probing depths exceeding 5 mm.

Fig 6-2e Rehabilitation of posterior regions with fixed prostheses and of the anterior region with a fixed prosthesis for the mandibular right central incisor) is performed. The diastema reduced spontaneously after surgery.
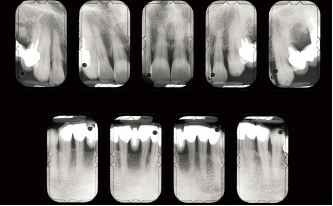
Fig 6-2f Six years after the beginning of treatment. Response to therapy is favorable: repair and attachment gains have occurred in sites where destruction was most significant.
Advanced Chronic Periodontitis with Multiple Associated Disorders
Fig 6-3a A 55-year-old, otherwise healthy, nonsmoking female patient. The patient has never undergone any dental cleanings and brushes once a day. Signs: Deposits, presence of plaque, severe inflammation, halitosis, occlusal disturbance, anterior overjet, diastema, mobility, discomfort, and pain. Multiple local factors: Bacterial, dental, prosthetic, and functional. Diagnosis: Advanced chronic periodontitis.

Fig 6-3b Treatment consists of managing inflammation and correcting local and functional factors. Periodontal surgery is performed throughout the dentition. Three sites receive specific treatment: the maxillary left lateral incisor and mandibular right central incisor were extracted, and the maxillary left canine underwent guided tissue regeneration therapy (see Figs 6-5a to 6-5h).

Fig 6-3c The goal of this iatrogenic prosthetic device was to correct a primary anterior underbite and to act as a splinting device for the incisors. A new underbite appeared, most likely secondarily to lingual hyperfunction.

Fig 6-3d When the anterior prosthetic device is removed, the incisors are intact. The right central incisor is extracted. This promotes spontaneous realignment of the three remaining incisors, correction of ectopic buccal position of the mandibular right canine, and spontaneous closure of the diastema between the maxillary central incisors, all of which contribute to restoring periodontal health.
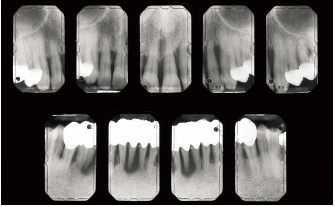
Fig 6-3e Destruction around anterior teeth is extremely severe (particularly around the maxillary left lateral incisor and canine, the mandibular central incisors, and the right lateral incisor). Attachment losses and pocket depths are very significant. A conservative approach allows for a continuous evaluation of the response to treatment.

Fig 6-3h Favorable response to periodontal treatment, which consisted of local and surgical management. Antibiotic therapy (amoxicillin 500 tid for 8 days) is administered during the days before and after regeneration surgery around the maxillary left canine.

Fig 6-3i Inflammation is more severe in sites where restorations are poorly adapted.

Fig 6-3j The second premolar had exhibited terminal bone destruction and Class IV mobility and was extracted. Favorable periodontal response occurred following treatment. Abutment design on the molar allows for future access to pulp in the event that root amputation is indicated (Class II).

Fig 6-3k There is a direct relation between the degree of inflammation and the amount of plaque-derived biofilm.
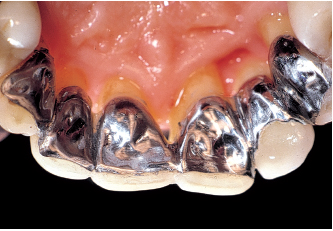
Fig 6-3l A bonded, removable pontic-splint replaces the left lateral incisor, stabilizes the central incisors, and ensures splinting before guided tissue regeneration is initiated around the left canine.
Advanced Chronic Periodontitis and Orthodontics
Fig 6-4a Advanced chronic periodontitis in a 45-year-old female patient. Dental displacements and secondary diastemata are significant. There is no canine guidance on the left. The maxillary left lateral incisor presents Class III mobility. Esthetics are compromised.
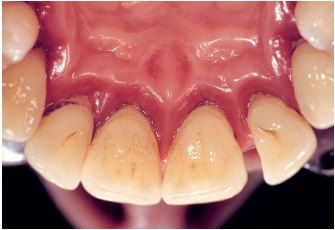
Fig 6-4b Signs of inflammation are generalized and correlate to the amount of bacterial deposits. Infection is commensal.

Fig 6-4c Infection control is achieved through the usual protocol: crown and root debridement, scaling, and root planing (four sessions), followed by periodontal surgery. Because teeth malpositions have not improved, orthodontic management is required.

Fig 6-4d Dental displacements and diastemata have been corrected. Note healthy gingival tissue.
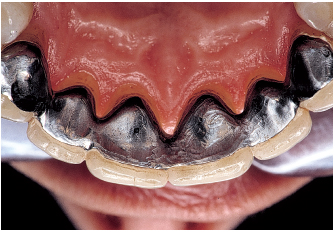
Fig 6-4e A bonded splint stabilizes the anterior teeth, canine to canine.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses