Chapter 5
Patient assessment
CHAPTER OBJECTIVES
- To consider the key aspects of the medical and dental history that are relevant to the management of periodontitis.
- To describe the clinical factors to assess when deciding which sites require periodontal treatment.
- To review the parameters to be assessed at diseased sites that will influence decisions about how to treat each site.
- To consider the medical factors (and other patient factors) that are relevant when planning periodontal therapy.
A detailed and thorough examination of the periodontal tissues is essential to ascertain disease extent (i.e., the distribution of pockets) and severity (i.e., the depth of pockets) in patients with periodontitis. This is routinely achieved by undertaking a full probing chart, recording probing depths at 6 points per tooth throughout the entire dentition. There is no shortcut available for this procedure, and it must be explained to the patient that detailed charting is essential to assess the baseline periodontal status (and therefore inform the diagnosis), to help plan the treatment (i.e., to decide which sites require instrumentation), and to be used as a reference point for assessing the response to the treatment. Measurement of probing depths is a fundamental component of periodontal therapy and decisions about instrumentation are made based on the depth of pockets, along with other factors such as bleeding on probing (BOP), the presence of biofilm and calculus, and other signs of inflammation.
THE PERIODONTAL EXAMINATION
First: listen
The periodontal examination starts with a conversation: why has the patient come to see you, what are their problems, what do they hope to achieve from treatment? It is best to ask open-ended questions that invite the patient to describe, in their own words, what their primary concerns are. Some of the typical sorts of questions that are useful to ask are shown in Box 5.1. As an example, a common complaint from patients with advanced periodontitis is drifting or over-eruption of teeth, resulting in a cosmetic problem (Figure 5.1). It is important to be aware of factors like this from the outset, so that the patient’s expectations can be managed: as a clinician, you may be very happy with a generalized reduction in probing depths

Figure 5.1 This patient presents with poor oral hygiene, plaque and calculus deposits, gingival bleeding, generalized gingival inflammation, and gingival recession. Clinical examination revealed generalized probing depths of 5–8 mm and alveolar bone loss affecting > 50% of the root length throughout the dentition. Her main concern is the appearance of the midline diastema, which has resulted from drifting of the upper incisors, notably tooth #8 (FDI 11). She wants something done about it! Cases such as this can be difficult to manage. It will probably not be possible to close the gap – orthodontics may not be appropriate even with a good outcome following the periodontal therapy. Expectation management is key – what is realistic to achieve must be explained from the outset
Box 5.1 Useful questions to ask a new patient regarding their periodontal status
You’ve come to see me regarding your gum health: what sorts of problems have you been experiencing?
Patients may describe a variety of problems: difficulty with chewing certain types of foods, altered speech, difficulty wearing dentures, bleeding gums, concerns about mobile teeth, compromised aesthetics. Alternatively, they may not have any particular symptoms or concerns at all, other than knowing that they have a problem with their gums.
Have you noticed any bleeding from the gums, for example when brushing your teeth, on waking up, or when eating?
Have you noticed if any of your teeth are loose?
Have you had any pain or sensitivity from any of your teeth?
Have you had any treatment for gum problems before?
If the patient has had treatment, ask further questions: when was the treatment done, how many appointments, how long did the treatment visits last for?
Do you smoke?
If the answer is yes, ask further questions: for how many years have they smoked, and how many cigarettes per day? If the patient is an ex-smoker, ask how many years they smoked for, how many cigarettes per day, and also, when did they quit?
Have you had any bad taste or bad breath? Have you noticed any gum swelling?
What do you use for cleaning your teeth?
Find out whether the patient uses a manual or powered brush, or any other cleaning aids such as floss or interproximal brushes. How often do they use them, for example, daily? How long do they spend on their oral hygiene procedures?
What is your understanding of what has caused your gum problems?
This is a really useful question to ask, as it will provide good information regarding the patient’s knowledge of the causes of periodontal problems, and will help you frame the discussions about periodontal disease and treatment in terms that are meaningful to the patient.
What would be your ideal outcome following treatment?
This will be linked to their primary complaints. For example, improved aesthetics may be the desired outcome, or eradication of bad breath, or reduced bleeding. It is important to manage the patient’s expectations, and to be very honest about what can realistically be achieved as a result of the periodontal therapy. If the nonsurgical periodontal therapy is the first part of a complex treatment approach that might involve, for example, fixed or removable prosthodontics, or orthodontics, or periodontal surgery, it is important that the patient is aware that the appropriateness of performing such complex procedures may well depend on the outcomes of the initial periodontal therapy, the response to treatment, and their ability to maintain a high standard of plaque control.
following treatment, but if the over-erupted tooth is still in the same place following treatment, the patient may not be as pleased! It is essential, therefore, to understand the patient’s main concerns so that you can discuss the aims of the treatment with them, and ensure that they are aware of the expected outcomes of your care.
Medical and dental history
Following on from the initial conversation with the patient, and before commencing the clinical examination, a full medical history should be recorded. A systematic approach should always be followed when recording the medical history; health history forms that are completed by the patient and then reviewed by the clinician together with the patient are useful to ensure that nothing is missed (Figure 5.2). Aspects of the medical history that are particularly relevant to periodontal therapy are shown in Box 5.2. It is also useful to be aware of the patient’s occupation, which can impact delivery of care (e.g., shift workers may find it difficult to attend appointments for treatment).
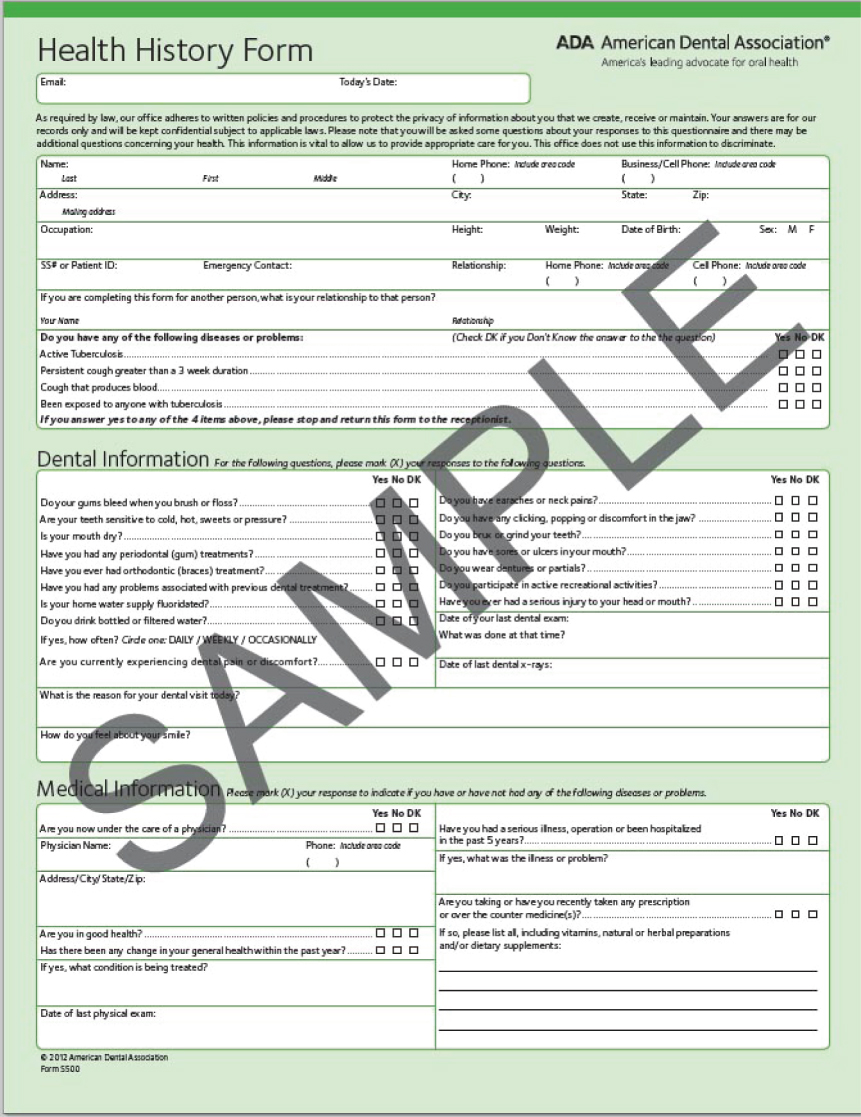
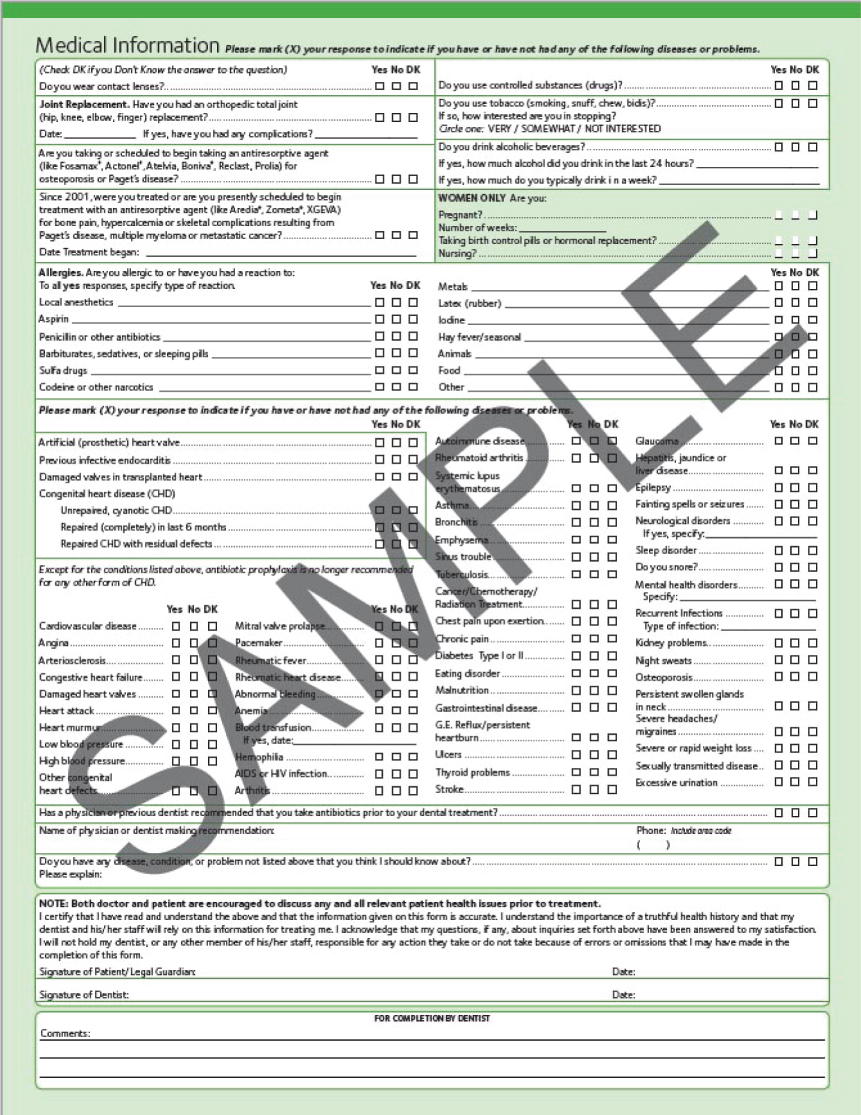
Figure 5.2 Health History Form from the American Dental Association – a great example of a comprehensive patient self-complete medical history form that is then reviewed and discussed by the clinician to ensure that full information about the patient’s medical status is obtained. Copyright © 2013 American Dental Association. All rights reserved. (Reprinted with permission)
Box 5.2 Key aspects of medical history relevant to periodontal therapy
Smoking status
It is essential to record a full smoking history. This includes number of cigarettes per day and number of years of smoking. In the case of ex-smokers, record how many cigarettes they used to smoke per day, how many years they smoked for, and when they quit. All current smokers must be advised about the harmful aspects of smoking on periodontal health, and encouraged and supported in attempts to quit.
Diabetes
Diabetes, particularly if poorly controlled, increases the risk for periodontitis. Ask patients about their level of glycaemic control, and if they know their most recent glycated hemoglobin measurements (HbA1c).
Medical status
Conditions such as cardiovascular diseases, stroke, hematologic disorders, bleeding tendencies, cancer, liver disease, endocrine disorders, neurological problems, and infectious diseases may all influence the management strategy adopted for the patient. Liaison with the patient’s medical physician may sometimes be necessary to obtain further information, to help the dentist plan the provision of dental care.
Medications
Certain medications are associated with drug-induced gingival overgrowth, such as some calcium channel blockers, phenytoin, and ciclosporin.
Bisphosphonate therapy (particularly intravenous therapy) increases the risk for osteonecrosis of the jaw.
Anticoagulants prolong bleeding, and will influence periodontal treatment decisions.
Corticosteroids (especially high doses) may influence immune responses and inflammation.
Allergy
This should include questions relating to medications, dental products (e.g., chlorhexidine, eugenol, and latex) as well as environmental allergens such as pollen.
Family history of periodontal disease
This is particularly relevant for younger individuals with suspected aggressive periodontitis, for which the key characteristics are advanced periodontitis (particularly in relation to age) in patients who are otherwise medically healthy, and who have a family history of periodontal disease.
The dental history should also be recorded. In relation to periodontal treatment, it is important to ascertain whether the patient has previously received periodontal therapy, and what form it took. Was surgical or nonsurgical treatment provided? How many episodes of instrumentation were performed? Was anesthesia used? How many appointments has the patient attended for periodontal therapy, including maintenance care? Or, is the patient presenting for the first time for periodontal therapy? It is also important to be aware of other planned dental treatment, such as restorative care, provision of fixed or removable prostheses, endodontics, orthodontics or implant therapy.
Clinical examination
It is necessary to perform a complete oral and dental examination. Extraoral assessment should focus on the lymph nodes, temporomandibular joints, and muscles of mastication. Intraoral examination must include a full dental charting (teeth present, caries, restorations, and tooth surface loss) as well as examination of the oral soft tissues (lips, tongue, palate, buccal mucosa, floor of mouth, and oropharynx).
Make an assessment of the level of oral hygiene, particularly focusing on plaque deposits at the gingival margin and interproximally, as well as the presence of calculus. Note sites at which oral hygiene is suboptimal, and consider if this is due to patient ineffectiveness (e.g., the patient may not be performing daily hygiene in these regions, or may be using the wrong oral hygiene device), or is due to local factors that make daily hygiene difficult in these regions (e.g., as a result of the presence of overhanging margins of restorations). Evaluate the gingival tissues for evidence of inflammation (characterized by redness and swelling), or other pathologies (e.g., drug induced gingival overgrowth). Drying of the tissues is important to improve visibility when examining the gingival tissues.
The cornerstone of the periodontal examination is periodontal probing, and involves the use of a periodontal probe. Periodontal probing is essential for periodontal diagnosis, treatment planning, and monitoring, and is the only reliable method available for detecting periodontal pockets. Periodontal pockets cannot be visualized on radiographs. A schematic representation of a periodontal pocket is shown in Figure 5.3.
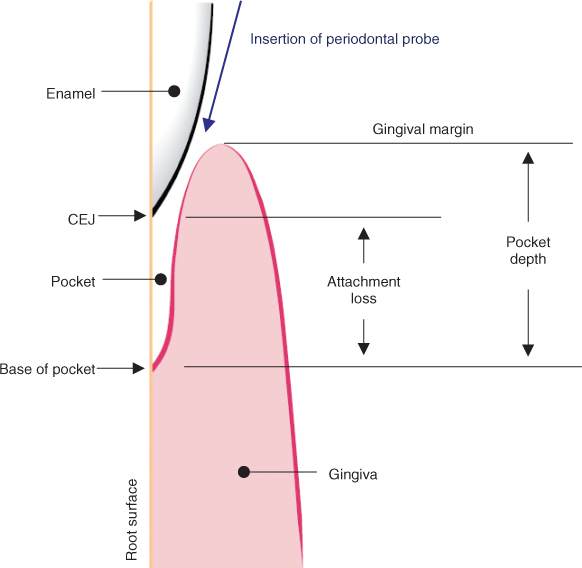
Figure 5.3 Schematic representation of a periodontal pocket. The probe is inserted to the depth of the pocket, and the measured probing depth is the distance from the free gingival margin to the probe tip, which is assumed to be at the base of the pocket. In inflamed tissues, the probe tends to penetrate the tissues at the base of the pocket, resulting in bleeding on probing, and also a higher measured probing depth (compared to the true pocket depth). Following treatment, resolution of inflammation results in shrinkage of the gingival tissues and greater resistance of the tissues at the base of the pocket to penetration by the probe. Both of these factors result in reduced probing depths following treatment. Whereas the reference point for measuring probing depth is the gingival margin, the reference point for measuring attachment loss is the CEJ. It may often be difficult to locate the CEJ, particularly in patients presenting with gingival inflammation, and for this reason, probing depths are the more useful measure for assessing periodontal status and response to treatment. CEJ: cemento-enamel junction. (Source: Preshaw et al., 2012. Reproduced with permission of Springer)
Although periodontal probing is often regarded as a simple procedure to perform, it is actually technically challenging and prone to error. The recorded probing depths can be affected by multiple factors including:
- probe position, angulation, and orientation
- force (pressure) applied
- probe diameter
- probe tip sharpness/bluntness
- clarity of probe markings and visibility of the site
- presence of blood, saliva, plaque, all of which can obscure probe markings
- presence of calculus (supra- or subgingival)
- margins of restorations
The force that should be applied when probing is generally considered to be around 0.25 Newtons (Hefti, 1997). This can be difficult to assess, but is typically the amount of force required to depress the skin on the pad of the thumb by about 1 mm with a periodontal probe.
Probing depths should be recorded at 6 sites per tooth (Figure 5.4). A systematic approach is essential to ensure that no sites are missed, and that the recording of the probing depths either onto paper records or into a computer system is accurate. A common method is to record probing depths as follows:
Figure 5.4 Follow a systematic approach when performing periodontal probing. 1: probe all the buccal sites in the upper arch, from right to left, starting at the disto-buccal aspect of the last standing molar. It is convenient to pause at the midline and call out bleeding on probing scores for the buccal aspects of the first quadrant (upper right quadrant) before progressing to probing the buccal aspects of the upper left quadrant. Call out the bleeding on probing scores for the upper left after completing the upper left probing. 2: after completing the buccal measurements, record the palatal probing depths in the maxilla, this time from left to right (again, it is useful to pause in the midline to call out bleeding scores before proceeding to completing the probing assessments at the right side). Repeat the process in the mandible: buccal first from right to left, and then lingual from left to right. Probe placement locations at six sites are shown on selected teeth. MB: mesio-buccal; B: buccal (i.e., mid-buccal); DB: disto-buccal; MP: mesio-palatal; P: palatal (i.e., mid-palatal); DP: disto-palatal; ML: mesio-lingual; L: lingual (i.e., mid-lingual); DL: disto-lingual
- Buccal surfaces of upper arch (from right to left)
- Palatal surfaces of upper arch (from left to right)
- Buccal surfaces of lower arch (from right to left)
- Lingual surfaces of lower arch (from left to right).
The probe should be inserted into the pocket, approximately parallel to the long axis of the tooth and “walked” around the tooth to record the probing depths. At interproximal sites, the probe will need to be angled slightly to ensure that the probe tip is at the depth of the pocket, which is typically below the contact point.
Record the probing depth measurements either onto a paper form, or into a computerized recording system. The most important aspect of the chart is that it should permit site-by-site comparisons of probing depths recorded at sequential probing examinations over time (e.g., so pre- and posttreatment measurements can be viewed on a site-by-site basis). An example of a paper-based probing chart is shown in Figure 5.5 and more thoughts about periodontal probing are presented in Box 5.3.
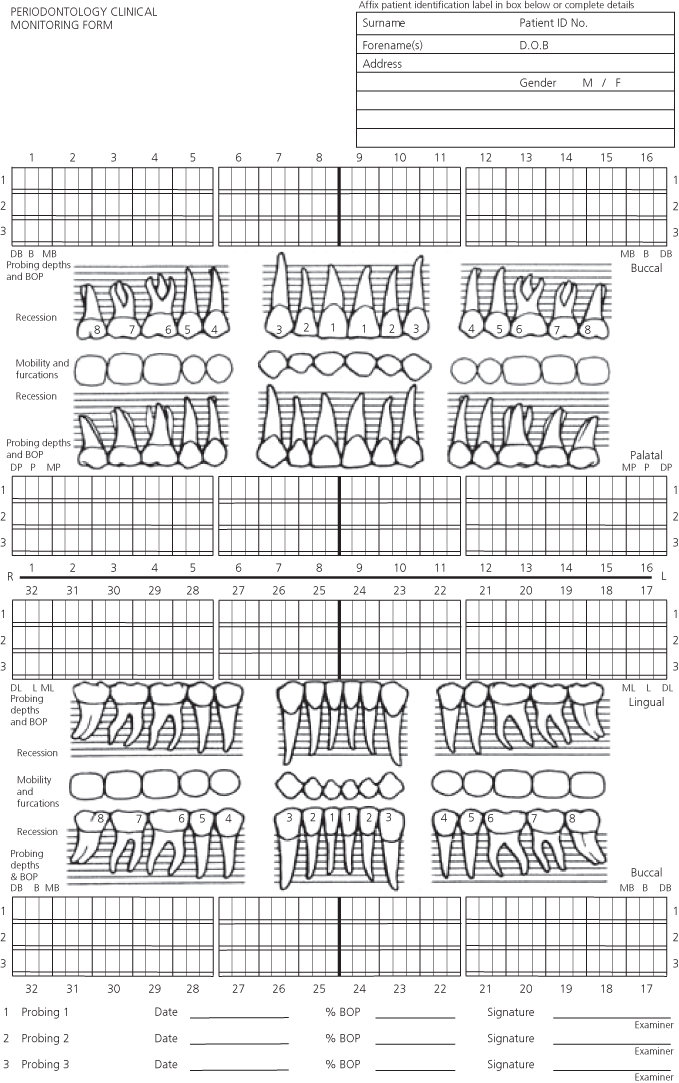
Figure 5.5 Paper recording form for periodontal assessment. This form permits up to 3 consecutive full mouth probing records to be made, allowing for site-by-site comparison in changes in probing depths that occur following treatment. Bleeding on probing can be recorded by circling the probing depth measurements (or, on this form, by shading in the small rectangle under each probing depth measurement). Recession can be drawn onto the form, as well as indications of mobility and furcation involvement
During the probing procedure, also measure recession, if present, at each site, as the distance from the CEJ to the gingival margin. BOP should be recorded as present/absent at each site following probing. In patients with minimally inflamed tissues, there may be very little bleeding, in which case it may be reasonable to wait until the midline has been reached in the probing sequence, and then look back over the probed quadrant to identify any isolated bleeding sites. On the other hand, in patients with extensive gingival inflammation (Figure 5.6), there may be profuse bleeding immediately after each site is probed, and in this case, it is more accurate to record BOP scores immediately after probing each site.

Figure 5.6 A new patient presenting for periodontal treatment for the first time. Initial inspection reveals extremely poor oral hygiene, abundant plaque and calculus deposits, extensive gingival inflammation and spontaneous gingival bleeding. Accurate periodontal probing will be difficult to perform because of the abundant plaque and calculus and the high probability of profuse bleeding after probing at each site. Nonetheless, an effort should be made to complete a full probing chart prior to commencing any treatment – it will take time (longer than usual!), with the need to remove plaque from the probe with a gauze swab after each probing measurement, and washing/aspiration and drying of the tissues to improve visibility
The presence of furcations should be assessed, using a curved furcation probe. Every furcation entrance should be checked: for maxillary molars, there are three potential furcations to assess (mid-buccal, mesio-palatal, disto-palatal) whereas for mandibular molars, there are two potential furcations to assess (mid-buccal, mid-lingual).
It may also be necessary to assess the occlusion in certain cases, and study models may be indicated. Clinical photographs can also be a useful component of the initial patient assessment.
IDENTIFYING SITES TO TREAT
Decisions about which teeth to retain and which to extract, or which sites to perform root surface debridement (RSD) at, can be very difficult to make. The main reason for the difficulty is that we cannot see into the future; we do not know which sites will progress, which sites will respond well to treatment, or whether the patient will be able to maintain compromised teeth.
Box 5.3 Periodontal probing – so much to think about!
The 6 sites versus Walk that Probe!
Recording probing depths at six sites per tooth (MB, B, DB, ML, L, DL) as shown in Figure 5.4 is standard throughout the world. These sites have been chosen because most of the time, they coincide with the locations of the deepest pockets around a tooth. The MB, DB, ML and DL locations are aiming to identify pockets underneath the contact points, which tend to be the areas at which the deepest pockets are located. And, the B and L (i.e., mid-buccal and mid-lingual) measurements at molars tend to coincide with areas of furcation involvement.
The question often arises: should I only insert the probe at exactly those 6 locations when I examine a patient, or should I “walk” the probe around the entire circumference of the tooth?
The answer is that we walk that probe! We walk the probe around the entire circumference of the tooth so that we can find the deepest probing depth measurements around the tooth, because that is what we are most interested in. We then use our clinical skill and judgment to record the deepest measurement at a particular region of the tooth into the most relevant (i.e., closest) of the six standard locations.
What else do we assess with a periodontal probe?
The periodontal probe is a pretty useful tool. We measure probing depths with it and elicit bleeding on probing as an indicator of inflammation. We wipe it along the tooth surface as we proceed with our examination to identify plaque (keep some gauze handy to wipe it clean so you can still read the markings on the probe). We use it to detect the presence of calculus and make assessments of root morphology. All of these factors are used to help us determine which sites to treat and how to treat them.
A research study reports a mean probing depth reduction of 1.2 mm… that doesn’t sound like much!
When we see an individual patient, and provide periodontal treatment, we naturally focus on the deep sites and the response to treatment at those individual sites. We may see a particular pocket reduce from 6 mm to 4 mm, or from 8 mm to 5 mm. Yet, when we read the research literature, much smaller probing depth reductions seem to be reported – why is this?
The answer is that most research studies report mean (i.e., average) probing depth reductions following treatment, across all sites. If a full mouth mean change is reported, this includes every site in the mouth, including the sites that were deep prior to treatment, as well as those that were shallow prior to treatment. Most patients with periodontitis have a mix of deep sites and shallow sites, including sites that may be 3 mm or less prior to treatment. We don’t expect those shallow sites to particularly change following therapy. Therefore, when calculating a mean probing depth reduction across the entire dentition, those shallow sites which don’t change much have the effect of “diluting” or “reducing”’ the magnitude of the probing depth reductions that occurred at the sites that were deep prior to treatment. Many studies nowadays stratify the analysis according to initial probing depth, for example, they might only report the probing depth reductions at sites that were 5 mm or greater prior to treatment, and ignore any changes at the sites that were 4 mm or less prior to treatment.
As an example, consider the patient shown in Figure 5.7. This patient attended for the first time in 2004 (Figure 5.7a), and a diagnosis of chronic periodontitis was reached. The treatment strategy involved personalized oral hygiene instruction, and ultrasonic RSD. No decisions were made about extractions, other than noting the poor prognosis of several of the teeth, including the first molars, notably #19 (FDI 36). This tooth responded positively to vitality testing, and the decision was made to retain the tooth. Further radiographs were obtained in 2007 (Figure 5.7b) and 2010 (Figure 5.7c) and throughout this period, the patient continued to receive periodontal maintenance care. The patient was able to achieve a high standard of oral hygiene, with excellent plaque control and minimal gingival inflammation, as can be seen in the clinical image obtained in 2010 (Figure 5.7d). Over this six-year period, the periodontal condition remained stable, there was no particular evidence of disease progression, and tooth #19 (FDI 36) remained vital, functional, and symptom-free.
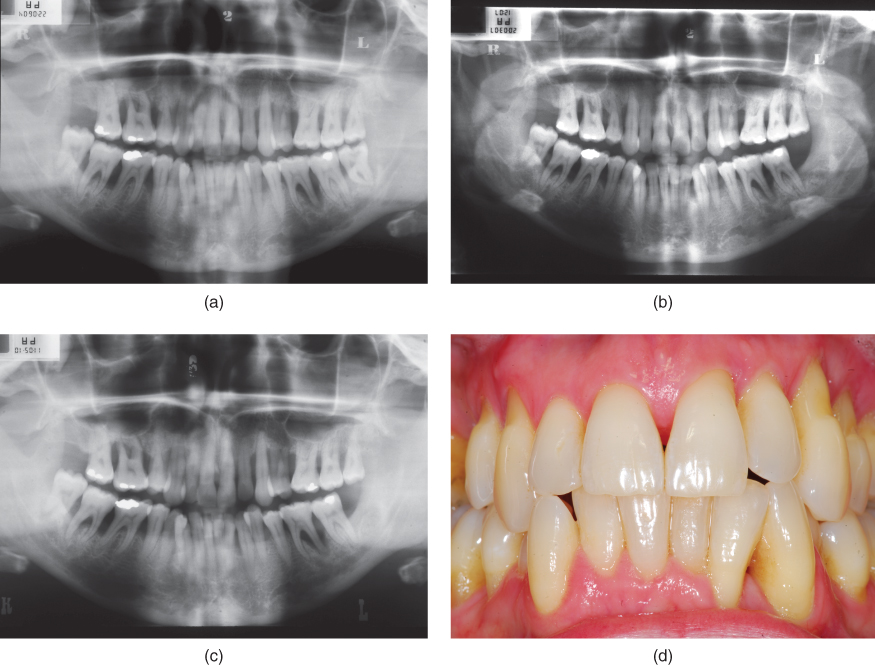
Figure 5.7 Radiographs obtained in 2004 (a), 2007 (b) and 2010 (c) which reveal that, although the patient presented with advanced periodontitis and generalized advanced alveolar bone loss with multiple vertical defects, over the course of 6 years of non-surgical periodontal therapy (episodes of RSD and OHI interspersed with periods of periodontal maintenance care) bone levels remained reasonably stable with no particular evidence of disease progression, even at compromised teeth such as #19 (FDI 36). The patient’s compliance with the periodontal therapy and excellent plaque control are evident in the clinical image (d) obtained in 2010
How many clinicians would have recommended extraction of tooth #19 (FDI 36) when the patient first presented in 2004? What other treatment options might have been considered? For example, extraction and replacement with an implant could have been considered, or alternatively, periodontal surgery involving hemisection of the tooth and removal of the distal root (and probably also endodontic treatment) could have been performed. Yet, in this case, the simplest treatment option (i.e., nonsurgical management involving RSD, oral hygiene instruction and long-term periodontal maintenance care) proved to be highly effective. Clearly, the patient was very compliant, but if the patient had not been able to maintain such a high level of plaque control, then the surgical options (e.g., implant placement or hemisection) would not have been indicated anyway. Review of the clinical chart for this patient reveals that the probing depth at the distal aspect of #19 (FDI 36) was 10 mm in 2004, 8 mm in 2007 and 5 mm in 2010.
This case highlights the difficulties that clinicians can face when deciding how to treat a patient with periodontitis. The “biological model” of periodontal treatment that was advocated by Kieser (see Chapter 1) suggests that the treatment response />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


