5 Potential for Poor Wound Healing
5.0 INTRODUCTION
Hard and soft tissue injury, whether due to surgical oral procedures, disease, or trauma, can cause the formation of wounds, which, if not secondarily infected, heal normally in an uncomplicated manner in healthy individuals. Surgical oral procedures typically fully heal, often without evidence of tissue injury. Inflammatory oral conditions, such as minor recurrent aphthous stomatitis and ulcerative oral lichen planus, present with recurrent painful mucosal ulcerations that may require medical intervention to promote healing but rarely result in scar formation. Orofacial trauma can range from a minor injury such as cheek biting or a pizza burn, which typically heals without complications, to more extensive injuries including facial fractures, in which healing may require surgical intervention and may be complicated by infection secondary to the introduction of foreign material into the wound.
Wound healing is a complex and highly organized process that involves coagulation (see chapter 3), acute inflammation, cellular regeneration and proliferation, and tissue remodeling. Acute inflammation is the early reaction to injury in which a vascular and cellular response removes debris and foreign bodies from the wound. Macrophages are released from the microcirculation and clear extracellular debris, fibrin, and other foreign material at the site of wound repair. Regeneration of injured tissue begins with cell replication and angiogenesis, controlled by a complex interplay of cytokines, growth factors, and other biostimulatory mediators. If wound repair is not achieved by regeneration alone, a granulation response occurs in which there is a proliferation of fibroblasts, followed by collagen deposition and organization of fibrous connective tissue, leading to scar formation. During the remodeling phase, the wound undergoes contraction and maturation, and in most cases results in clinically normal-appearing tissue.
Healing can occur through three basic mechanisms. Primary intention is the process of wound repair achieved when the wound borders are approximated (i.e., primary closure) using sutures or other techniques to keep the borders closed during healing. Secondary intention is characterized by a wound where the borders are not precisely closed, and granulation tissue replaces the gap between the two planes (i.e., secondary closure). This type of healing is generally slower than primary intention and has a greater risk of scar formation. Most dental procedures, such as extractions and gingivectomy, heal by secondary intention. Healing through tertiary intention is the process by which the wound is initially cleaned, debrided, and observed, followed by delayed primary closure, typically 4–5 days later. Use of reconstructive tissue grafts may undergo healing with tertiary intention.
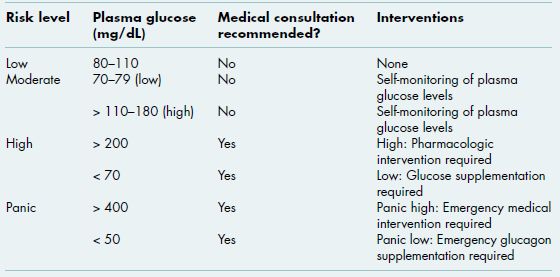
Table 5.1 Risk assessment for poor wound healing.
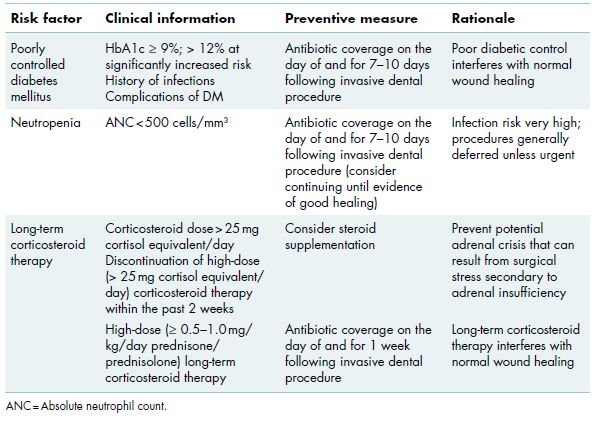
Systemic and local factors can influence wound healing. Systemic factors that can impede healing include inadequate circulation, compromised immune function, prolonged corticosteroid therapy, antiresorptive therapy, and nutritional deficiencies. Local factors that can adversely affect healing include the size and location of the wound, mechanical insult, foreign bodies such as debris and sutures, and infection, which is the single most important cause of delay in wound healing. Given the close association between healing and infection, there is some degree of unavoidable overlap with chapter 4, and therefore these two chapters should be considered in tandem. This chapter reviews the most common disorders that increase a patient’s susceptibility for poor wound healing and describes diagnostic tests that can be utilized to assess risk as well as strategies for risk reduction (Table 5.1).
5.1 Diabetes mellitus
Diabetes mellitus (DM) is an endocrine disorder characterized by progressive intolerance to glucose and its impaired metabolism. Dysfunction of the pancreatic beta cells causes defects in insulin secretion (Type 1 DM), insulin action (Type 2 DM), or both, which results in sustained hyperglycemia. Impaired glucose tolerance is a pre-diabetic state of compromised blood glucose metabolism that is associated with insulin resistance and often precedes Type 2 DM. Long-term hyperglycemia leads to the development of glycation in which glucose binds to proteins and other molecules through a non-enzymatic process. Glycation results in neutrophil dysfunction, diminished vascular perfusion and progressive peripheral nerve damage, all of which have systemic implications and contribute to poor wound healing.
Figure 5.1 Advanced periodontal disease in a 48-year-old male with poorly controlled diabetes mellitus who presented for evaluation of multiple loose teeth and halitosis.

Long-term complications of DM include end-stage renal disease requiring hemodialysis and/or renal transplantation, coronary artery disease that increases the risk of cerebrovascular accident and myocardial infarction, retinopathy that can lead to blindness, peripheral neuropathy of the hands and feet, and chronic wounds that in some cases require amputation. Oral complications of diabetes include delayed healing and frequent oral infections. Periodontal disease can be particularly aggressive, especially in poorly-controlled diabetic patients (Figure 5.1). Diabetes is a major public health concern in the United States due to its high prevalence and long-term health consequences.
Poorly regulated insulin activity, whether due to underlying disease or inadequate management, may result in acute hypo- or hyperglycemic states. Severe hypoglycemia is characterized by diaphoresis, disorientation, dizziness, and hypotension, and requires urgent medical management (i.e., oral supplementation with simple sugars or subcutaneous administration of glucagon). Hypoglycemia episodes are not associated with impaired healing or an increased risk of infection. Acute hyperglycemia is often benign and asymptomatic; however, in cases of severe hyperglycemia (e.g., blood glucose greater than 350 mg/dL), pharmacologic supplementation is crucial and emergency medical care may be required since serious complications such as osmotic diuresis can rapidly develop.
Oral health care providers are in a unique position of being able to engage in diabetes management activities to improve health behaviors of their diabetic patients. Regular dental visits provide opportunities for education about metabolic control, diet, and medication compliance, as well as physician referral when warranted.
5.1.1 Tests for diagnosis and monitoring of DM
Diagnosis and monitoring of DM are assessed through plasma glucose levels. Fasting plasma glucose and the oral glucose tolerance test are used for diagnosis, random plasma glucose is used for screening and monitoring, and glycated hemoglobin (HbA1c) measures long-term diabetic control.
Table 5.2 Tests for diagnosis and monitoring of diabetes mellitus.
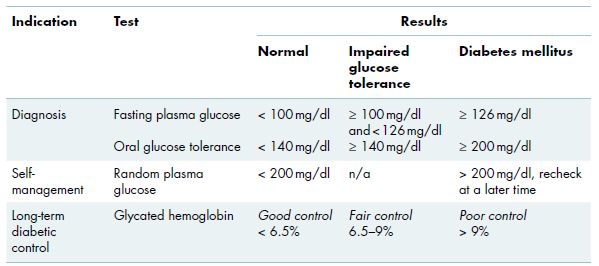
5.1.1.1 Diagnosis of DM: Fasting plasma glucose and oral glucose tolerance tests
Fasting plasma glucose is a routine test performed to assess the glucose level after a period of overnight fasting. This test is used to screen patients who may have signs or symptoms related to diabetes and is performed in a medical laboratory setting after 8–12 hours of no oral intake, with the exception of daily medications and water. Two fasting glucose measurements of at least 126 mg/dL are considered diagnostic for DM (Table 5.2).
The glucose tolerance test, also referred to as the oral glucose tolerance test, is a secondary diagnostic test that is performed when a patient has an equivocal fasting glucose test (i.e., near 126 mg/dL) or borderline glycated hemoglobin (i.e., near 6.5%; section 5.1.1.3). The test evaluates the body’s ability to closely regulate glucose levels. Subsequent to overnight fasting, the patient is given an oral dose of glucose (75 mg), usually in a liquid form, and plasma glucose levels are assessed at baseline, 1 hour and 2 hours following glucose intake (Table 5.2).
Figure 5.2 Home glucose meter for daily self-monitoring of random plasma glucose levels.
5.1.1.2 Glucose self-monitoring: Random plasma glucose
Random plasma glucose is defined as the measurement of circulating glucose levels at any given time throughout the day, with a normal value of 80–100 mg/dL (Table 5.2, Alert Box 5.1). The random plasma glucose can vary greatly in diabetics and depends on the time of day the measurement/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses