CHAPTER 50
Neck Pathology
Anil N. Shah1 and Matthew T. Brigger2
1Department of Otolaryngology—Head and Neck Surgery, Naval Medical Center San Diego, and San Diego, California, USA
2Department of Otolaryngology—Head and Neck Surgery, Naval Medical Center San Diego; and Uniformed Services of the Health Sciences University, San Diego, California USA
Midline Neck Pathology
Differential Diagnosis
- Thyroglossal duct cyst (TGDC)
- Dermoid or epidermoid cyst
- Lipoma
- Submental lymphadenopathy
- Thyroid masses or goiter
- Vascular malformations (hemangioma)
- Teratoma
- Ectopic thyroid (lingual thyroid)
Procedure: Excision of Midline Neck Mass
A midline neck mass, prior to excision, must be differentiated from a thyroid gland mass and normal thyroid tissue should be confirmed, generally through imaging, to ensure that excision will not result in complete removal of functioning thyroid tissue from an ectopic location. Standard imaging modalities include ultrasound, computed tomography (CT) scan, and magnetic resonance imaging (MRI). Fine-needle aspirate (FNA) cytology is recommended prior to an open biopsy of midline and lateral neck masses.
Indications
- Excisional biopsy to determine the diagnosis when prior cytologic evaluation was nondiagnostic
- Aesthetic correction of biopsy proven benign mass within the neck (i.e., lipoma)
- Prior history of infection within the anterior neck
- Relative risk of malignancy originating in a thyroglossal duct cyst
Contraindication
- Acute infection or inflammation at the surgical site (relative contraindication)
Anatomy
The thyroid anlage originates as a thickening of cells at the foramen cecum, which is located on the dorsum of the tongue posteriorly at the apex of the V-shaped sulcus formed by the circumvallate papillae. Fusion of the second branchial arch anlage in the midline may result in entrapment of the thyroglossal duct by the hyoid bone.
Neck layers:
- Skin
- Subcutaneous tissue
- Platysma muscle
- Superficial (investing) layer of deep cervical fascia
- Midline linea alba with laterally located strap muscles
- Middle (pretracheal) layer of the deep cervical fascia
- Pretracheal space, which contains the thyroglossal duct cyst
Sistrunk Procedure for Thyroglossal Duct Cyst (TGDC) Excision
- Preoperative antibiotics are administered. Short-acting paralytics are utilized to allow for facial nerve testing. The patient is intubated with the endotracheal tube directed cephalically or toward the contralateral side of the mass.
- The patient is placed in cervical extension using a shoulder roll. Prominent landmarks (midline mandible, hyoid bone, and thyroid and cricoid cartilage) are marked using a sterile marking pen.
- A transverse incision is marked in the midline in a skin crease within the upper part of the neck overlying the mass. If there is evidence of a draining sinus, then an elliptical incision should be made to include the involved skin.
- The marked incision is injected with 1% lidocaine with 1:100,000 epinephrine within the subdermis just superficial to the platysma.
- The patient is prepped and draped from the mandible to a point several centimeters below the sternal notch. Use of a split drape will allow for manual palpation of the base of tongue through the mouth during the final stages of the dissection if needed.
- The initial incision is made with a #15 blade through skin, dermis, and subcutaneous fat. Once the platysma is identified, dissection proceeds through the platysma layer, and superior and inferior subplatysmal flaps are elevated. Of note, the platysma is often deficient in the immediate midline in the region of the midline raphe. It is more important to elevate the superior flap due to the course of dissection compared to the inferior flap. Deep to the platysma are the right and left anterior jugular veins, which can either be ligated or elevated within the superior subplatysmal flap.
- Once the strap muscles are identified, they are retracted laterally at the midline raphe without division. However, a portion of the sternohyoid, at the level of the hyoid, may have to be excised with the specimen depending on the proximity of the walls of the cyst to the strap muscles.
- The mass (Figure 50.1) is dissected free from the surrounding strap musculature, thyroid cartilage, and thyrohyoid membrane using a combination of blunt and sharp dissection up to the hyoid bone. It is absolutely critical to identify and confirm the location of the thyroid notch and cartilage prior to making cuts within the hyoid bone. This will prevent inadvertent damage to the thyroid cartilage, which is in close proximity to the hyoid bone in the pediatric population.
- The muscles, soft tissue, and periosteum are dissected off of the hyoid bone on both sides in order to remove the middle one-third of the hyoid bone with the specimen. Bone-cutting ronguers or heavy scissors should be used to cut the hyoid bone.
- As the hyoid bone is elevated anteriorly, dissection can proceed up to the base of tongue, and an ellipse of tissue is taken with the specimen. Placing a new glove on the surgeon’s hand will allow manual palpation of the base of tongue and position the foramen cecum into the dissection plane.
- A 2-0 silk ligature is used at the deep aspect of the dissection upon removal of the mass to induce scarring within the wound bed and to ensure closure of any remaining duct remnant (Figure 50.2).
- If the vallecula or oropharynx is entered, the defect should be closed with interrupted non-absorbable sutures through the transcervical incision.
- The wound bed should be copiously irrigated and inspected for signs of hemorrhage. A passive drain is placed in most cases, although some cases may require active drainage.
- The wound is closed in a layered fashion with 3-0 Vicryl sutures for the deep fascia, 4-0 Vicryl for the superficial fascia and deep dermis, followed by a running 5-0 Monocryl subcuticular skin closure.
- The skin incision is covered with a thin layer of antibiotic ointment, and a light pressure dressing (i.e., fluffed gauze and tegaderm) is applied.

Figure 50.1. Surgical exposure of a thyroglossal duct cyst.
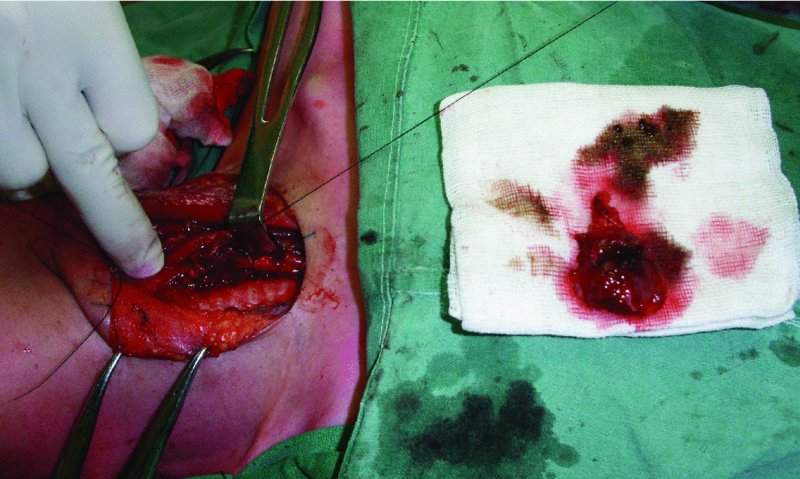
Figure 50.2. A silk ligature is used along the deep aspect of the dissection after removal of the mass to induce scarring within the wound bed, as well as to ensure closure of any remaining duct remnants.
Postoperative Management
- Patients are given intravenous (inpatient) and oral (outpatient) antibiotics for 5 days postoperatively.
- Analgesics are prescribed.
- Drains are typically removed after 48 hours or when nonproductive.
- Follow-up is based on the nature of the mass excised.
Complications
- Recurrence of TGDC: Minimized with resection of the midline portion of the hyoid bone with a Sistrunk procedure. A history of a prior infection increases the risk of recurrence, especially infections within 6 months of definitive treatment and requiring incision and drainage. Recurrence is likely after re-excision and may be due to the presence of accessory ducts and diverticula from the main duct and pharyngeal mucosa that was not removed at the initial surgery. Re-excision should be performed with wide dissection of a generous core of muscle between the superior aspect of the hyoid bone and the base of the tongue as well as an additional portion of the hyoid bone.
- Iatrogenic hypothyroidism: Secondary to removal of functional thyroid tissue within the thyroglossal duct cyst. Preoperative imaging should be performed to verify the presence of a descended thyroid gland.
- Nerve injury: Injury to the hypoglossal and superior laryngeal nerves may oc/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


