Coronal Polishing
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Explain the difference between a prophylaxis and coronal polishing.
• Explain the indications for and contraindications to a coronal polish.
• Name and describe the types of extrinsic stains.
• Name and describe the two categories of intrinsic stains.
• Describe the types of abrasives used for polishing the teeth.
• Describe the types of abrasives used for porcelain esthetic restorations.
• Name materials to be avoided when one is polishing esthetic restorations.
• Describe the technique used for polishing esthetic restorations.
• Demonstrate safety precautions to be followed during coronal polish.
• In states where it is legal, demonstrate coronal polishing technique.
Performance Outcomes
On completion of this chapter, the student will be able to achieve competency standards in the following skills:
• Demonstrate the handpiece grasp and positioning for the prophy angle.
• Demonstrate the fulcrum or finger rest used in each quadrant during a coronal polish procedure.
• Be able to determine that the teeth are free from stains and plaque.
Electronic Resources
![]() Additional information related to content in Chapter 58 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 58 can be found on the companion Evolve Web site.
![]() and Multimedia Procedures DVD
and Multimedia Procedures DVD
Key Terms
Calculus (KAL-kyoo-lus) Calcium and phosphate salts in saliva that become mineralized and adhere to tooth surfaces.
Clinical crown That portion of the tooth that is visible in the oral cavity.
Coronal (kuh-ROE-nuhl) polishing A technique used to remove plaque and stains from the coronal surfaces of the teeth.
Endogenous (en-DOJ-en-us) stains Stains developed from within the structure of the tooth.
Exogenous (ek-SOJ-uh-nus) stains Stains developed from external sources.
Extrinsic (ek-STRIN-zik) stains Stains that occur on the external surfaces of the teeth that may be removed by polishing.
Fulcrum (FUL-krum) Finger rest used when an instrument or handpiece is held for a specified time.
Intrinsic (in-TRIN-zik) stains Stains that occur within the tooth structure that may be removed by polishing.
Oral prophylaxis (proe-fi-LAK-sis) The complete removal of calculus, debris, stain, and plaque from the teeth.
Prophy paste Commercial premixed abrasive paste used for polishing teeth and restorations.
Rubber cup polishing A technique that is used to remove plaque and stains from the coronal surfaces of the teeth.
Coronal polishing is a technique that is used to remove plaque and stains from the coronal surfaces of the teeth. (Refer to Chapter 15 for a discussion of dental plaque.) Polishing the crowns of teeth is considered to be primarily a cosmetic procedure. However, a smooth tooth surface is less likely to retain plaque, calculus, and stain.
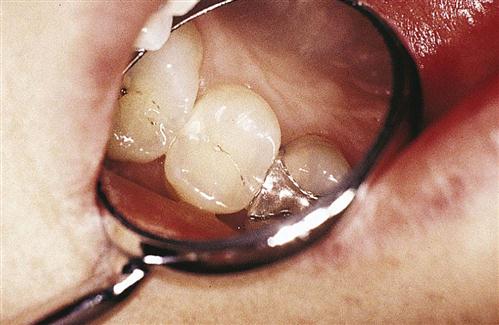
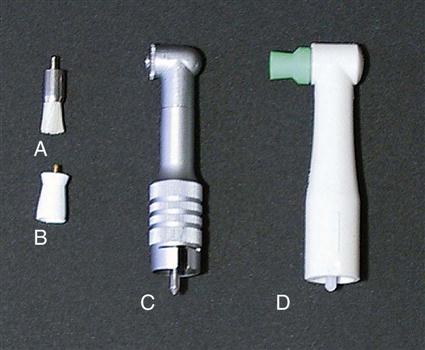
In addition, patients like the feel of smooth, polished teeth. Coronal polishing is most commonly done with the use of a dental handpiece with a prophy angle (Fig. 58-1), a rubber cup, and a polishing material (abrasive agent). Specific indications for and contraindications to a coronal polish are listed in Box 58-1.
Coronal polishing is strictly limited to the clinical crowns of the teeth. (The clinical crown is that portion of the tooth that is visible within the oral cavity.) In some states, coronal polishing is delegated to registered or expanded-functions dental assistants (EFDAs) who have had special training in this procedure.
It is very important to understand the difference between a prophylaxis and a coronal polishing. A coronal polish is not a substitute for an oral prophylaxis. An oral prophylaxis, commonly known as a prophy or a cleaning, is the complete removal of calculus, debris, stain, and plaque from the teeth. (Calculus is a hard mineralized deposit that is attached to the teeth.) In almost every state, the dentist and the registered dental hygienist are the only members of the dental team who are licensed to perform an oral prophylaxis.
Selective Polishing
Selective polishing is a procedure in which only those teeth or surfaces with stain are polished. Studies have shown that the abrasive agent used during coronal polishing actually removes a small amount of the fluoride-rich outer enamel layer. The purpose of selective polishing is to avoid unnecessary removal of even small amounts of surface enamel. Therefore, when the stain is very light and is not of esthetic concern to the patient, selective polishing should be considered. The basic principle of selective polishing is that teeth should not be polished unless it is necessary. For some individuals, stain removal may cause dentinal hypersensitivity during and after the appointment. The needs of the patient must always be reviewed before stain removal. If you encounter a patient who does not have visible stain but is accustomed to polishing and chooses to have it done, you should use a very fine abrasive such as a commercial toothpaste.
Historically, teeth were polished to remove all soft deposits and stains before fluoride was applied because it was believed that uptake of the fluoride into the enamel would be increased. As scientific knowledge has evolved, it has been shown that polishing does not improve the uptake of professionally applied fluoride. Therefore, polishing is no longer necessary before fluoride is applied.
In addition to cosmetic value, coronal polishing can have therapeutic value. Therapeutic polishing refers to polishing of the root surfaces that have been exposed during periodontal surgery. (Refer to Chapter 55 for a review of periodontal surgery.) Polishing reduces the endotoxins and the bacteria on the cementum. Whether polishing for cosmetic or therapeutic purposes, it is important to understand the polishing process and its effects on the tooth surface (Box 58-2).
Dental Stains
Stains are primarily an esthetic problem. Some types of stain can be removed, whereas others cannot. It is important for the dental assistant to be able to correctly identify stains, to provide the patient with accurate information about the cause of the stains and possible options for removing them. For stains that cannot be removed, other treatment options are available. These include professional and at-home bleaching procedures, enamel microabrasion, and cosmetic restorative procedures such as laminate veneers and composite restorations.
Types of Stains
Dental stains are categorized as endogenous or exogenous in nature.
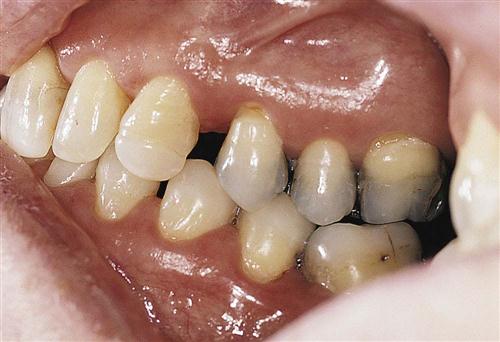
Endogenous stains originate within the tooth through developmental and systemic disturbances. Types of endogenous stains include those caused by an excessive amount of fluoride during formation of the tooth. Another example of an endogenous stain would be that resulting from medications taken by the mother or the child during tooth development. Tetracycline is an example of a medication that is known to cause developmental staining. Endogenous stains may be seen in both deciduous and permanent dentitions and cannot be removed by polishing (Figs. 58-2 through 58-6).
Exogenous stains are those that originate outside the tooth and are caused by environmental agents. These can be subdivided even further into extrinsic and intrinsic stains, depending on whether or not the stain can be removed.
Extrinsic stains are those stains that appear on the exterior of the tooth and can be removed. Examples include staining from food, drink, and tobacco. In these cases, the source of the stain is external, and the stain may be removed (Table 58-1).
TABLE 58-1
| Type of Stain | Appearance | Cause |
| Black stain | Thin black line on the teeth near the gingival margin. More common in girls. Frequently found in clean mouths. Difficult to remove | Caused by natural tendencies |
| Tobacco stain | A very tenacious dark brown or black stain | Caused by the products of coal tar in tobacco and by the penetration of tobacco juices into pits and fissures, enamel, and dentin of the teeth. Use of any tobacco-containing products causes tobacco stains on the teeth and restorations. |
| Brown or yellow stain | Most commonly found on the buccal surfaces of the maxillary molars and the lingual surfaces of the lower anterior incisors | Caused by poor oral hygiene or by the use of a toothpaste with inadequate cleansing action |
| Green stain | Appears as a green or green-yellow stain, usually on the facial surfaces of the maxillary anterior teeth. Most common stain in children | Caused by poor oral hygiene when bacteria or fungi are retained in bacterial plaque |
| Dental plaque agents | Reddish-brown stain appears on the interproximal and cervical areas of the teeth. Also can appear on restorations, in plaque, and on the surface of the tongue. | Caused by the use of prescription mouth rinses that contain chlorhexidine. (Chlorhexidine is a disinfectant with broad antibacterial action.) |
| Food and drink | Light brownish stain. Stain is lessened with good oral hygiene. | Caused by tea, coffee, colas, soy sauce, berries, and other foodstuff |
From Robinson D, Bird D: Essentials of dental assisting, ed 4, Philadelphia, 2007, Saunders.
Intrinsic stains are those that are caused by an environmental source but cannot be removed because the stain has become incorporated into the structure of the tooth. Examples include tobacco stains from smoking, chewing, or dipping and stains from dental amalgam that have become incorporated into the tooth structure. The dental assistant must be able to recognize these conditions because these stains cannot be removed by polishing or scaling (Table 58-2).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses