Marginal chronic periodontitis
Similar to gingivitis, mild chronic periodontitis is induced by bacterial plaque; it is defined as gingival inflammation associated with clinical attachment loss less than one third of the root length. In the molar region, furcation invasion does not exceed Class I. Treatment is the same as that for gingivitis. After treatment, residual pockets and attachment loss are less than 4 mm, and as a general rule, surgical treatment is not necessary.
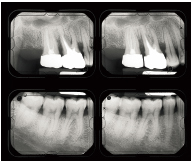
Marginal chronic periodontitis (pockets less than 4 mm) can usually be managed by scaling and root planing in a single treatment phase (Figs 5-1a and 5-1b).
Fig 5-1b Periodontal therapy consists of oral hygiene instructions followed by two scaling and then two root planing sessions. Swift response to treatment occurs, with complete reversal of inflammation. There is a slight gingival recession, along with papillae tissue loss. As a general rule, surgery is not necessary; it may, however, be indicated when bony defects are present or to improve gingival conditions before prosthetic care.
Moderate to locally advanced chronic periodontitis
Moderate chronic periodontitis (once known as adult periodontitis) is the most common form of periodontitis. It occurs in all age groups. It is characterized by a slow progression with intermittent periods of rapid progression (American Academy of Periodontology 2000).
Clinical signs and symptoms
• Swelling, redness, and bleeding on probing are present, with or without suppuration.
• Chronic periodontitis is qualified as moderate when loss of periodontal attachment is greater than or equal to one third of the root length. Probing depth may reach 6 mm and clinical attachment loss 4 mm. Increased mobility is often observed. In the furcae, attachment loss does not exceed Class I.
• Radiographic evaluation displays evidence of bone loss.
• Moderate chronic periodontitis may be localized to one tooth, extend to several teeth, or be generalized to all quadrants. Simultaneously in a given patient, there may be healthy areas and other areas featuring chronic periodontitis with slight, moderate, or severe levels of destruction.
Treatment goals
Treatment goals involve controlling or eliminating microbial factors altogether, as well as modifying risk factors to arrest disease progression durably. Periodontal health and functional and esthetic comfort must subsequently be maintained and recurrence prevented. Commensal infection is preponderant. Therefore, local treatment is the priority since it reduces bacterial load and may promote a bacterial equilibrium that is compatible with periodontal health. The reduction of inflammatory signs is a hallmark for these microbiologic changes. Locally, an attempt at regenerating the attachment system may be made.
Several different factors may affect treatment planning and the general outcome: some are patient-related and include general health status, age, motivation, cooperation, and plaque-control proficiency. Other factors include the clinician’s ability to eliminate subgingival deposits, the need for dental and prosthetic work, and the presence of sites with severe periodontal destruction.
Conventional treatment
Initial treatment (etiologic)
• Systemic risk factors (diabetes, systemic disease), behavior-related risk factors (smoking), environment-related risk factors (stress), or bacterial risk factors (presence of virulent pathogenic species) are likely to compromise success of conventional treatment. These factors should be properly controlled or eliminated when possible.
• Oral hygiene instructions, improvement, and assessment of plaque control.
• Supra- and subgingival scaling and root planing.
• Eventually, administration of antimicrobial agents (antibiotics and antiseptics).
• Elimination or correction of local, iatrogenic, or functional risk factors.
• Assessment of initial treatment phase outcome. This involves screening through all disease markers. An appropriate time interval should be respected, to allow for tissue repair and a reduction of inflammation to occur. Three different possibilities should be anticipated:
– Outcome is unsatisfactory because of poor plaque control. Chances for treatment success are slim to none.
– Outcome is satisfactory as far as inflammation is concerned, but the conditions necessary to achieve stable periodontal health have not been established. Adjunct treatment should be considered (surgery or other).
Periodontal surgery
• Periodontal augmentation surgery
• Corrective surgery
– Flap surgery with or without ostectomy
– Prosthetic surgical preparation prior to prosthetic rehabilitation
• Reparative surgery
– Bone grafts
– Guided tissue regeneration
– Combined techniques
Other treatments
• Resume some aspects of initial therapy
• Correct other risk factors (cessation of smoking, systemic disease management)
• Establish a periodontal maintenance schedule
Conditions required for therapeutic success
The predictable effects of a successful conventional treatment for mild or moderate chronic periodontitis are:
• A decrease in plaque to a level compatible with gingival health
• A significant reduction of all clinical signs of inflammation
• Pocket depth reduction
• Stability or, at best, clinical attachment gain
In areas where tissue response is poor, the following items may be observed:
• Persistence of residual inflamed gingival tissue
• Persistence or increase in pocket depth for deep pockets
• Unstable clinical attachment levels
• Persistent plaque rates to a degree incompatible with gingival health
Frequently, localized areas display persistent signs of instability, though the general periodontal context displays overall improvement of disease markers. In these cases, specific adjunct therapy should be considered.
Case report of moderate chronic periodontitis with locally advanced sites
Forty-one-year-old, otherwise healthy, nonsmoking female patient, brushes twice a day and uses toothpicks. Family history reveals that the patient’s mother was edentulous at age 45 (Figs 5-2a to 5-2bb).
Chief complaints
Tooth mobility, pain on chewing in maxillary incisors and right first molar; long history of bleeding gingiva.
Clinical signs
Halitosis, inflammation (most prominent in lingual/palatal aspects of all quadrants), bacterial plaque, calculus, attachment loss (generally 4 to 6 mm, locally 8 to 10 mm), pockets, dental mobility (Class II to IV), secondary diastemata, bone loss from one third to two thirds of the root length, furcation invasion and presence of angular lesions, primary anterior overbite, absence of canine guidance, improperly fitting restorations, molar occlusal trauma, lingual hyperfunction.
Severity
Moderate to severe; attachment losses frequently exceed 6 mm.
Complexity factors
These are essentially local factors, such as plaque, restorations, functional occlusal disorder, and overload. Destruction is linked to the presence of these local factors.
Diagnosis
Moderate to severe chronic periodontitis featuring a predominant endogenous-type infection, caused by growth of a selected number of commensal anaerobic populations, and aggravated by numerous local factors.
Treatment goals and methods
The chief objective is to control infection and to eliminate inflammation; this is achieved through proper plaque control, placement of provisional restorations, and scaling and root planing. Progressive reduction or disappearance of inflammation indicates a favorable evolution in treatment; inflammatory signs (swelling, redness, bleeding) are reversible, while those related to destruction (horizontal bone loss) are not. Some improvement (attachment gains, reduction of probing depths, dental mobility, migration) is nevertheless likely to occur.
Periodontal treatment generally leads to reduction or correction of dental displacement, occasionally without further indication for orthodontic therapy. Orthodontic treatment, if initiated too early, may render assessment of the response potential difficult.
Restorative periodontal strategies aim at eliminating complexity factors (ill-fitting restorations) and risk factors (pockets).
It seems unlikely in this clinical case that a course of antibiotic therapy will be necessary.
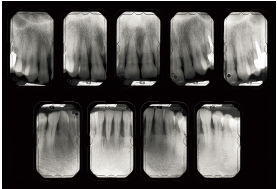
Fig 5-2c Bone destruction is irregularly distributed. In some places, it reaches 50%.
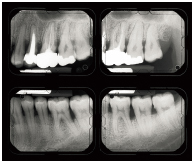
Fig 5-2d Here again, bone destruction is more advanced in restored teeth (maxillary left second premolar, first molar, and second molar). Mandibular teeth present less bone destruction. Severity factors are local and functional in nature.
Risk factors
Bacterial plaque, a possible predisposition to periodontal disease, and presence of persistent periodontal pockets are a few of the risk factors.
Recurrent subgingival bacterial colonization increases the likelihood of disease progression. This risk is directly proportional to the patient’s ability to effectively control the accumulation of plaque, as well as to the persistence of high-risk sites, including deep pockets, furcation invasions, and mobile teeth.
Prognosis
Good.

Fig 5-2f Attachment loss around the first molar exceeds 10 mm and involves the furcation. The tooth presents Class III mobility. The tooth is very tender to percussion.

Fig 5-2g Significant amounts of plaque deposit are visible on the palatal aspect of the maxillary right central incisor. This evokes the characteristic aspect of plaque biofilm. Opposite the root surface, gingival recession has occurred concomitantly to intense inflammation. The maxillary right central incisor exhibits Class III or higher mobility. Attachment loss exceeds 10 mm on the distal aspect. Interincisal diastema is of recent onset (6 months).
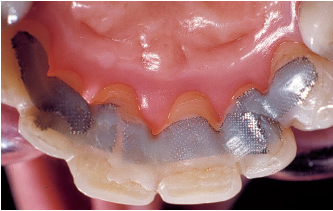
Fig 5-2h After two scaling sessions, two planing sessions, periodontal surgery, and orthodontic treatment, inflammation has disappeared and attachment gain has occurred around the incisors. Transitional splinting is performed on all six anterior teeth.

Fig 5-2j An infectious incident occurs after root planing. The bacterial balance is modified. The elimination of residual beneficial species promotes tissue invasion by residual pathogens. Note the quick closure of the diastema subsequent to an inflammatory episode: a change in inflammatory status may artificially reduce secondary migrations.

Fig 5-2k Antibiotic treatment is necessary (amoxicillin 500 mg tid for 8 days and metronidazole 500 mg tid for 8 days). Periodontal flap surgery is performed. Orthodontic treatment is performed to reverse residual diastemata and restore canine guidance.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses