Digital Imaging, Dental Film, and Processing Radiographs
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe the purposes and uses of digital radiography.
• List and describe the advantages and disadvantages of digital radiography.
• Explain the fundamental systems of digital radiography.
• Identify advantages and disadvantages of each digital imaging system.
• List and describe the equipment necessary for digital radiography.
• Identify the types of dental image receptors.
• Describe the composition of a dental x-ray film.
• List and identify the component parts of an automatic film processor.
• Describe common time and temperature errors during film processing.
• Describe chemical contamination errors during film processing.
• Describe film handling errors that can occur during film processing.
• Describe some common lighting errors during film processing.
• State the types of and indications for the three types of dental images.
• Identify the five basic sizes of intraoral dental film.
• Explain the purpose of an intensifying screen.
• Describe the process for duplicating radiographs.
• Describe the process for digitizing radiographs using a scanner.
• Describe the rationale for scanning and clearing phosphor plates.
Performance Outcomes
On completion of this chapter, the student will be able to meet competency standards in the following skills:
• Duplicate a set of dental radiographs.
• Process dental x-ray films with the use of a manual tank.
• Successfully process dental films using a daylight loader.
Electronic Resources
![]() Additional information related to content in Chapter 39 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 39 can be found on the companion Evolve Web site.
• The Interactive Dental Office Patient Case Studies: Miguel Ricardo, Harriet Ross, and Lee Wong
• Procedure Sequencing Exercises
• WebLinks
![]() and the Multimedia Procedures DVD
and the Multimedia Procedures DVD
Key Terms
Automatic processor Machine that automates all film processing steps.
Beam alignment device Assists in the positioning of the position indicator device (PID)
Bitewing Image view that shows the crowns of both arches on one film.
Calcium tungstate Common type of phosphor.
Cassette Contains extraoral films during exposure.
Cephalometric film Shows the bony and soft tissue areas of the facial profile.
Charge-coupled device (CCD) A solid-state image sensor used in intraoral digital imaging.
Digital image Electronic signals captured by sensors and displayed on computer monitors.
Digitized Scanning of traditional film-based radiographs into a digital image.
Duplicating film Film designed for use in film duplicating machines.
Emulsion (ee-MUL-shun) A coating on the x-ray film that contains energy-sensitive crystals.
Extraoral film Film designed for use in cassettes.
Film speed The sensitivity of the emulsion on the film to radiation.
Intensifying screen The part inside an extraoral cassette that converts x-ray energy into visible light, which in turn exposes screen film.
Intraoral film Film designed for placement in the patient’s mouth.
Label side Colored side of the film that faces the tongue.
Latent image The invisible image on the x-ray film after exposure but before processing.
Occlusal Radiographic view that shows large areas of the maxilla or mandible.
Panoramic film Used in cassettes to provide a wide view of both the upper and lower jaws.
Periapical (per-ee-AP-i-kul) Radiographic view that shows the crown, root tip, and surrounding structures.
Phosphor storage plates (PSPs) Reusable film-sized plates coated with phosphor as the image receptor.
Positioning instrument Intraoral device used to position and hold the film, sensor, or PSP.
Radiograph (RAY-dee-oe-graf) Image produced on photosensitive film by exposing the film to radiation and then processing it.
Teledentistry Process of using electronic transfer of images and other information for consultation and/or insurance purposes in dentistry.
Tube side Solid white side of the film packet that faces the x-ray tube.
In this chapter, you will learn the advantages and basic concepts of digital radiography, including scanning and digitizing dental images. You will learn the various types and uses of intraoral and extraoral images. Using conventional x-ray film, you will learn how to use manual and automatic processing techniques, and how to duplicate films. You will also learn how to recognize common errors in film processing, and how to prevent them from occurring.
Digital Radiography
Digital radiography has been used in dentistry since 1987, and it has improved tremendously during this time. Today, in many areas of the United States and Canada, dentists and dental schools are changing from conventional film-based radiography to digital radiography (Fig. 39-1).
When digital radiography is discussed, the term digital images is used instead of radiographs, x-rays, or films. The digital images are not radiographs but electronic signals that are captured by sensors and displayed on a computer monitor almost instantaneously (Fig. 39-2). These images can be emailed to insurance companies and other dentists for consultations. If desired, hard copies of these images can be printed on image-quality paper.
Although digital imaging systems are high tech, a conventional x-ray machine is still needed to expose the image, and the position of the image receptor (sensor or phosphor storage plate [PSP]) in the mouth is identical to positioning with film. In addition, strict infection control measures must be used because the sensors and PSPs are reused time and again. U.S. Food and Drug Administration (FDA)–cleared disposable, fluid-impervious barriers must be used on digital image sensors and phosphor plates. Digital image receptors are not able to tolerate heat sterilization.
Step-by-step procedures for the use of digital radiography systems vary by manufacturer. It is critical to refer to the manufacturer’s instruction booklet for information concerning operation of the system, equipment preparation, patient preparation, and exposure factors. Only general guidelines on sensor preparation and placement are discussed here.
Types of Digital Imaging Systems
Two basic methods are used to acquire a digital x-ray image: direct imaging and indirect imaging.
Direct Digital Imaging
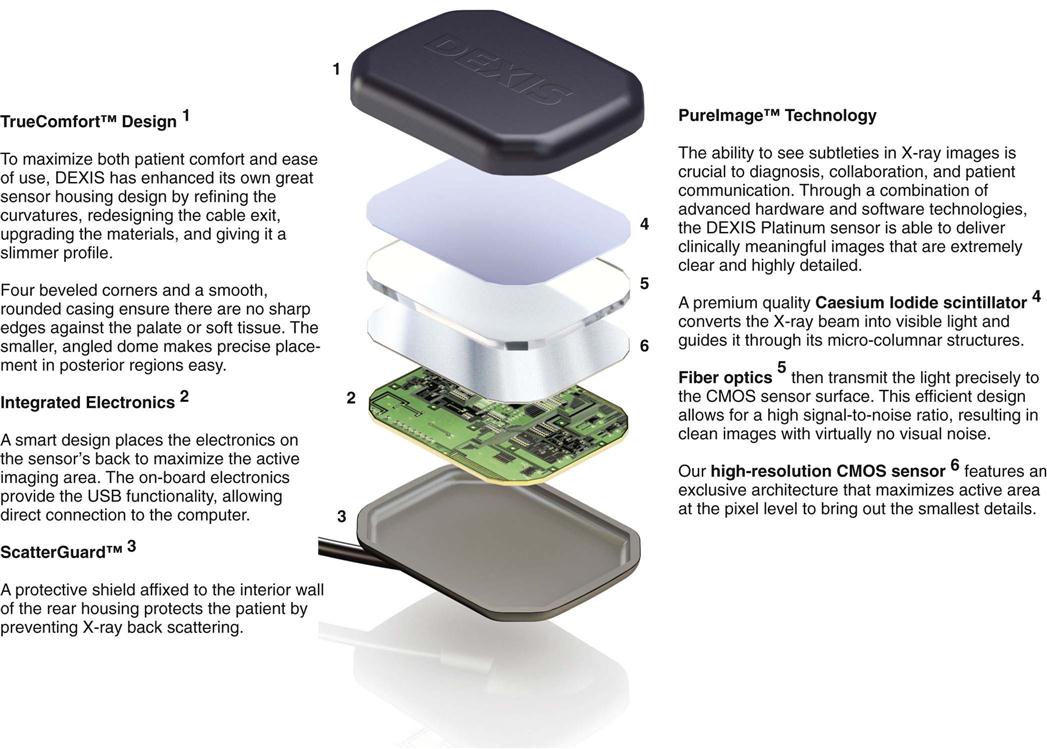
In direct imaging, a solid-state sensor is the image receptor. It contains an x-ray–sensitive silicon chip with an electronic circuit embedded in the silicon (Fig. 39-3).
The charge-coupled device (CCD) (sensor), the most commonly used digital receptor, is used in a variety of other imaging devices, such as telescopes, fax machines, personal data assistants (PDAs), video cameras, and even some panoramic machines and other extraoral imaging systems such as cone beam volumetric imaging (see Chapter 42).
Like telephones, some CCDs are wireless, and other types have a cable connected directly from the sensor to the computer. The wireless type of sensor uses radio frequency transmission to instantly transmit the image to the computer via radio waves (Fig. 39-4).
Indirect Digital Imaging
Phosphor Storage Imaging
In phosphor storage plate (PSP) imaging systems, the image receptor is a thin flexible plate, the size of a conventional x-ray film, that has been coated with phosphor crystals (Fig. 39-5). The phosphor layer is able to store the energy of the x-ray photons for some time. A scanner is required to “read” the information stored on the plate by using a laser beam to release the energy from the plate and convert it into a digital image. The latent image will remain in the phosphor plate before the scanning phase for minutes to hours, depending on the environment in which the plates are stored. They should not be exposed to bright light or warmth because this will release the energy before it is read by the scanner. After the plates are scanned, they are exposed to bright light that erases all remaining energy, and the plates are ready to be used again. For infection control, the imaging plate is inserted into a specially designed barrier envelope. The barrier envelope is sealed by removing the adhesive strip and pressing the envelope closed. The imaging plate is protected and then can be used intraorally (Fig. 39-6). The imaging plate is positioned in the patient’s mouth using the same positioning techniques as are used with conventional dental x-ray film. After exposure, the imaging plate is carefully removed from the barrier envelope and then is placed in a scanner that uses a laser to display the image on the computer.
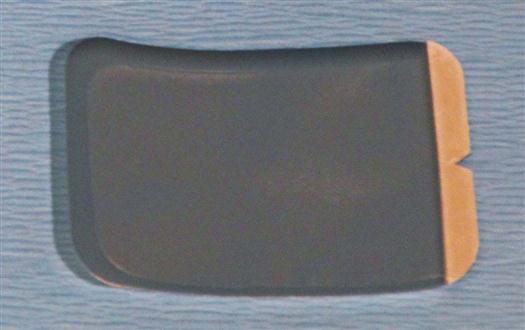

The imaging plates cannot be autoclaved, and extreme care must be taken when handling to avoid scratches or dust.
Digitizing Images
Film-based radiographs may be digitized for viewing on a computer in much the same way as any other document. Desktop scanners capture and digitize the light signal of whatever is placed inside them. This process is similar to placing a film on a duplicator lightbox (discussed later in this chapter). This type of indirect digital imaging is slightly less detailed than direct digital imaging because the resultant image is similar to a “copy” of the image versus the “original” (Fig. 39-7).
Digital Imaging Software Programs
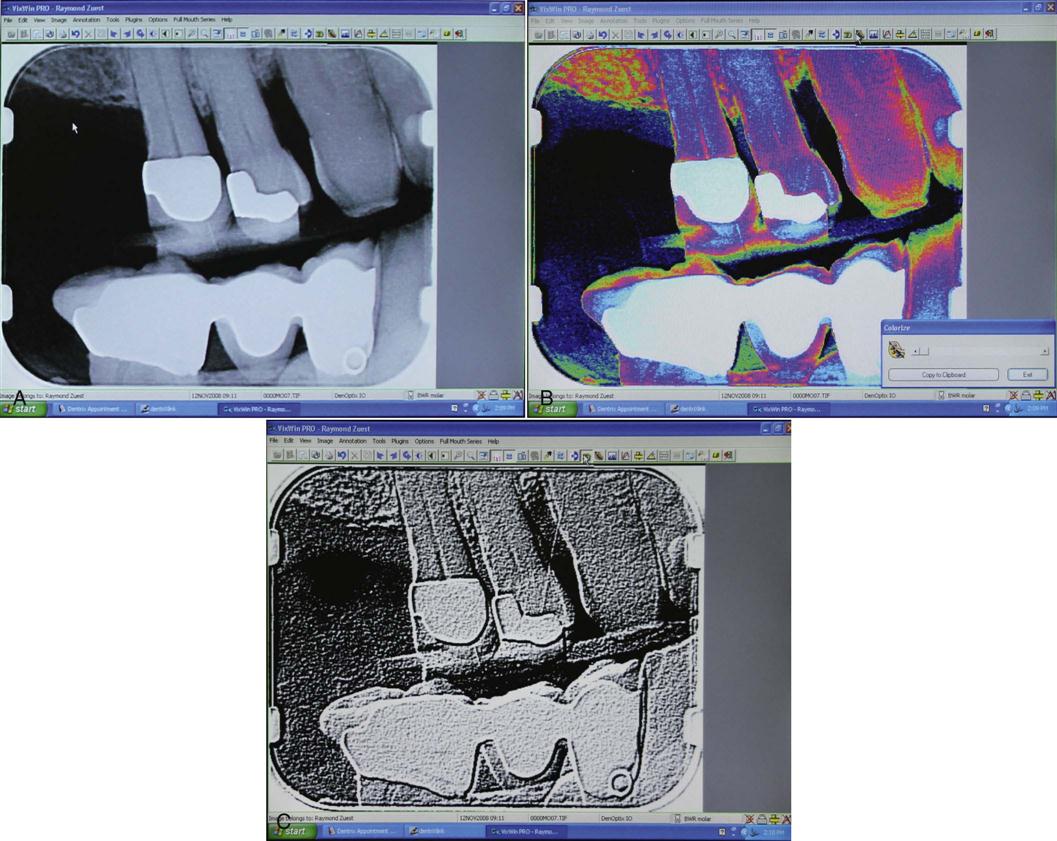
Most computer software programs that are used in digital imaging are capable of performing electronic image enhancement. This means that the operator can change the following image variables together or separately (Fig. 39-8 and Box 39-1):
X-Ray Film and Film Processing
Although many dental practices are transitioning to digital techniques, a significant number of private dental practices are using conventional film-based techniques. The dental assistant must thoroughly understand the procedures and techniques necessary to process films into high-quality diagnostic dental images. It is also important to use the correct terminology. Film is the correct term to use before it has been processed. The film is in the packet; the film is placed in the bite-block; the film is exposed and processed. After the film has been processed, it becomes an image or radiograph.
Positioning Instruments
Positioning instruments (dental film and sensor holders) are used to position and hold dental x-ray films or the digital sensor in the patient’s mouth. The use of a positioner keeps the patient’s fingers from being exposed to x-radiation. Positioners also assist the operator in properly placing the film or sensor and the position indicator device (PID). When a rectangular PID is used, a film holder is absolutely necessary to avoid cone cuts, or clear areas of the film that are not exposed to radiation (see Chapter 38).
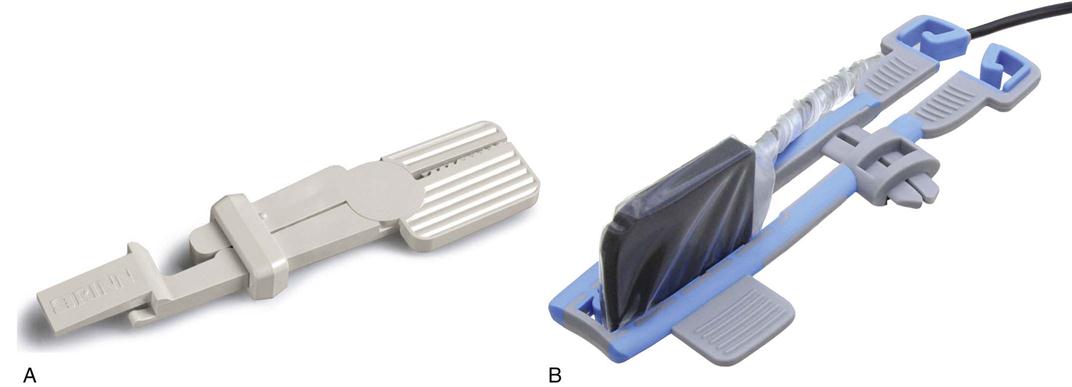
Various types of intraoral positioning instruments are currently available. The sensor holders used in digital radiography are almost identical to the x-ray film holders used in conventional techniques. The primary difference is seen in the size and shape of the holder.
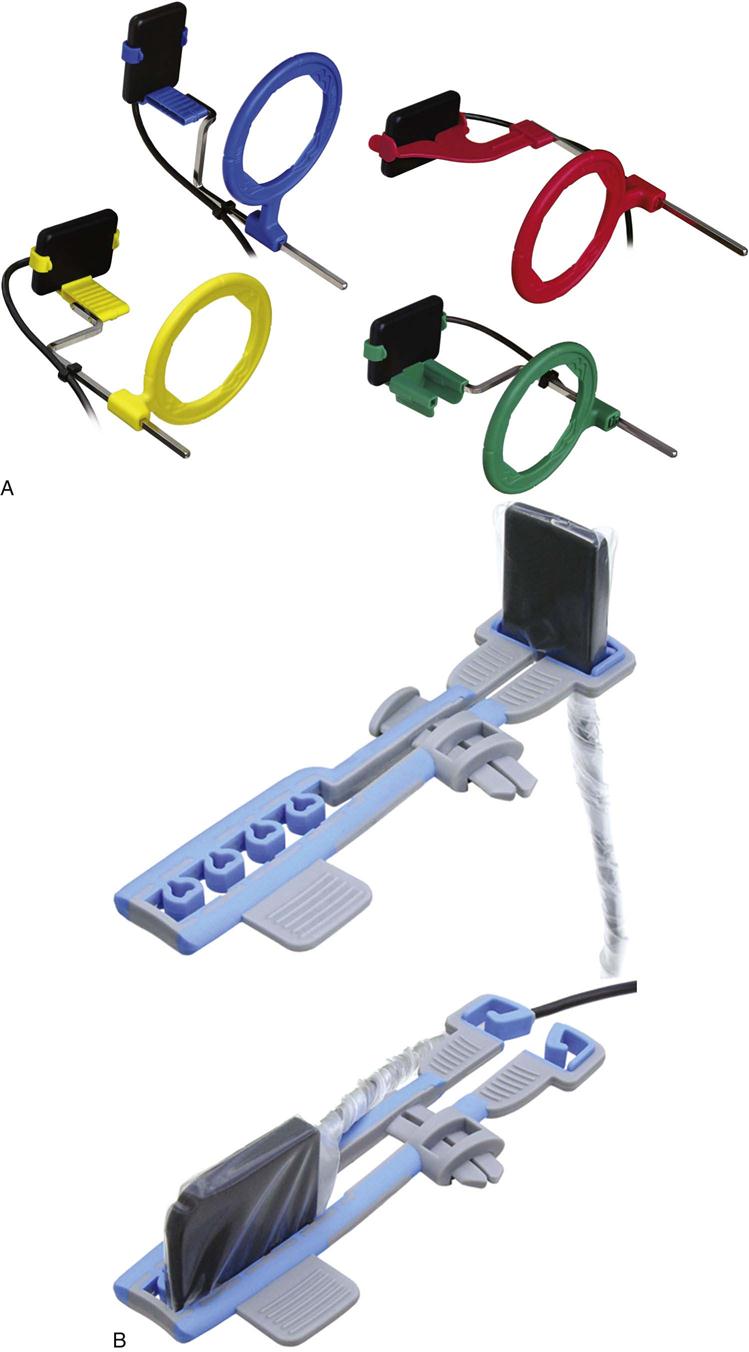
Double-ended instruments used for the bisecting technique hold the film or phosphor plate between two serrated plastic grips that can be locked into place (Fig. 39-9).
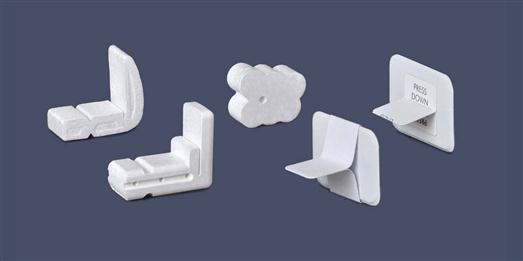
A basic style of film holder is the disposable polystyrene (Styrofoam) bite-block with a backing plate and a slot for film retention (Fig. 39-10). Other devices include the EndoRay (Dentsply International, York, Pennsylvania) (Fig. 39-11), which is used for images with endodontic instruments in the canal.
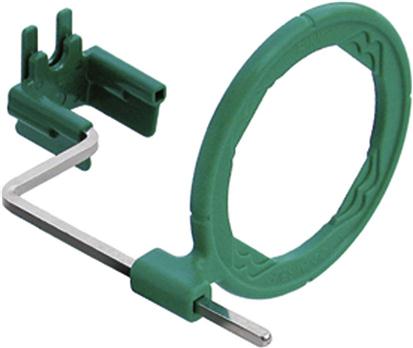
Beam Alignment Devices
Devices used to align the beam are available from several manufacturers for both film-based and digital techniques. The beam alignment device assists in positioning of the PID in relation to the tooth and film or sensor. Rinn XCP instruments (Dentsply Rinn, Elgin, Illinois) use color-coded plastic bite-blocks, plastic aiming rings, and metal indicator arms for film-based techniques, and Rinn XCP-DS are examples of instruments used for holding digital sensors. Note: Several manufacturers produce digital sensors, and the size and shape of sensors vary slightly. You must be sure that you use a digital sensor holder designed to fit the specific brand of sensor you are using (Fig. 39-12).
Dental Film
Film used in dental radiography is photographic film that has been adapted for dental use. A photographic image is produced on dental x-ray film when it is exposed to x-rays that have passed through teeth and adjacent tissues. The concept is similar to an image that is recorded on photographic film after it has been exposed to light through the shutter and lens of a camera.
The dental assistant must understand the composition of x-ray film and latent image formation. The assistant also must be familiar with the types of film used in dental radiography, as well as methods of film storage and protection.
Film Composition
Intraoral film consists of a semi-flexible acetate film base that is coated on both sides with an emulsion of silver bromide, silver halide, and silver iodide that is sensitive to radiation. Beginning with the film base, the following layers make up a />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses