CHAPTER 56
Parietal Bone Graft
Christopher J. Haggerty
Private Practice, Lakewood Oral and Maxillofacial Surgery Specialists, Lees Summit; and Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
A means of obtaining membranous bone for the reconstruction of hard tissue craniomaxillofacial defects.
Indications
- Reconstruction of the nasal dorsum in patients requiring augmentation rhinoplasty (saddle nose deformity) or naso-orbito-ethmoid (NOE) fractures (loss of bony support)
- Reconstruction of orbital wall and floor defects (correction of posttraumatic enophthalmos)
- Reconstruction of alveolar process defects prior to implant placement
- Reconstruction of craniomaxillofacial defects caused by tumor ablative surgery
- Reconstruction of alveolar clefts
- Reconstruction of skull defects or cranioplasty
Contraindications
- Harvest can be complicated in older patients due to a lack of diploe space and/or thin dura
- Anticoagulated patients
- Patients with suspected intracranial injuries
- Minimal or no diploe space identified on computed tomography (CT) or magnetic resonance imaging (MRI)
- Venous lacunae identified on CT or MRI
- Anatomical aberration identified on CT or MRI
- Less than 6 mm of parietal bone thickness
- When cancellous bone is required
Anatomy
- The superior sagittal sinus (SSS) originates anteriorly from the crista galla of the ethmoid bone and empties posteriorly into the torcular Herophili at the internal occipital protuberance.
- The superior temporal line serves as the superior attachment of the temporalis fascia. The inferior temporal line serves as the superior attachment of the temporalis muscle.
- The thickness of the parietal bone ranges from 3–12 mm.
Split-Thickness Parietal Bone Graft Harvest Procedure
- Preoperative antibiotics are administered to provide coverage for skin and scalp flora. Preoperative steroids are administered to minimize postoperative soft tissue edema.
- The patient is placed under general anesthesia and positioned supine within a Mayfield headrest. The patient is prepped and draped to include the area of parietal bone harvest and the recipient site for the graft (ie. the orbit or NOE region). A linear band of hair is either shaved or parted in the area of the proposed scalp incision. The scalp incision is marked with a sterile marking pen, and a mixture of local anesthetic with a vasoconstrictor is injected into the subgaleal plane to aid in hemostasis and for hydrodissection of the tissue.
- Exposure of the parietal bone can be achieved either with a linear incision in the location of the parietal bone or via a coronal incision. If a linear incision is utilized, the length of the incision and the extent of the exposure correlate with the amount of parietal bone to be harvested. Alternatively, a coronal incision can be utilized if additional exposure is required to areas such as the orbital rims, the dorsum of the nose, and the frontal sinus.
- Vertical dissection should proceed through the scalp layers until the pericranium is reached. Lateral dissection should begin within the subgaleal plane, preserving the attachment of the pericranium to the calvarium. The pericranium is sharply incised, reflected, and preserved dependent on the amount of parietal bone graft required and the adjunctive procedures performed.
- The graft site should be a minimum of 2 cm lateral to the midline sagittal suture and should avoid crossing other sutures (coronal, lambdoid, and squamous).
- The area of the graft is marked either with a sterile marking pen or with electrocautery. If the exact size of the defect is known, a template made of sterile foil, sterile paper, or bone wax can be used.
-
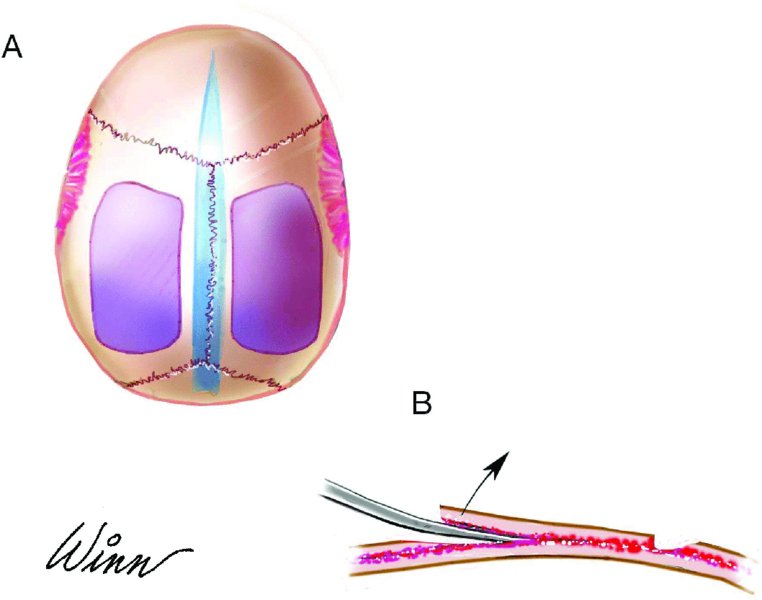
A reciprocating saw, round bur, or fissured bur is used to outline the area of the parietal bone to be harvested (Figure 56.4). The bur or saw is taken to the depth of the outer cortex until the diploe space is entered. The author prefers the use of either a round bur or a fissured bur due to the improved tactile feel once the diploe space is entered.
- Depending on the nature of the graft, the bur or saw may be used to outline numerous linear strips of calvarian bone or a single larger segment to harvest.
-
A bur is used to bevel two edges of the graft—typically, the lateral and the superior margin of the graft. The bevel will allow for the insertion of an osteotome into the diploe space. A thin spatula osteotome is initially used to enter the diploe space from a beveled edge, and then a larger curved osteotome is used to elevate the outer table (Figure 56.5). The osteotome blade should be moved sequentially along the two beveled edges of the graft site. The blade of the osteotome should be sharp, and it should be directed parallel to the diploe space (Figure 56.1B). If numerous side-by-side segments (strips) of bone are to be removed, after the removal of the initial segment, the osteotome can be laid parallel to the diploe space to facilitate additional parietal bone segment harvest (Figure 56.8).
- Once the outer table is removed, the marrow of the diploe space should be removed with a curette in order to decrease bleeding and to expose the inner table to check for fractures and cerebrospinal fluid (CSF) leakage. The site is copiously irrigated, and if bleeding persists, a thin layer of bone wax is applied to bleeding areas with a Freer elevator.
- A layer of surgicel can be placed within the outer table defect, and the incision is closed in a layered fashion. Larger graft sites or sites with non-ideal hemostasis will require drain placement.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


