5 Mini Open Brow Lift
The Transfollicular Subcutaneous Approach
Numerous techniques have been described to treat the aging brow and forehead.1–22 Chapter 6 on endoscopic brow and forehead lift (EBFL) will make it apparent how advanced technology provided a new procedure that has become very popular and probably represents the most common contemporary brow lift technique. Despite its popularity, there remain surgeons who do not favor EBFL. Some may be intimidated by the equipment and learning curve and prefer the same coronal brow lift they learned decades ago. Other surgeons don’t like EBFL because they simply aren’t proficient at it. They have the training, they have the instrumentation, they do the procedure, but the results or longevity are lacking; this is actually a common scenario. I have personally met competent surgeons all over the world who have given up their scope and switched back to a blade. “Endoscopic brow lift does not work” is a statement frequently heard at meetings and conferences, yet there are thousands of surgeons who attest that it does!
Terminology plays an important role in understanding (or misunderstanding) surgical procedures, so we will discuss it first. Incisions made in front of hair follicles are termed trichophylic (hair loving) because the follicles are not disturbed. Incisions that transect intact hair follicles (transfollicular) have been termed trichophytic,20,22–26 tricho meaning “hair” and phytic either from the Greek phynai, “to be born,” or phyein, “to produce.” Ask different surgeons the meaning of trichophylic and trichophytic, and you are likely to get a variety of answers. I prefer to use the term transfollicular to describe the incision used with the mini open brow lift.
When discussing the pluses and minuses of various brow lift procedures, TFSBFL comes up a winner in many categories (Table 5-1). It is the only commonly used brow and forehead lift procedure that does not elevate the anterior hairline—very important, especially in females. For patients with a low hairline, virtually any brow lift procedure is acceptable; a nominal hairline elevation is not critical. For patients with higher hairlines (longer foreheads), no extra increase in the anterior hairline is acceptable, so these patients are optimum candidates for TFSBFL (Figure 5-1). In fact, it can lower the hairline if the superior scalp is freed.
Table 5-1 Relative Advantages of Subcutaneous Mini Open Brow and Forehead Technique Compared to Endoscopic Brow and Forehead Lift
| Subcutaneous Mini Open Brow and Forehead Lift | Endoscopic Brow and Forehead Lift |
|---|---|
| No specialized instrumentation required | Significant specialized instrumentation required |
| Minor to moderate learning curve | Significant learning curve |
| Simple subcutaneous dissection | Requires extensive dissection of multiple tissue planes |
| No concern of frontal nerve injury | Frontal nerve injury more problematic |
| Direct-vision technique | Closed technique |
| Does not raise the hairline | Raises the hairline |
| Excellent improvement of forehead rhytids | Less dramatic improvement of forehead rhytids |
| Very low tension on brow suspension | Often extreme tension to fixate brow |
| Control of brow suspension over entire brow | Less precise control of brow suspension |
| Subcutaneous dissection, less edema, faster recovery | Subperiosteal dissection, extends recovery |
| Direct access to brow depressors | Indirect access to brow depressors |
| No need for osseous fixation | Usually requires osseous fixation |
| No need for overcorrection | Frequently overcorrected |
| Predictable longevity | Longevity varies among surgeons |
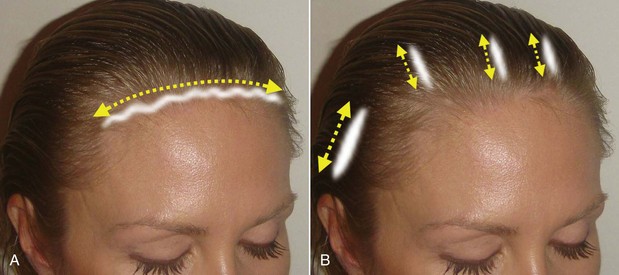
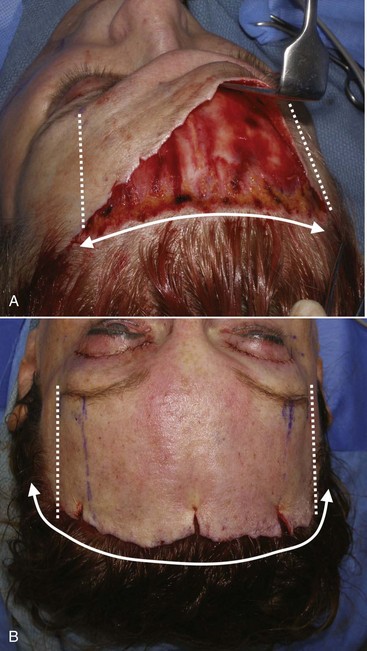
A high hairline is not the only reason to use TFSBFL. Another huge advantage is that it is a direct-vision procedure and allows direct vision from scalpel to suture. No complex instrumentation and digital equipment are required, making it simpler. The learning curve is less complex than EBFL, and it is very attuned to facelift surgery, which most cosmetic facial surgeons are familiar with. The TFSBFL is a skin-excision technique and is simply a facelift for the forehead and brow. Subcutaneous dissection, flap development, skin excision, and resuturing techniques are virtually identical to rhytidectomy. Being a subcutaneous procedure, there is less edema and ecchymosis compared to other brow lift techniques. Since this is a skin-excision technique, stability is excellent, and the result is immediately evident. As the skin is excised all across the horizontal width of the brow and the area resutured, the suspension is dispersed across the entire brow hairline (Figure 5-2, A). This is in extreme opposition to the EBFL, which only has several fixation points that are suspended with extreme tension in selected regions (see Figure 5-2, B).
There are few disadvantages to the TFSBFL technique. One relative disadvantage is that it is not reversible insofar as it is a skin-excision technique. An endoscopic brow and forehead lift that was overcorrected could be reversed in the first several weeks by removing the fixation and redissecting the pockets. There is no easy means of reversing TFSBFL after the skin has been removed. Another relative disadvantage is the public or collegial perception that open brow lifts are excessive or antiquated. This thinking is mostly a result of opinions concerning older coronal brow lifts. Endoscopic proponents claim that EBFL is a minimally invasive procedure. This is simply not true. Only the actual incisions are less invasive. In reality, EBFL is the most aggressive brow lift technique, traversing numerous tissue planes and necessitating cranial fixation. Comparatively, TFSBFL is a very conservative procedure. There is the stigma of a visible incision for several weeks, but when this procedure is performed correctly, the incision is rarely a concern. Multiple authors have described various subcutaneous approaches for brow and forehead lifting.10–14
Surgical Technique
The patient is marked preoperatively in the holding area. The area of maximum brow elevation is decided with the patient looking in the mirror. This area generally corresponds to the lateral pupillary limbus but is personal preference (Figure 5-3). The proposed incision can also be marked preoperatively, which can assist the novice surgeon, but in reality it is just as easy to perform this in surgery. Although it is commonly discussed as the junction of the medial and lateral brow being the area of maximum elevation, I personally feel that this varies on every patient and I always seek input from the patient when deciding how and where to elevate the brows. In addition, the medial brow should not be over elevated as this leads to the unnatural or overdone appearance in patients.
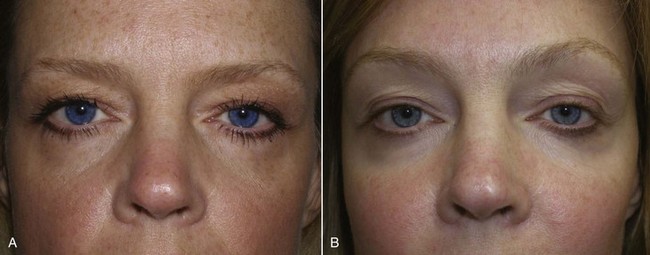
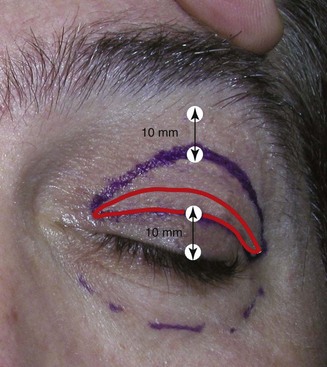
As outlined in Chapter 6, Brow and Forehead Lifting, I perform simultaneous blepharoplasty on 99% of my brow patients (Figure 5-4). I do, however, temper the amount of skin removal and the incision outline of the upper blepharoplasty when performing concomitant brow lift, regardless of approach (Figures 5-5 and 5-6).
The entire brow and forehead is injected with tumescent anesthesia, and the actual hair incision is injected with lidocaine 2%, 1 : 100,000 epinephrine (Figure 5-7). It is important to remember that this is a subcutaneous procedure, and the anesthesia must be injected subcutaneously. The eyelid surgery is performed first, which allows the local anesthesia and vasoconstrictor to take effect in the brow.
Crafting the Incision
The transfollicular (trichophytic) incision does not happen by accident and requires some level of skill to perform properly. Most surgical skin incisions are made with the scalpel blade perpendicular to the skin surface, which produces a flat interface on both sides of the healing skin. The trichophytic incision is made using an extreme angle of bevel when incising. The scalpel is actually held at a 10- to 20-degree angle, which almost makes the scalpel appear perpendicular to the skin surface (Figure 5-8). It is of extreme importance to keep the scalpel at the same angle along the entire incision. Again, the angulation of the incision is the crux of this procedure.
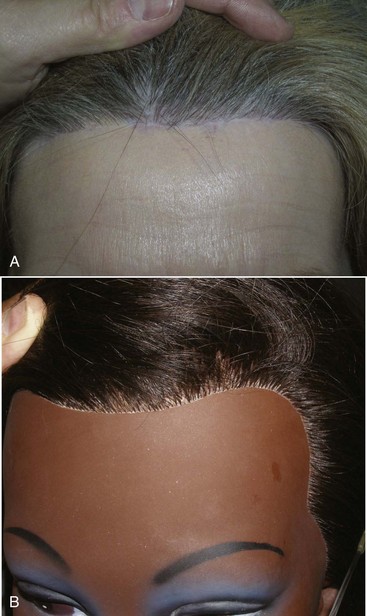
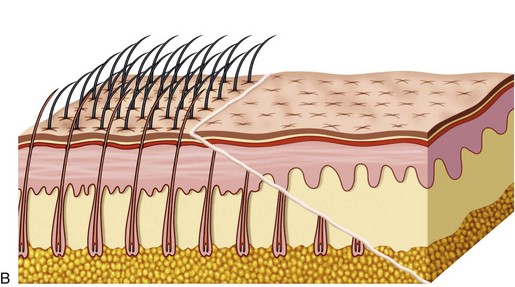
The incision pattern is also very critical for a naturally appearing hairline scar. First and foremost, the incision should never be made anterior to the hairline. The trichophylic incision totally avoids any hair follicles. This may sound good in theory and will definitely be easier to incise and close, but the aesthetics are frequently unacceptable. In my opinion, it should never be attempted. I frequently hear surgeons advocate the prehairline incision but continually see patients in my office who were treated elsewhere and have unacceptably visible trichophylic incisions. There are few straight lines in nature. Also important is the fact that there is no such thing as a “natural hairline.” Only a toupee or a bad hair transplant produces a true “hairline” (Figure 5-9). Making a straight-line prefollicular incision on a patient’s forehead can make them an “incision cripple” for life, with a visible and often hypopigmented scar. A natural hairline is not a line at all but a gradual transition of follicular density from the very thin and sparse vellus anterior hairs to the area of more follicular density where the hairline thickens (Figure 5-10).
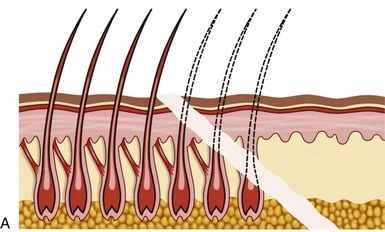
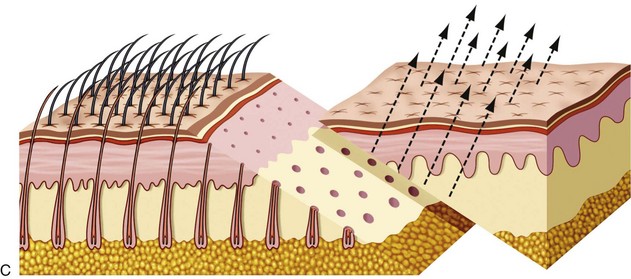
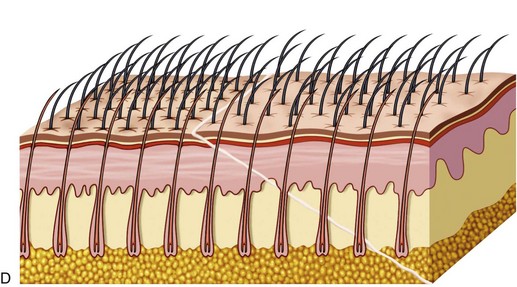
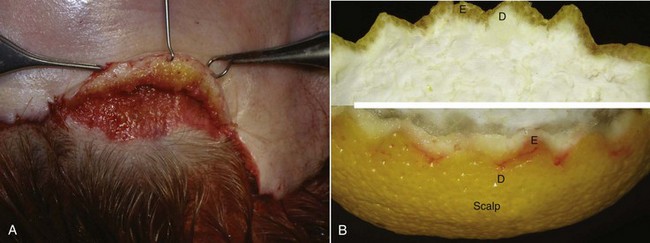
The transfollicular (trichophytic) incision is a totally different animal in design. First and foremost, the incision is designed to “cut across” existing hair follicles and is intentionally placed about 5 mm posterior to the anterior hairline. The optimum placement of this incision is at the region of the follicular density change from the thin, sparse anterior hairs to the denser follicles of the “actual” hairline which averages about 5 mm it the hairline (Figure 5-11, A). After the incision is made, excess skin trimmed, and the flap replaced, the transected follicles will lie under the newly placed flap, which is beveled (see Figure 5-11, B). As the wound matures (over several weeks), the hair bulbs of the transected follicles begin to grow through the thinly beveled flap (see Figure 5-11, C). When fully mature, most of the transected follicles will regrow through the flap and effectively camouflage the scar (see Figure 5-11, D).
The first step to successful TFSBFL and an aesthetic scar is a firm understanding of this incision. The bevel of the incision is critical and must be the same angle on both flaps. The first incision is an extreme bevel, and the second incision on the excess skin must be cut at the same angle and bevel as the initial incision. There are several reasons for this. The beveled flap will transition from subcutaneous to dermal to epidermal. The thin dermal/epidermal interface allows a thin enough transition to allow the underlying follicles to perforate the flap. To illustrate this transition, Figure 5-12 shows a beveled incision on a lemon peel; the white region corresponds to the dermis, and the yellow region corresponds to the epidermis.
Incision Position
I stated earlier that linear prefollicular incisions produce unaesthetic scars. It is appropriate to mention at this point that even irregular geometric incisions are unfavorable when placed anterior to the hair follicles (Figure 5-13). Incision position is critical.
The TFSBFL incision is optimally placed about 5 mm posterior to the most anterior hairline, which corresponds to the change in follicular density from sparse to thick. To be effective, this incision must be placed posteriorly enough to transect several rows of hair follicles; otherwise there are no follicles to regrow through the scar (Figure 5-14).
Incision Geometry
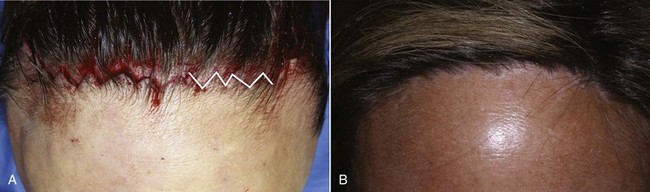
Keeping with incision design, the next aspect to be addressed is incision geometry. Understanding that the incision is placed about 5 mm into the hairline, the configuration can be regular with large or small triangles or irregular with random undulating geometry. Different surgeons prefer one of these configurations over the others. Proponents of large triangular incisions say that the incision, skin excision, and reapproximation of the trimmed flap is less laborious. My experience with the larger triangular configured flaps has been poor; this intentional geometry is obvious after healing (Figure 5-15).
Some surgeons prefer much smaller triangular incisions. I have experienced acceptable results with this type of incision but have mixed feelings about using small triangles. The increased surface area makes for a much more complex incision, excision, and especially suturing (Figure 5-16). It heals with acceptable results but is simply more time intense. Additionally, as the triangles become smaller they become more like a straight line, which is unfavorable.

FIGURE 5-16 Small triangles create an aesthetic scar but are much more time intense to incise, trim, and suture.
(Courtesy Todd Owsley, DDS, MD.)
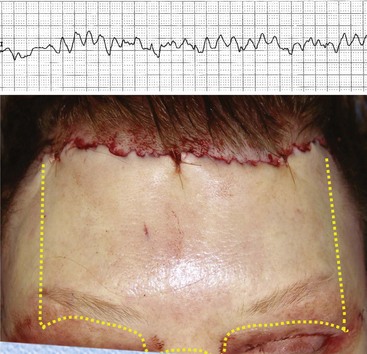
After experimenting with all the common geometric incision patterns, I have settled on a random, irregular, undulating incision pattern (Figure 5-17). This incision is made by using the scalpel in a reciprocating manner much like filleting a fish. The pattern is basically irregular and reminiscent of ventricular fibrillation on an ECG. When I teach this technique to residents, I tell them to incise like they’ve had too much coffee. The incision pattern and the angle of the cut are both critical factors in the success of this technique. If a patient has a prominent widow’s peak, it is better to cut through the lower third of the apex instead of following the distinct V shape of the peak. Otherwise the angles are too conspicuous with the final scar.
The extent of the incision is commensurate with the amount of aging changes specific to the patient. Younger patients without extreme lateral brow hooding can be treated with shorter incisions, because the amount of lateral dissection is less. In the younger patient, the incision and dissection only need to be made to a point just lateral to the maximum desired arch of the brow (Figure 5-18). In other words, as the dissection is made over the brow and it begins to be released, the dissection can stop just past the area of maximum arch. This usually corresponds the lateral limbus. When this area is released and the brow is significantly arched, there is no need to continue lateral dissection (Figure 5-19, A).
In the older patient or those with significant lateral hooding, increased lateral dissection will be required, thus a wider incision and dissection (see Figure 5-19, B). With this technique, no incision is ever carried lateral to the temporal crest.
Once the incision is made, the next step is to “pretunnel” the subcutaneous flap (Figure 5-20). This step is not performed by all surgeons, but I truly feel it is worth the small amount of time required. It is absolutely critical to make the flap dissection in the subcutaneous plane. />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses