5
Fluid management
The maintenance of fluid, electrolyte balance and blood volume is crucial to good outcomes following surgery. The fundamental goal is delivery of adequate oxygen to the tissues, which can be expressed by the oxygen delivery equation (Table 5.1) showing the factors that determine oxygen delivery:
- cardiac output (= stroke volume × heart rate);
- haemoglobin concentration;
- oxygen saturation.
Table 5.1 Oxygen delivery equation – normal values
| Oxygen delivery (DO2) = CO × [Hb] × % oxygen saturation (SaO2) × 1.34 |
| DO2 = CO × [Hb] × 1.34 × 0.99 |
| DO2 = 5 × 150 × 1.34 × 0.99 |
| DO2 = 1000 mL O2/min approx. |
Units: DO2, mL O2/min; CO, L/min; Hb, g/L.
Extremes of fluid management have a detrimental outcome, particularly for patients undergoing major surgery and/or patients with poor physiological reserve. Too little fluid results in dehydration and haemoconcentration, leading to a poor cardiac output and oxygen delivery to the tissues. If left untreated, in the early stages compensation will occur with increased oxygen extraction and a switch to anaerobic metabolism and production of lactic acid. Eventually, there will be organ failure when compensatory mechanisms are exhausted. Conversely, excess fluid management will overwhelm the circulation, with fluid will leaking out into the tissues, causing oedema. This too will impede cellular oxygenation and healing and causes organ dysfunction, especially in the lungs. For many patients there may be a considerable amount of physiological reserve and they may cope well with relative extremes of fluid balance, but for some patients the margins between inadequate and excessive fluid administration may be very small.
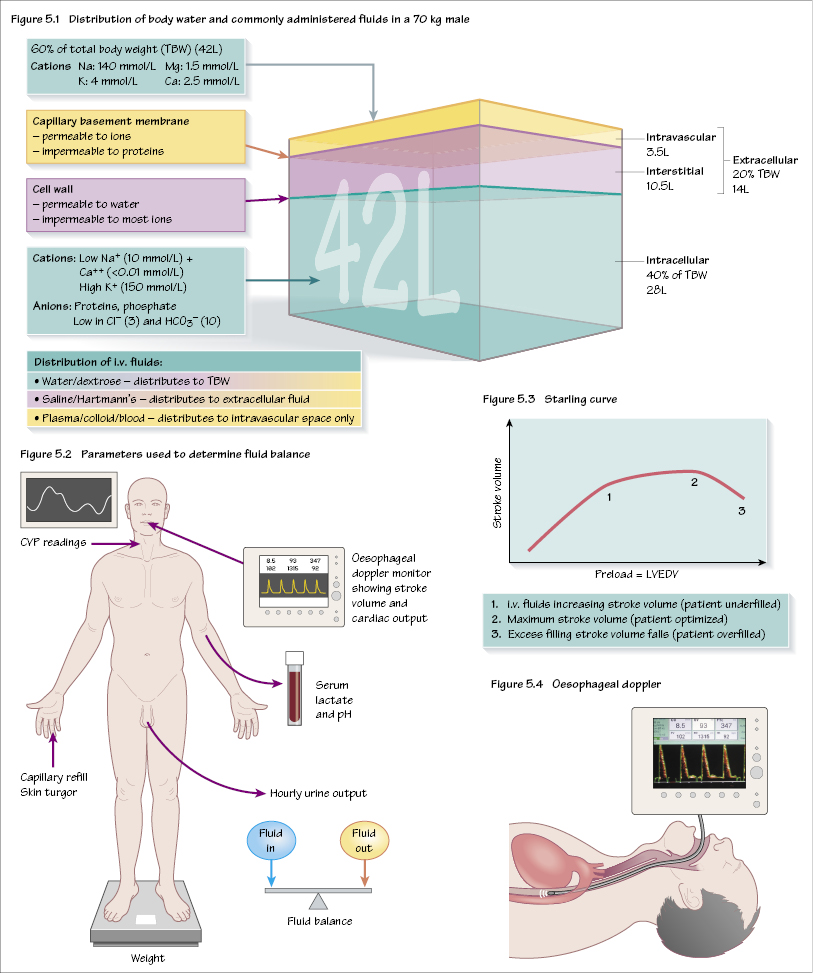
Fluid compartments
The body contains approximately 60% water. Approximately two-thirds of this is intracellular, and one-third extracellular, with the extracellular fluid further subdivided into interstitial and intravascular fluid. Figure 5.1 shows these compartments. There are two points to note:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


