Chapter 5 Prosthetic Options in Implant Dentistry
Implant dentistry is similar to all aspects of medicine in that treatment begins with a diagnosis of the patient’s condition. Many treatment options stem from the diagnostic information. Traditional dentistry provides limited treatment options for the edentulous patient. Because the dentist cannot add abutments, the restoration design is directly related to the existing oral condition. On the other hand, implant dentistry can provide a range of additional abutment locations. Bone augmentation may further modify the existing edentulous condition in both the partial and total edentulous arch and therefore also affects the final prosthetic design. As a result, a number of treatment options are available to most partially and completely edentulous patients. Therefore, once the diagnosis is complete, the implant treatment plan of choice at a particular moment is patient and problem based. Not all patients should be treated with the same restoration type or design.
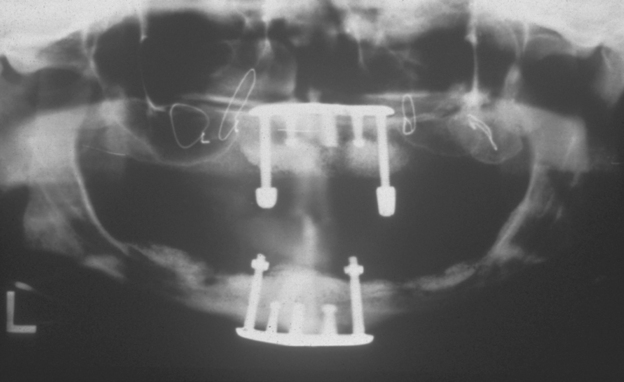
The goals of implant dentistry are to replace a patient’s missing teeth to normal contour, comfort, function, esthetics, speech, and health, regardless of the previous atrophy, disease, or injury of the stomatognathic system. It is the final restoration, not the implants, that accomplish these goals. In other words, patients are missing teeth, not implants. To satisfy predictably a patient’s needs and desires, the prosthesis should first be designed. In the stress treatment theorem,1 the final restoration is first planned, similar to the architect designing a building before making the foundation. Only after this is accomplished can the abutments necessary to support the specific predetermined restoration be designed (Figure 5-1).
COMPLETELY EDENTULOUS PROSTHESIS DESIGN
An axiom of implant treatment is to provide the most predictable, most cost-effective treatment that will satisfy the patient’s anatomical needs and personal desires. In the completely edentulous patient, a removable implant-supported prosthesis offers several advantages over a fixed-implant restoration (Box 5-1).
Box 5-1 Advantages of Removable Implant-Supported Prostheses in the Completely Edentulous Patient
However, some completely edentulous patients require a fixed restoration because of desire or because their oral condition makes the fabrication of teeth difficult if a superstructure and removable prosthesis are planned. For example, when the patient has abundant bone and implants have already been placed, the lack of crown height space may not permit a removable prosthesis.2
Too often, treatment plans for completely edentulous patients consist of a maxillary denture and a mandibular overdenture with two implants. However, in the long term, this treatment option may prove a disservice to the patient. The maxillary arch will continue to lose bone, and the bone loss may even be accelerated in the premaxilla.3,4 Once this dimension is lost, the patient will have much more difficulty with retention and stability of the restoration. In addition, the lack of posterior implant support in the mandible will allow posterior bone loss to continue.5 Paresthesia, facial changes, and reduced posterior occlusion on the maxillary prosthesis are to be expected. The doctor should diagnose the amount of bone loss and its consequences on facial esthetics, function, and the psychological and overall health. Patients should be made aware of future compromises in bone loss and its associated problems with minimal treatment options, which do not address the continued loss of bone in regions where implants are not inserted.
The completely implant-supported overdenture requires the same number of implants as a fixed-implant restoration. Thus the cost of implant surgery may be similar for fixed or removable restorations. Fixed prostheses often last longer than overdentures, because attachments do not require replacement and acrylic denture teeth wear faster than porcelain to metal.6 The chance of food entrapment under a removable overdenture is often greater than for a fixed restoration, as soft tissue extensions and support are often required in the latter. The laboratory fees for a fixed prosthesis may be similar to a bar, coping attachments, and overdenture. Because the denture or partial denture fees are much less than fixed prostheses, many clinicians charge the patient a much lower fee for removable overdentures on implants. Yet chair time and laboratory fees are often similar for fixed or removable restorations that are completely implant supported. One should consider increasing the patient fees for overdentures to a level more in line with fixed restorations.
PARTIALLY EDENTULOUS PROSTHESIS DESIGN
A common axiom in traditional prosthodontics for partial edentulism is to provide a fixed partial denture whenever applicable.7,8 The fewer natural teeth missing, the better the indication for a fixed partial denture. This axiom also applies to implant prostheses in the partially edentulous patient. Ideally, the fixed partial denture is completely implant supported rather than joining implants to teeth. This concept leads to the use of more implants in the treatment plan. Although this may be a cost disadvantage, it is outweighed by significant intraoral health benefits. The added implants in the edentulous site result in fewer pontics, more retentive units in the restoration, and less stress to the supporting bone. As a result, complications are minimized and implant and prosthesis longevity are increased (Box 5-2).
PROSTHETIC OPTIONS
In 1989, Misch proposed five prosthetic options for implant dentistry9,10 (Table 5-1). The first three options are fixed prostheses (FPs). These three options may replace partial (one tooth or several) or total dentitions and may be cemented or screw retained. They are used to communicate the appearance of the final prosthesis to all the implant team members. These options depend on the amount of hard and soft tissue structures replaced and the aspects of the prosthesis in the esthetic zone. Common to all fixed options is the inability of the patient to remove the prosthesis. Two types of final implant restorations are removable prostheses (RPs); they depend on the amount of implant support, not the appearance of the prosthesis.
| TYPE | DEFINITION |
|---|---|
| FP-1 | Fixed prosthesis; replaces only the crown; looks like a natural tooth |
| FP-2 | Fixed prosthesis; replaces the crown and a portion of the root; crown contour appears normal in the occlusal half but is elongated or hypercontoured in the gingival half |
| FP-3 | Fixed prosthesis; replaces missing crowns and gingival color and portion of the edentulous site; prosthesis most often uses denture teeth and acrylic gingiva, but may be porcelain to metal |
| RP-4 | Removable prosthesis; overdenture supported completely by implant |
| RP-5 | Removable prosthesis; overdenture supported by both soft tissue and implant |
From Misch CE: Bone classification training keys, Dent Today 8:39-44, 1989.
Fixed Prostheses
FP-1
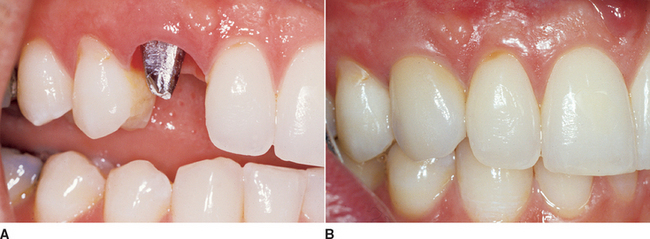
An FP-1 is a fixed restoration and appears to the patient to replace only the anatomical crowns of the missing natural teeth. To fabricate this restoration type, there must be minimal loss of hard and soft tissues. The volume and position of the residual bone must permit ideal placement of the implant in a location similar to the root of a natural tooth. The final restoration appears very similar in size and contour to most traditional fixed prostheses used to restore or replace natural crowns of teeth (Figure 5-2).
The FP-1 prosthesis is most often desired in the maxillary anterior region, especially in the esthetic zone during smiling or speaking. The final FP-1 restoration appears to the patient to be similar to a crown on a natural tooth. However, the implant abutment can rarely be treated exactly as a natural tooth prepared for a full crown. The cervical diameter of a maxillary central incisor is approximately 6.5 mm with an oval to triangular cross section. However, the implant abutment is usually 4 mm in diameter and round in cross section. In addition, the placement of the implant rarely corresponds exactly to the crown-root position of the original tooth. The thin labial bone lying over the facial aspect of a maxillary anterior root remodels after tooth loss and the crest width shifts to the palate, decreasing 40% within the first 2 years.11 The occlusal table is also usually modified in unesthetic regions to conform to the implant size and position and to direct vertical forces to the implant body. For example, posterior mandibular implant-supported prostheses have narrower occlusal tables at the expense of the buccal contour, because the implant is smaller in diameter and placed in the central fossa region of the tooth12 (Figure 5-3).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses