Removable Prosthodontics
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Differentiate between a partial and a full denture.
• Identify indications and contraindications for removable partial and full dentures.
• List the components of a partial denture.
• List the components of a full denture.
• Describe the steps in the construction of a removable partial denture.
• Describe the steps in the construction of a full denture.
• Discuss the construction of an overdenture and an immediate denture.
• Identify home care instructions for removable partial and full dentures.
• Describe the process of relining or repairing a partial or full denture.
Performance Outcomes
On completion of this chapter, the student will be able to achieve competency standards in the following skills:
• Assist in the delivery of a partial denture.
• Assist in the try-in of the wax setup for a full denture.
Electronic Resources
![]() Additional information related to content in Chapter 52 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 52 can be found on the companion Evolve Web site.
• Interactive Dental Office Patient Case Study: Jose Escobar
• Procedure Sequencing Exercises
• WebLinks
Key Terms
Alveoplasty (al-VEE-uh-plas-tee) The surgical shaping and smoothing of the margins of the tooth socket after extraction of the tooth, generally in preparation for the placement of a prosthesis.
Border molding Process of using fingers to contour a closer adaptation of the margins of an impression while still in the mouth.
Centric (SEN-trik) relation Having the jaws in a position that produces a centrally related occlusion.
Connector Piece of metal that joins the various parts of a partial denture; also called bar.
Coping (KOEP-ing) Thin metal covering or cap placed over a prepared tooth.
Edentulous (ee-DEN-tyoo-lus) To be without teeth.
Festooning (fes-TOO-ning) The process of carving the base material of a denture or denture pattern to simulate the contours of the natural tissues.
Flange (flanj) Parts of a full or partial denture that extend from the teeth to the border of the denture.
Framework Metal skeleton of a removable partial denture.
Full denture (DEN-chur) Prosthesis that replaces all of the teeth in one arch.
Immediate denture Temporary denture placed after the extraction of anterior teeth.
Lateral excursion (ek-SKUR-zhun) Sliding the position of the mandible to the left or right of the centric position.
Mastication (mas-ti-KAY-shun) Chewing.
Occlusal (o-KLOO-sul) rim Rim built on the baseplate to register vertical dimension and occlusal relationship of the mandibular and maxillary arches.
Overdenture Full denture supported by two or more remaining natural teeth.
Partial denture Removable prosthesis that replaces teeth within the same arch.
Pressure points Specific areas in the mouth where a removable prosthesis may rub or apply more pressure.
Protrusion (proe-TROO-zhun) Position of the mandible placed forward as related to the maxilla.
Rebasing (ree-BAY-sing) Procedure to replace the entire denture base material on an existing prosthesis.
Relining (ree-LYE-ning) Procedure to resurface the tissue side of a partial or full denture so that it fits more accurately.
Resorption (ree-SORP-shun) When teeth have been extracted, the alveolar bone no longer has a purpose, and the body will resorb it.
Rest Metal projection on or near the retainer of a partial denture.
Retainer (ree-TAY-nur) Device used to hold attachments and abutments of a removable prosthesis in place.
Retrusion (ree-TROO-zhun) Position of the mandible posterior from the centric position as related to the maxilla.
Template (TEM-plut) Clear plastic tray that represents the alveolus as it should appear after teeth have been extracted.
Tuberosity (too-buh-ROS-i-tee) Rounded bony protrusion behind your last molar in the maxilla.
Removable prosthodontics is the dental specialty in which missing teeth are replaced with a prosthesis that the patient can place in and take out of the mouth freely. Two major types of removable prosthetics are available:
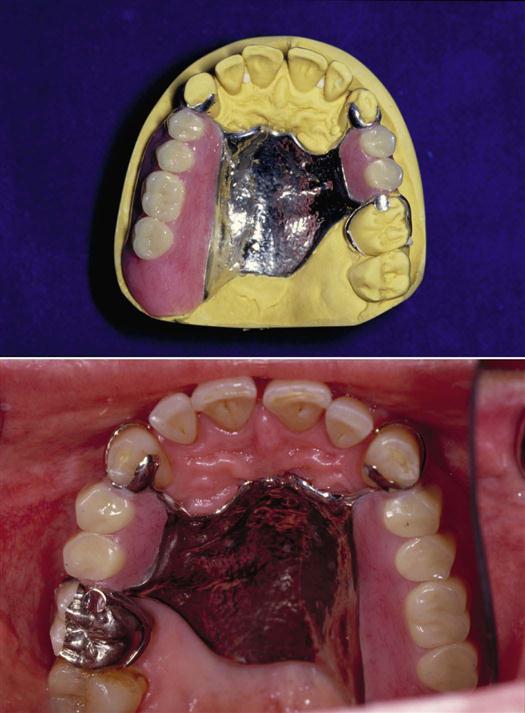
• Removable partial denture, also referred to as a partial, replaces one or more teeth in the same arch (Fig. 52-1).
• Removable full denture, also referred to as a denture, replaces all the teeth in one arch (Fig. 52-2).
Factors Influencing the Choice of a Removable Prosthesis
The dentist must advise patients who are considering a removable prosthesis that it will never function as well as the natural dentition that is being replaced, regardless of how well it is constructed and fits. The dentist considers the following extraoral and intraoral factors before recommending this treatment plan for a patient.
Extraoral Factors
Although extraoral factors are usually beyond the control of the dentist, they cannot be ignored. These factors include the patient’s physical and mental health, motivation, age, occupation, and dietary habits, as well as social and economic factors.
Physical Health
Certain physical conditions, such as diabetes, affect the ability of the tissues to tolerate the pressure of a removable prosthesis. Also, the patient who is in poor health may be unable to cope during the fabrication of a new prosthesis or unable to adapt to wearing it.
Mental Health
Individuals with poor mental health may be irritated by and overly concerned about the denture in their mouth. Patients with severe mental disability or mental decline may not be able to keep the appliance in place or maintain adequate oral hygiene.
Patient Motivation
Occasionally, a patient’s major motive for having teeth extracted and replaced with a prosthesis is for esthetic reasons, that is, only to improve their appearance. The dentist should explore all acceptable alternative treatment options before giving serious consideration to the request.
Age
A prosthesis for a young person must be designed to allow for growth and accommodate for new teeth as they erupt. If the patient is very active or plays contact sports, the strength of the appliance is also an important factor.
A different challenge is found in the attitude of an older patient who associates the loss of teeth with aging and has an unrealistic desire to retain teeth that are structurally unsound.
Dietary Habits
Healthy tissue is an important aspect of removable prosthodontic success. Patients with poor nutritional habits may have poor tissue response to the prosthesis, which could affect the overall tolerance and comfort of the prosthesis.
Social and Economic Factors
How important is it to the patient to replace lost teeth? Patients’ attitudes about their oral health and appearance will help them decide if dentures are important or not.
The ability to pay for the treatment is a major economic factor. You can actually find “denture clinics” or “mail order clinics,” which cater specifically to the lower economic population by providing a quick, low-cost method of obtaining a denture.
Occupation
Patients whose daily activities involve “meeting the public” are concerned about the possible change in their appearance during or after the transition to partial or full dentures. Appointments for surgery and the delivery of the prosthesis should be scheduled without serious disruption to the patient’s social and occupational activities.
Intraoral Factors
The condition of the tissues in the patient’s mouth is a key factor in determining whether a removable partial or a complete denture can be recommended.
Musculature
Facial muscles contribute to retention and functional control of the prosthesis. Strong muscle attachments with good muscle tone are important. On the contrary, a large or very active tongue may cause difficulty in retention and wearing of the prosthesis. A patient with a nervous, unusual facial habit may have difficulty retaining and adjusting to a prosthesis.
Salivary Flow
The presence of something foreign, such as a prosthesis, in the oral cavity may stimulate an excessive flow of saliva. This response usually diminishes and is controlled as the patient becomes accustomed to wearing the prosthesis. However, the prosthesis may make saliva control more difficult to deal with in patients with paralysis of the facial muscles caused by a stroke.
In contrast, a patient with a lack of saliva may find it very difficult to wear a prosthesis and may be very uncomfortable. Physical conditions, medications, or radiation treatment may be the cause of inadequate salivary flow.
Residual Alveolar Ridge
Successful wearing of a removable prosthesis depends mainly on the support provided by the alveolar ridge. If it is at normal height and is evenly contoured, the alveolar ridge should provide good support, allowing for an even distribution for the stress of mastication. If the alveolar ridge has resorbed anywhere within the ridge, this can result in a sore spot for the patient. Resorption occurs when the alveolar ridge has resorbed, causing an uneven distribution of pressure of the prosthesis, which keeps it from fitting properly.
In some cases, it is necessary for the surgeon to perform an alveoplasty to recontour the alveolar ridge surgically to minimize such problems (see Chapter 56). It is a normal ongoing process for the alveolar ridge to continue to decrease in size and shape after teeth are lost. A well-fitted prosthesis minimizes these changes; a poorly fitting prosthesis accelerates the process. Because of these changes, it is important that the patient return periodically for an oral examination and for reevaluation of the fit of the prosthesis.
Oral Mucosa
When the mucosa that covers the residual ridge is altered by the patient’s physical condition, the prosthesis may cause friction and irritation and be difficult for the patient to wear. Likewise, a poorly fitting prosthesis may cause irritation and sore spots, known as pressure points, on the oral mucosa. Patients should be seen promptly so the dentist can relieve these sore spots.
Oral Habits
Oral habits such as clenching or grinding can cause extreme stress on the ridges and remaining teeth, which must be taken into account when selecting a removable prosthesis. Mouth breathing may affect the patient’s ability to hold the appliance in place.
Tori
Tori are abnormal growths of bone in a specific area. Mandibular or maxillary tori, when present, can affect the patient’s ability to wear a prosthesis in that arch (see Chapter 17). Depending on the type of prosthesis, it may be necessary to have the tori surgically removed before fabrication of the appliance is begun.
Removable Partial Denture
A removable partial denture receives its support and retention from the underlying tissues and remaining teeth that serve as abutments. This type of prosthesis is designed to distribute the forces of mastication between these abutments and the supporting tissues (Box 52-1).
Components of a Partial Denture
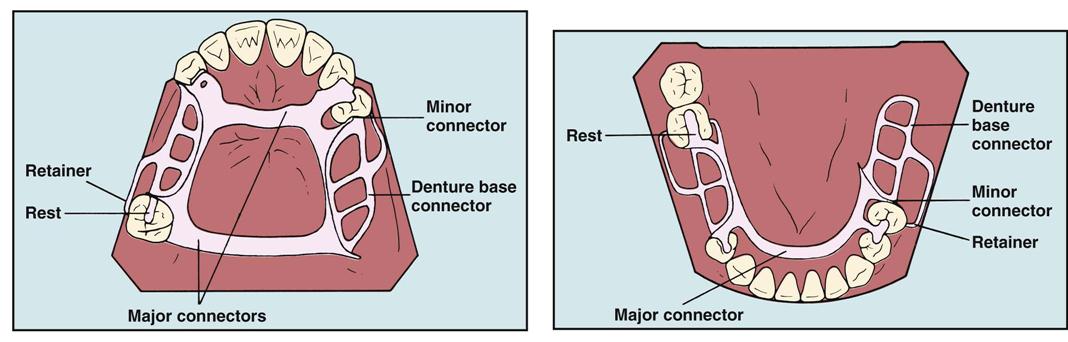
The basic components of a removable partial denture are the framework, connectors, denture base, retainers, rests, and artificial teeth (Fig. 52-3).
Framework
The framework is the cast metal skeleton that provides support for the remaining components of the prosthesis. The dental laboratory technician constructs this meshlike portion of the partial denture to cover the framework with acrylic resin to mirror the appearance of gingiva.
Connectors
The connectors, or bars, join together the various parts of the partial denture. The major connector is the piece of rigid metal that joins the right-and-left-quadrant framework of the partial denture. This connector also helps to provide support for the remaining teeth, so the stress is evenly distributed. A maxillary partial denture will have a palatal connector, and the mandibular partial denture will have a lingual connector.
A stress breaker is a metal device built into a partial denture design to protect the abutment teeth from excessive occlusal loads and stress during mastication. A stress breaker is advised for abutment teeth that have limited support in the alveolar ridge.
The minor connector links the major connector to the base and other areas, such as rests and clasps.
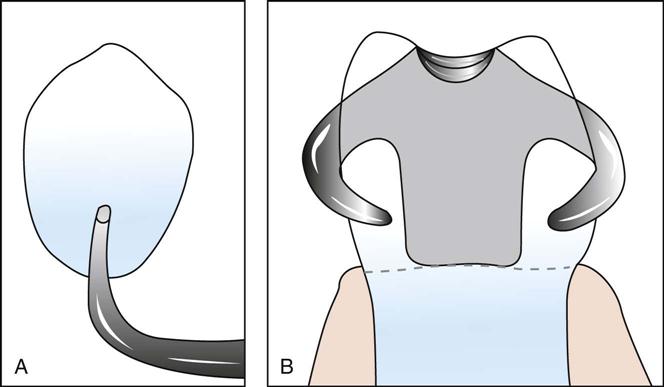
Retainer
A retainer, also known as a clasp, is the portion of the framework that directly supports and provides stability to the partial denture by partially encircling or resting on an abutment tooth.
The I-bar retainer, or I-bar clasp, approaches the tooth in a straight line from the apical direction and extends upward against the tooth (Fig. 52-4, A). A circumferential retainer, or C-clasp, originates at the occlusal surface of the tooth and extends downward, so that it partially encircles the tooth (Fig. 52-4, B).
Rest
A rest is a metal projection designed to control the seating of a prosthesis as it is positioned in the mouth. Rests prevent the partial denture from moving in a gingival direction, which would place abnormal stress and wear on the abutment tooth. The rest also aids in distributing the retention load of the partial denture to several teeth, not just to a single tooth. It also prevents passage of food between the abutment tooth and the retainer.
Rests are designed to lay within a prepared recess on the occlusal or lingual surface of a tooth. If a cast restoration is in place on the abutment tooth, the rest is positioned to protect the tooth structure against wear. Although the rest fits into the casting, it is not attached to it. Two common types of rests are available as follows:
Artificial Teeth
Artificial teeth can be constructed from acrylic or porcelain (Fig. 52-5). Acrylic teeth are selected more often because they do not produce a clicking sound during chewing; however, acrylic teeth tend to wear faster and are more susceptible to staining. Porcelain te/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses