Esthetics and Its Relationship to Function
Robert Lee
Introduction
However pleasing a dental restoration may appear, if it is destructive to the biologic system, it is “ugly.” Many dentists and laboratory technicians lack knowledge concerning natural tooth morphology and tooth positions that help create beautiful teeth and smiles and good function. Dentists who have devoted much of their lives studying and practicing occlusal rehabilitation have generally ignored esthetics while concentrating on improved function, joint stability, and comfort for their patients. On the other hand, dentists who have concentrated their efforts on esthetics have often paid little attention to function. If we understand the functions of teeth, it is easier to reproduce them in natural-like artificial forms because form follows function. Today’s challenge is to give patients the best of both worlds: good function and good esthetics.
In modern humans the primary functions of the teeth are for (1) mastication, (2) swallowing, (3) speech, (4) expression (eg, smiling), (5) psychologic, (6) esthetics, and (7) craniomandibular stabilization.
Bioesthetics is the study or theory of the beauty of living things in their natural forms and functions. This chapter presents bioesthetic relationships of natural unworn tooth forms to (1) rest position, (2) centric relation position, (3) vertical dimension of occlusion, (4) vertical and horizontal overbite, (5) condyle positions during rest and function, (6) plane of occlusion, and (7) mastication. The role of anterior crown morphology and tooth position and their importance for both esthetics and function will be covered in particular.
Esthetics involves more than the six anterior maxillary teeth, however. In most people it goes at least back to the first molars during a large smile or laugh (Fig 5-1). Consideration will also be given to the form and function of posterior crowns. Because occlusal loading affects the longevity of the teeth, periodontium, joints, and dental restorations, this chapter discusses how tooth morphology relates to occlusal loading of the gnathic system. Some important aspects of clinical treatments for bioesthetic occlusion will be presented in the latter part of this chapter.

Fig 5-1 Smile of a 27-year-old woman showing mesial of maxillary first molars.
Natural unworn permanent crown morphology
The following discussion of the crowns of teeth is not intended to be a complete anatomic description but rather highlights some significant morphologic factors relating to oral functions and esthetics, which perhaps have been overlooked. Dental morphology and anatomy books often show average tooth lengths skewed to the low end because they include worn teeth.1–4 It is necessary to have unworn crown morphology for good esthetics as well as function. Nature produces sharp tooth morphology on both anterior and posterior occlusal surfaces. However, to protect the extremely hard prismatic hydroxyapatite enamel from fracturing the sharp incisal edges, cusp points, and ridges, nature has provided convexity at the crests and apexes of these tooth structures.
Mandibular incisors
Although the mandibular incisors are the smallest teeth in the mouth, they are a physiologic cornerstone for good occlusion. It is almost impossible to have long-lasting nontraumatic functional occlusion without adequate clinical crown lengths of these teeth. Unworn natural mandibular central and lateral incisors range from 9 to 12 mm from the cementoenamel junction to the incisal edge (Fig 5-2) with an average length of 10 mm (Fig 5-3). The central incisors are slightly narrower than the laterals. The incisal edges from labial to lingual are about 0.5 mm (Fig 5-4). The actual incisal edges are even sharper because of their convexity (Fig 5-5). The mandibular incisors have a labial angulation in the dental arch.
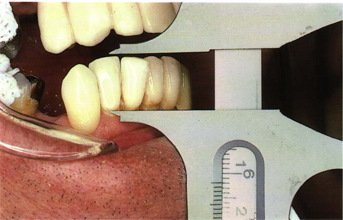
Fig 5-2 A 12-mm mandibular incisor.
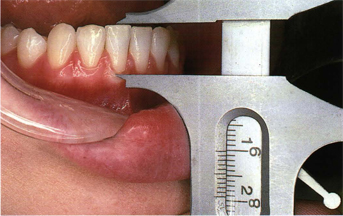
Fig 5-3 A 10-mm (average length) mandibular incisor.
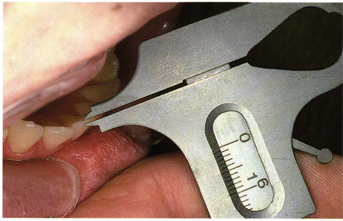
Fig 5-4 Cutting edges of unworn mandibular incisors are 0.5 to 0.75 mm.
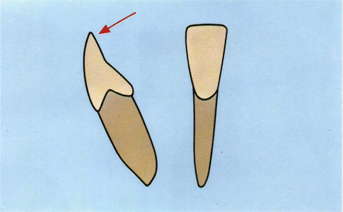
Fig 5-5 Profile tracing of actual mandibular incisor. The arrow indicates sharp convex cutting edge.
Maxillary incisors
A facial view of maxillary unworn natural anterior teeth in the mouth generally show relatively large, long central incisor crowns (see Fig 5-1). Mesial and distal incisal edges of unworn central incisors are rounded. The straight incisal edges often observed on central incisors are usually caused by wear patterns. Labial to lingual incisal edge contours are convex but sharp (about 0.7 mm). The lateral incisors are smaller and shorter, with more rounded mesiodistal incisal edges than the central incisors. The crown length of maxillary unworn central incisors ranges from 11 to 13 mm, with an average of 12 mm from the cementoenamel junction to the incisal edge (Fig 5-6). The lateral incisors are about 10 mm long with the incisal edge about 1 to 2 mm shorter than the central incisors. The gingival height of the lateral incisor is about 1 mm below the central incisor (Fig 5-7). The maxillary incisors have a labial incisal angulation in the dental arch. The concave lingual fossa of the maxillary incisors is designed for phonetics and forward posturing of the mandibular incisors in speaking and rest positions. The lingual fossa of the maxillary incisors also allow space for protrusive and lateral cyclic movements of the mandibular incisors during mastication.
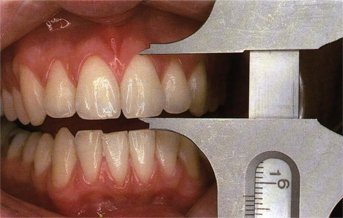
Fig 5-6 A 12.5-mm maxillary central incisor with slightly worn incisal edge.
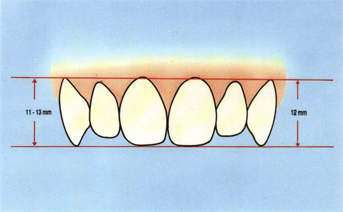
Fig 5-7 In good occluding dentitions the maxillary central incisors and canines are positioned about the same vertically and the lateral incisors are shorter both cervically and incisally.
Maxillary “canine area”
It may be helpful to think of the canine and premolar teeth as the “canine area.” Viewing the buccal aspects of the maxillary teeth, the canine (first canine) cusp tip is the longest and sharpest. Maxillary canines range from 11 to 13 mm with an average length of about 12 mm (Fig 5-8). The cusp tips of the canines are nearly as long as the central incisors in the plane of occlusion. The cervical height of the maxillary canines is at least as high as that of the central incisors. The buccal cusp of the “second canine” (first premolar) is slightly shorter than the first canine. The “third canine” (second premolar) buccal cusp is slightly shorter than the “second canine.” In the canine area the buccal cusp tips of the first, second, and third “canines” form a straight line (Fig 5-9). This straight line includes the mesiobuccal cusp of the first molar. The contact areas of these teeth also form a straight line (Fig 5-10). The buccal cervical heights of the first, second, and third “canines” and back to the cervical line of the first molar form a-Straight line (Fig 5-10). These three straight lines created by the cusp tips, cementoenamel junctions, and contact areas are not parallel but are distally converging lines, which help produce better functional tooth morphology while also producing good natural esthetics. The arrangement of these teeth to form these converging lines has been referred to as the graduation effect. The large buccal cusps of these teeth are important in medial guidance by the chewing side (ipsilateral) teeth. They guide the lateral mandibular movements in a more vertical manner in the coronal (frontal) plane and are the major factors in preventing harmful posterior contacts of the non-chewing side (contralateral) teeth.
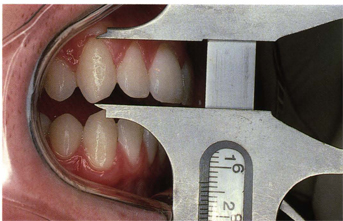
Fig 5-8 A 13-mm right maxillary canine with slight attrition.

Fig 5-9 Dentition of a 55-year-old man showing the gradation effect of the “first canine,” “second canine” (first premolar), and “third canine” (second premolar).
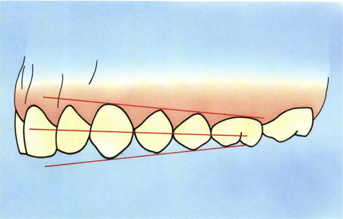
Fig 5-10 Distally converging lines (gradation effect) show height of cementoenamel junctions, interproximal contact points, and buccal cusp tips.
In a good unworn natural dentition the buccal embrasures mesial and distal to the first canine are generally about 90° (Fig 5-11). The mesial and distal marginal ridges of the first, second, and third canines are located gingivally. These gingivally placed marginal ridges create generous, beautiful, natural buccal cusp forms, which are also compatible both functionally and esthetically with the good anterior lengths and positions of the incisors. On the first premolar the buccolingual angle of the buccal cusps is about 65° and the lingual cusp about 90° (Fig 5-12). The triangular ridge height to groove depth is often 90° or steeper. The cusp tip-to-fossa depth is about 4 mm in the first premolar. The maxillary second premolar cusps are not quite as sharp and long as the first premolar (Fig 5-13).
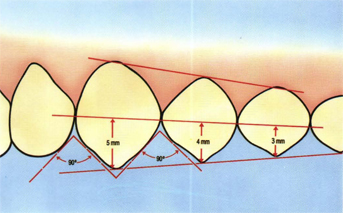
Fig 5-11 The length of the buccal cusps of the “first, second, and third” canines (measured from the interproximal contact points) are about 5, 4, and 3 mm, respectively. The mesial and distal embrasures of the “first canine” are about 90° generally.
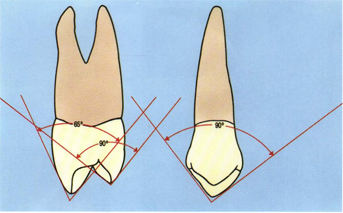
Fig 5-12 The buccal cusp of the maxillary “second canine” is about 65° buccolingually and about 90° mesiodistally, whereas the lingual cusp is about 90° buccolingually and 65° mesiodistally.
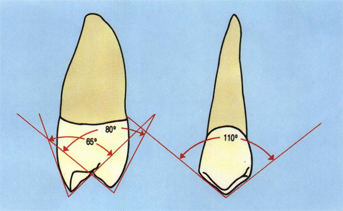
Fig 5-13 The buccal cusp of the “third canine” (second premolar) is about the same as the “second canine” (first premolar) buccolingually but is more obtuse (110°) mesiodistally. The lingual cusp of the second premolar is at least as sharp (80°) as the first premolar buccolingually. The lingual cusp of the second premolar is about 90° mesiodistally.
Grooves of premolar teeth are naturally deep for function and to allow the pressure of food to dissipate during mastication. The deep grooves of the teeth add immensely to natural esthetics when the patient is laughing and the occlusal surfaces are showing. The functioning of sharp premolar teeth are important during mastication of tough or hard foods, such as meat, carrots, apples, bread crusts, and nuts, as well as vertical guidance of the mandible.
Mandibular “canine area”
Unworn mandibular canines have the longest crowns in the mouth (Fig 5-14). Mandibular canine crown lengths range from 11 to 15 mm with an average length of about 12 mm (Fig 5-15). The canine tips are sharp and pointed. The mandibular canines and premolars also have gingivally placed marginal ridges that produce large buccal cusps. The buccal cusp of the first premolar is exceptionally large and sharp. The buccolingual angle of the buccal cusp of the first premolar is about 65° (Fig 5-16). The buccolingual cusp angle of the mandibular second premolar is about 75°, which also makes it sharp (Fig 5-17). The mesial and distal embrasures on the mandibular canines and first premolars are steep (about 90°) (Fig 5-18).
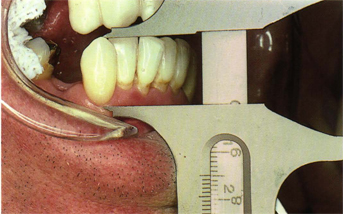
Fig 5-14 Mandibular canine teeth usually have the longest clinical crowns in the mouth; this mandibular canine measures 15 mm.
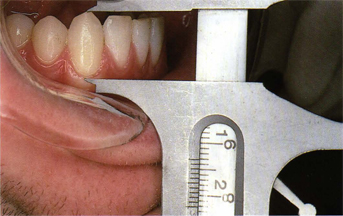
Fig 5-15 Mandibular canines average 12 to 13 mm from the cementoenamel junction to the cusp tip.
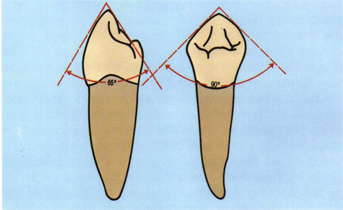
Fig 5-16 The buccal cusp of the mandibular “second canine” (first premolar) is about 65° buccolingually and 90° mesiodistally.
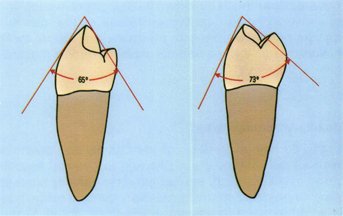
Fig 5-17 The buccolingual angle of the mandibular “third canine” (second premolar) is about 75°, which is about 10° less than the first premolar.

Fig 5-18 Mandibular canine area teeth in natural dentition of a 32-year-old man showing large, steep embrasures.
Molars
Although cusp angles of molars are not as steep as those in the canine area teeth, it is usually a surprise to realize just how long and sharp the cusps are on unworn molars. The mesiodistal cusp angles average about 100° and the buccolingual cusp angles average about 90° (Fig 5-19). The triangular ridge height to groove depth often exceeds 90°. Unworn molar cusp heights to fossa depths range from 3 to 4 mm. The cusp ridges are angular to about 90° buccolingually. The cusp triangular ridges are also basically about 90°. The buccal cusps of the maxillary molars are for protection of the cheek and mucosa, proprioceptive against the cheek and mucosa, and for holding food on the occlusal table. The lingual cusps of mandibular molars are for protection of the tongue, proprioceptive against the tongue, and for holding food on the occlusal table. The lingual cusps of maxillary molars and the buccal cusps of mandibular molars are for piercing food followed by the cusp ridges, which split, shear, and crush the food (see Fig 5-19). The steep triangular ridges are designed for vertical shearing and crushing of food. The grooves and embrasures are for the escape and extrusion of food and to reduce the load of mastication on the teeth and other components of the gnathic system.
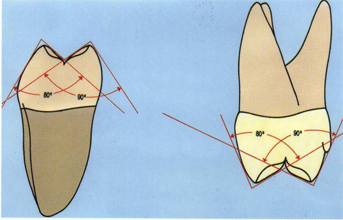
Fig 5-19 The buccal angles of maxillary and mandibular first molars are sharp, averaging generally between 80° and 90° buccolingually.
It is important that molar crown morphology be in a naturally sharp, unworn form to be compatible with the bioesthetics and naturally steep occlusal function of the incisors, canines, and premolars. The cusp of Carabelli often seen on maxillary molars may be of benefit in protection of the tongue and for proprioceptive guidance against the tongue. The cusp of Carabelli can also help to create a sharper buccolingual profile to the mesiolingual cusp of maxillary molars (see Fig 5-19).
Tooth genetics
Tooth morphology is totally genetic and is not specific to race or gender. Unerupted permanent teeth of young people of all races, including primitive people, such as aborigines, have sharp cusps. One cannot tell a young unworn Australian aborigine’s tooth form from that of a young unworn white’s. Anatomists and physiologists agree that tooth morphology is not specific to individuals any more than other organs of the body. There is a biologic spectrum or range of cusp lengths in natural tooth morphology (Figs 5-20 and 5-21). In any case, however, nature always produces sharp teeth genetically.
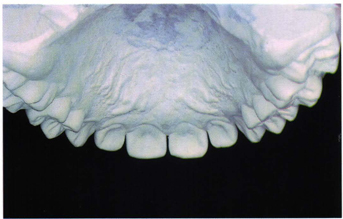
Fig 5-20 Casts of a young teenage girl representing the low end of cusp height range.
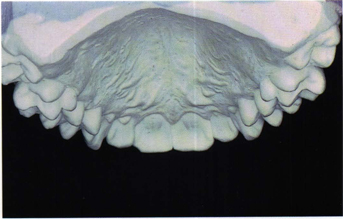
Fig 5-21 Casts of a young teenage girl representing the steep end of cusp height range.
Natural crown morphology of both anterior and posterior teeth develops early in life and is complete in every detail prior to tooth eruption into the oral cavity (Fig 5-22). However, the other components of the gnathostomatic system, including the joints, ligaments, muscles, maxilla, mandible, and other cranial facial bones, continue to change significantly long after the occlusal morphology of the teeth is complete. These changing components, such as the temporomandibular joints, maxilla and mandible, are predetermined by genetics. The skeletal components, however, are subject to environmental modification by factors such as abnormal posturing of the mandible due to poor occlusion, face sleeping, abnormal swallowing, thumb-sucking, and other abnormal habits. It seems that nature intends the protective covering of teeth (enamel) to last a lifetime (100 years) because there are no provisions for healing or regeneration.
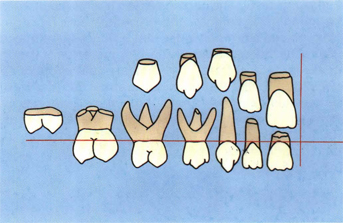
Fig 5-22 The genetic morphology of young unworn permanent crowns is sharp and complete in every detail before eruption into the oral cavity.
Occlusion refers to the act of closure or the state of being closed. We will first consider the state of being closed.
Centric relation (CR) = intercuspal position (IP)
Normal physiologic CR position of the jaws may be defined as the stable, comfortable, functional craniomandibular relationship in which the condyles are in their most superior position in intimate contact with the thinnest central bearing area of their respective discs against the distal surface of the articular eminences at any vertical rotational position of the mandible (Fig 5-23).
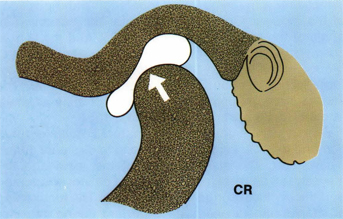
Fig 5-23 The normal physiologic position of the condyles in CR is in their most superior position in intimate contact to the thinnest portion of the biconcave discs at the most posterior slope of the articular eminences.
CR is a comfortable physiologic work position during mastication and swallowing, provided there are no deflective interferences from the teeth. CR is not a rest position; therefore, considerable electromyographic activity may be observed when the mandible is in the CR position. In dentitions in which IP = CR, CR is used during mastication and swallowing (and other random contacts of the teeth, including occasional clenching) about 5,000 times each day (Fig 5-24). The CR position has been found clinically to be the best location for maximum intercuspation of the teeth.5–7 Whenever IP does not occur at CR (centric occlusion or habitual occlusion) there are always posterior occlusal interferences in lateral border jaw movements with subsequent avoidance patterns.8
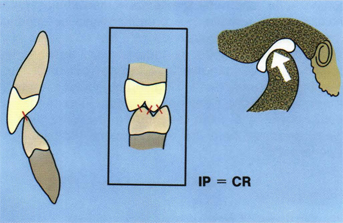
Fig 5-24 All of the teeth in the mouth should occlude evenly (IP) when the condyles are in CR position.
Clinical CR position may be simply defined as the completely retruded position of the mandible with the condyles in their most superior anterior position at any vertical rotational position of the mandible. Clinical CR does not require normal disc or condyle morphology or position. Clinical CR can be used as a treatment position when it has proven to be a stable, comfortable, repeatable position for the patient.
In good occlusion all of the teeth in the mouth make simultaneous contacts (IP) in CR including the anterior teeth (see Fig 5-24). However, the anterior teeth should never contact harder than the posteriors or fremitus may be produced with possible endodontic and periodontal trauma and/or interproximal separation of the teeth. Good posterior crown morphology and proper anterior overbite reinforces the integrity of the bi-concave discs of the temporomandibular joints each time the teeth are brought together in full occlusion in CR (about 5,000 times a day). This IP-CR relationship not only helps stabilize the condyle disc complex in CR position in the fossae but also helps maintain total craniomandibular stability.
Normally, occlusal contacts on the anterior teeth in CR are not broad, but rather two or three spots per tooth on the incisors and one on each canine (Fig 5-25).
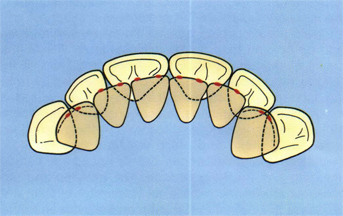
Fig 5-25 IP contacts on the anterior teeth should average about two for each tooth.
In good natural dentitions one rarely observes the actual cusp tips of posterior teeth making occlusal contacts. Instead, the contacts are usually found on cusp ridges and mesial and distal marginal ridges (Fig 5-26). Occlusal contact spots are small in good natural dentitions. The total tooth contact area has been estimated to be about 4 mm2 for the entire mouth, including all of the anterior and posterior teeth.9 The ideal contact location for the buccal cusps of the lower premolar is on the mesial and distal marginal ridges of the opposing premolars (cusp to marginal ridge).10 The contacts are just anterior and posterior to the point of the cusp on as they touch the marginal ridges of the upper premolars (Fig 5-27). This location allows for the maxillary canine to be in the embrasure distal to the mandibular canine (Class I) for maximum vertical guidance in lateral chewing. There is seldom, if ever, an occlusal contact with the rudimentary lingual cusp of the lower “second canine” (first premolar). Tripodization of mandibular buccal cusps and maxillary lingual cusps is rarely seen in natural occlusions. Tripodization is permissible in artificial crown occlusion provided the naturally sharp anatomic vertical profiles of the teeth are not violated. Cusp–fossa (moderate Class II) relationship is sometimes necessary for posterior artificial crowns (Fig 5-28). With cusp fossa relationship there is a tendency to produce flatter artificial cusp forms than in cusp-marginal ridge relationship because of poor tooth position and lack of interocclusal space. In any event, the common denominator in the posterior region in good natural dentitions seems to be: unworn (sharp) posterior tooth forms that occlude evenly in CR with small contact points (16 to 32 per side). The maxillary lingual cusps and mandibular buccal cusps occlude in opposing fossae or on mesial and distal marginal ridges or on cusp ridges.
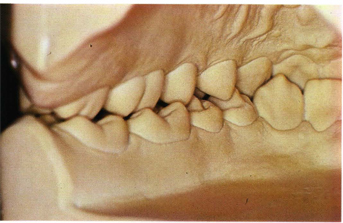
Fig 5-26 A lingual view of casts with normal posterior occlusal relation. Note the large embrasures and spaces. Also note that the rudimentary lingual cusps of the mandibular first premolar has no occlusal contact.
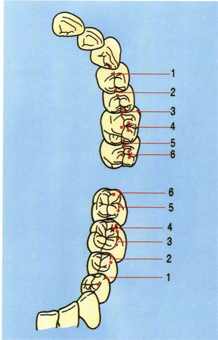
Figure 5-27a
Fig 5-27a In a normal Class I relationship, the buccal cusps of the mandibular premolars contact the marginal ridge of the maxillary premolars (cusp to marginal ridge). The mesiobuccal cusp of the first mandibular molar occludes on the adjacent marginal ridges between the maxillary first molar and second premolars while the distobuccal cusp of the mandibular first molar occludes in the central fossa of the maxillary first molar.
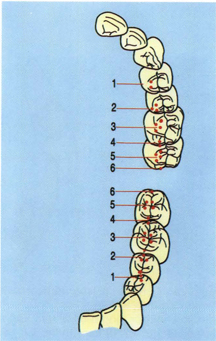
Figure 5-27b
Fig 5-27b In a normal Class I relationship, the lingual cusps of the maxillary premolars occlude on the marginal ridges or in the distal fossae of the mandibular premolars. There is usually no occlusal contact with the rudimentary lingual cusp of the mandibular first premolar. The mesiolingual cusp of the maxillary first molar occludes in the central fossa of its mandibular mate while the distolingual cusp occludes on the adjacent marginal ridges between the mandibular first and second molars.
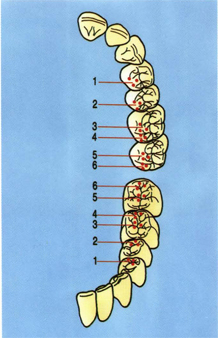
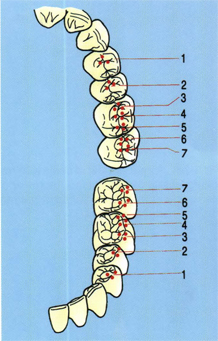
Fig 5-28 Cusp-fossa occlusal arrangement (moderate Class II) is sometimes necessary. However, care should be taken not to sacrifice natural tooth morphology in these cases. (left) The contacts of the maxillary lingual cusps shown against the mandibular teeth; (right) the contacts of the mandibular buccal cusps against the maxillary teeth.
Complete occlusion of the teeth (IP) is a specialized articulation of the craniomandibular system and can have a profound effect on the alignment and stability of the total craniomandibular articulation complex, including the maxillary and temporal bones as well as the temporomandibular joints. Full contact of all the teeth in the CR position of the condyles approximately 5,000 times per day helps to realign and stabilize the craniomandibular relationship into a state of biological equilibrium. This stabilization includes not only the teeth and temporomandibular joints but also affects other cranial articulations (sutures) in the skeletal system through the muscles. Stabilization of the craniomandibular relation in CR is important to the comfort, function, and longevity of dental restorations. The use of a properly constructed, adjusted, and maintained maxillary, anterior guided occlusal splint is probably the best way to align and stabilize the craniomandibular relationship prior to treating the occlusion and articulation of the teeth.
Anterior overbite
In well-related teeth the vertical overbite of the maxillary central incisors ranges from 4 to 5 mm when the teeth are in full occlusion (Fig 5-29). The horizontal overbite of the maxillary incisors is between 2 and 3 mm in full occlusion (see Fig 5-29). The incisal edges of the mandibular incisors contact the deepest portion of the lingual fossae of the maxillary incisors where the cingulum begins (Fig 5-30). The distobuccal convexity of the mandibular canine fits into the mesial lingual concavity of the maxillary canine. There is about 4 to 5 mm of vertical overbite of the canines. The natural convexity of the mandibular canine as it fits into the lingual concavity of the maxillary canine causes a rapid diminishing of the horizontal overbite (Fig 5-31). The horizontal overbite of the maxillary canines is much less than the incisors (about 1 mm) from the tip of the cusp to the labial surface of the mandibular canine (Fig 5-32).
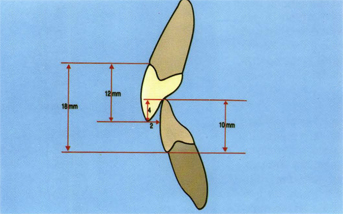
Fig 5-29 Central incisor vertical overbite averages about 4 mm with a 2- to 3-mm horizontal overbite. With an average maxillary incisor length of 12 mm and an average mandibular incisor length of 10 mm, there will be approximately 18 mm from upper cementoenamel to lower cementoenamel junction.
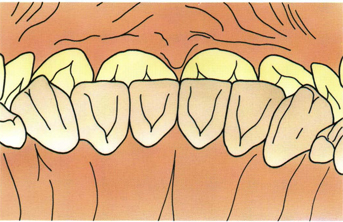
Fig 5-30 In full occlusion the incisal edges of the mandibular teeth touch the deepest portion of the lingual fossae of the maxillary incisors near the cingulum.
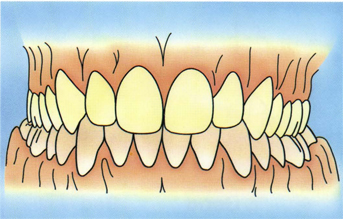
Fig 5-31 Horizontal overbite of the canines is minimal.
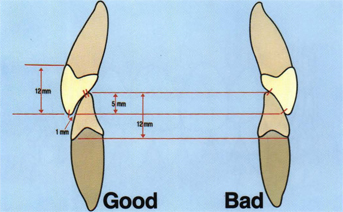
Fig 5-32 Horizontal overbite of the canines is usually less than 1 mm. However, there should not be large, flat surface contacts of the canines in IP.
In full occlusion the lower lip and upper lip rest against the labial surface of the maxillary incisors. The lower lip helps retain the maxillary teeth against the mandibular anterior teeth while the tongue holds the mandibular incisors against the maxillary incisors in a state of equilibrium, sometimes referred to as the neutral zone (Fig 5-33). This lip-tooth-tongue relationship helps produce a negative pressure seal during mastication and swallowing as well as stabilization of teeth positions.
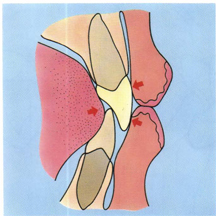
Fig 5-33 The lower lip as well as the upper lip should both be supported by the maxillary teeth when the teeth are in IP. During swallowing the pressure of the lips and the counter-pressure from the tongue help to stabilize the positions of the anterior teeth (arrows).
Maxillary and mandibular arch forms should be of adequate size to conform to each other and support normal size teeth without crowding. It is best if the arch midlines be coincidental with each other as well as the midsagittal plane of the patient’s head so that proper incisive and canine guidance and esthetics can better be achieved (see Fig 5-31). If any compromise with the midline is to be made in dental treatments, it should be with the mandibular midline rather than the maxillary midline.
“Rest position” and “free way space”
Most of the time (22 hours per day) the mandible is not in the CR position but is in a rest or semirest position with the anterior teeth separated anywhere from 1 mm to as much as 10 mm. The condyles do not remain in the deep portion of the fossae (CR) when the mandible is in various relaxation postures but are usually 1 to 2 mm forward on the eminentia (Fig 5-34). During enunciation of certain words (eg, S sounds), the condyles are usually forward down the eminentia about 2 to 3 mm from CR, depending on the amount of anterior horizontal overbite (Fig 5-35). The incisor horizontal overbite of 2 to 3 mm is important because it allows for this forward posturing of the mandible to take place comfortably without the feeling of mandibular confinement. However, the 2- to 3-mm horizontal overbite required in the incisors is not needed in the canines because normally the jaw does not move laterally during the periods of relaxation or speaking. If the incisor horizontal overbite exceeds 3 mm, there is a chance that the lower lip may be pulled up under the maxillary incisors, causing labial tooth migration and poor esthetics with the lips. The free way space used during speaking averages about 1.7 mm. Free way space is learned and, if anterior tooth relationships are changed, requires new learning but usually returns to about 1.7 mm in a short period of time.
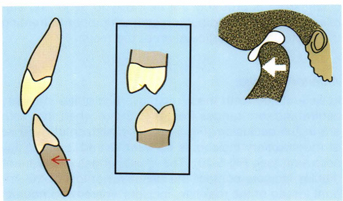
Fig 5-34 In rest positions the condyles do not remain in the CR position but are forward and the teeth are separated.
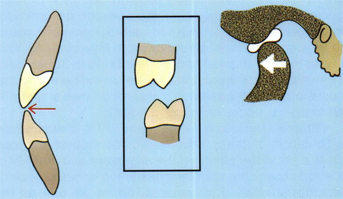
Fig 5-35 In normal speaking positions of the “S” sounds, the condyles are forward to CR and there is a very close position of the incisal edges of the anterior teeth with a larger space between the posterior teeth.
Vertical dimension of occlusion
It has been commonly believed and taught in prosthodontics for many years that vertical dimension of occlusion is critical. It was considered that, because of muscle length, free way space, and rest position, one should never increase occlusal vertical dimension (OVD). It was also believed that passive eruption of the teeth kept the OVD at its original level in worn dentitions and that if OVD was increased it ‘would gradually return to the worn-down position.11
The author, however, has been increasing OVD for more than 30 years with restorative dentistry, orthodontics, and orthognathic surgery, and has had no problems with rest position or free way space.12 The free way space returns to about 1.7 mm following the increase of OVD in these patients. Cephalometric radiographs 5 and 10 years posttreatment show that the increased distance between nasion and menton is not being lost.
Garnick and Ramfjord13 found that the interocclusal distance (free way space) averaged 1.7 mm in the clinically determined rest position, whereas the average distance was 3.29 mm with an additional resting range of 11 mm when determined electromyographically on the basis of minimal muscle activity. He stated that determining clinical rest position also involves the influence of emotional and exteroceptive and proprioceptive inputs to the neuromuscular system. Such input from joints, muscles, lips, tongue, cheeks, mucosa, teeth, and periodontal membrane undoubtedly contribute to the learning of rest position or conditioning of reflexes. Concepts regarding rest position of the mandible should be reevaluated and revised in light of the recent research and clinical experiences. When changing OVD in restorative dentistry, excellent anterior guidance and posterior crown morphology should be established to CR position of the condyles. The improved anterior and posterior guidance helps the patient form learned ingrams in the cerebral cortex for the new chewing patterns at the restored OVD.
There is a limit to the amount one can increase OVD. It appears, however, that the range is large (up to 10 mm on some people) and that OVD is one of the least critical factors in rehabilitating the occlusion. In restorative dentistry there is no advantage in increasing OVD more than is necessary to obtain good crown morphology on anterior and posterior teeth. If the anterior teeth are unworn and OVD is increased, it usually requires orthodontics or orthognathic surgery to obtain good anterior relations.
Development of occlusion
With the growth of the infant and the eruption of the teeth into the oral cavity, afferent stimuli from receptors in the periodontal membrane, lips, tongue, cheeks, mucosa, and temporomandibular joint influence the central nervous system and, reflexively, the position of the mandible (Fig 5-36). With the eruption of the teeth the process of mastication is learned, and learning depends upon the cerebral cortex.14 In other words, mastication is not part of the autonomic nervous system, similar to swallowing. Wickwire and Gibbs15 reported that the chewing patterns of young children with primary dentitions are generally wide. When the permanent teeth erupt into the oral cavity they begin establishing the in-grams for more vertical chewing patterns. The 6-year molars are the first guide teeth in establishing adult lateral chewing patterns. If the child (6 to 12 years) is fortunate enough to develop good relationships of the teeth, learned reflexes develop by which the mandible functions more vertically as the mandibular teeth approach the maxillary teeth in the final portion of the chewing cycles. When tooth morphology and/or tooth position is restored or changed, new ingrams for occlusion must be developed in the central nervous system. These new learned reflexes are not always immediate and may take longer for some people. There are five guidance factors involved in occluding the teeth: (1) anterior teeth, (2) posterior teeth, (3) right condyle path, (4) left condyle path, and (5) neuromuscular mechanism (cerebral cortex). Research shows that the teeth are the primary factors in jaw closing patterns and that teeth frequently make contact during mastication and swallowing.16–19 However, if tooth relationships do not allow for proper condylar positioning with the disc or if the teeth inhibit condylar movements, they can cause traumatic occlusion. Traumatic occlusion may be defined as any closures of the teeth that produce visible or invisible unphysiologic stress, damage, or overload to the teeth, joints, muscles, bones, periodontium, or nervous system.
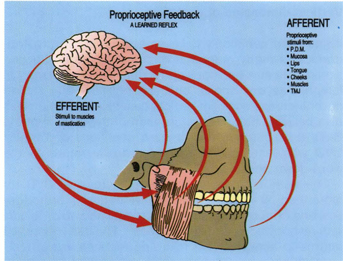
Fig 5-36 In addition to the pressoreceptors in the periodontal ligaments, there are many other components of the gnathic system, including the lips, tongue, cheeks, mucosa, skin, muscles, and temporomandibular joints, which contain proprioceptive bodies. These proprioceptors continuously monitor the position of the mandible and feed the information to the brain. The brain, in turn, tells the muscles how to move the mandible. Good chewing patterns are placed on a learned reflex level provided the teeth have good morphology and proper positions.
Traumatic occlusion is evidenced by the following: (1) abrasion and fracturing of teeth, dental restorations, and prostheses; (2) craniofacial pain (myalgia); (3) craniomandibular dysfunction (temporomandibular joint, TMJ); (4) tooth migration; (5) tooth mobility; (6) overload on the periodontium; and (7) exostoses (overload).
There are several basic identifiable interferences that can cause traumatic occlusion:
1. Centric relation: slide (anterior, lateral) and fulcrum.
2. Protrusive–retrusive, incisive.
3. Lateral border: nonworking side and working side.
Of the centric interferences, the fulcrum type is probably the more traumatic because the condyle is continually distracted from the disc during mastication and swallowing, often leading to disc derangements because the disc is unsupported, whereas with a slide the condyle is engaged with the concave portion of the disc during mastication and swallowing. Of the border interferences, those on the nonworking side are usually most disturbing to the neuromuscular system, often resulting in excessive wear on anterior teeth due to avoidance patterns. In addition to occlusal interferences, the presence of flat (unnatural) occlusal morphology in artificial crowns and natural teeth is also a cause of traumatic occlusion through overload.
Original natural tooth morphology per se is not the cause of traumatic occlusion (except perhaps in connection with microdentia, enamel aplasia). It is the relationship of the mandibular teeth to the maxillary teeth as the jaws close (in function and nonfunction) that creates the majority of problems in occlusion. Some of the poor relationships of the teeth are due to skeletal disharmonies connected with growth and development, poor posturing, abnormal habits, and so on. Other bad relationships of the teeth may be caused by lost teeth and subsequent tooth drift, worn teeth, or iatrogenic causes, such as flat artificial crowns, poorly carved restorations, high crowns and fillings, and improper orthodontic treatment.
Considering the fact that normal chewing function and parafunction (when viewed in the horizontal plane) take place within a small diamond-shaped area, only 3 mm to the right, 3 mm to the left, and 3 mm forward to intercuspal position, it should be no surprise that small changes or discrepancies (0.1 mm or less) in the occlusion can have serious effects (Fig 5-37).
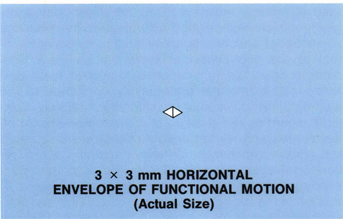
Fig 5-37 Actual size of functional mandibular movement in the horizontal plane takes place within a small diamond-shaped area only 3 mm to the right and to the left and forward.
Anterior tooth guidance
Anterior guidance is generally recognized as an important aspect in present-day concepts of occlusion.20–22 This guidance is of two types: (1) incisal guidance in protrusive–retrusive movements and (2) canine guidance in mediotrusive lateral movements. The primary importance of protrusive guidance is for proper incising as well as rest positions and speaking function. The primary importance of canine guidance is to help prevent lateral eccentric posterior tooth interferences and allow the condyles to move uninhibitedly along their border pathways in the fossae as well as guiding jaw closures more vertically to load the posterior teeth in their long axis.
Scientific guidelines have not been established as to how much the anterior overbite should be. Orthodontics has generally advocated an arbitrary amount of about 1.5 mm of vertical overbite. The term “cuspid disclusion” has been used by some dentists to describe canine function that separates the posterior teeth in lateral movements of the mandible. The word “disclusion,” however, is quantitatively ambiguous and can be used to mean as little as a few hundredths of a millimeter (Fig 5-38). Minimal “lift” on the canines usually disappears in a relatively short period of time (crowns at best acquire some wear in time). Minimal canine disclusion does not allow for in vivo functional physiologic factors, such as flexions and compressions of certain components of the gnathic system that result in posterior teeth coming into early premature lateral contact. The term also seems to imply that it is “normal” for the mandible to move from centric to eccentric positions with the teeth in contact. The term “cuspid disclusion” is inadequate to describe the potential physiologic guiding function of the canines. (It seems that the most physiologic way to “disclude” one’s teeth is to simply open the mouth.) “Canine guidance” is probably a more preferable term because it implies normal physiologic jaw functions.
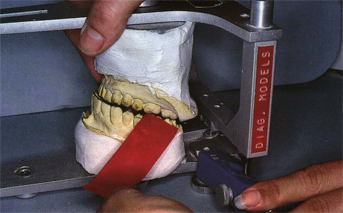
Fig 5-38 In the laboratory, “posterior disclusion” in lateral movement of the articulator can be accomplished with as little as a few hundredths of a millimeter of space between the teeth. This small space may not be adequate to keep the posterior teeth separated under functional loading (see Figs 5-80 to 5-83).
Some dentists have tried to relate the overbite of the anterior teeth to condyle movements on a direct basis. Some advocate the notion of making the incisal guidance 5° steeper than the condylar path (Fig 5-39) or contouring the lingual of canines to “harmonize” with the Bennett path of the condyles (Fig 5-40). This practice is not supported by observations of natural teeth and, if done, increases the chance of posterior eccentric interferences or requires the dentist to flatten the posterior crown morphology from its original natural form (Figs 5-41 a and b). Flattened occlusal posterior crown morphology causes more overload on the teeth and supporting structures.
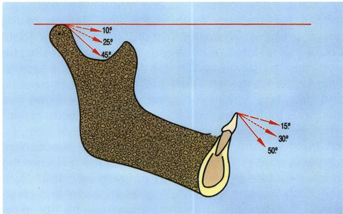
Fig 5-39 There is no scientific or clinical rationale for making incisal overbite with a minimal relation to the condylar path, as some suggest. If the notion that anterior overbite should be only 5° steeper than the condylar path, then one would have to make abnormally flat posterior teeth in the case of more horizontal condyle paths.
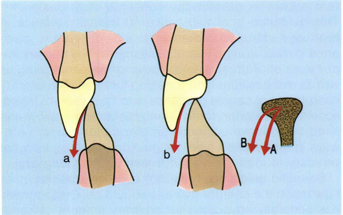
Fig 5-40 If one follows the notion of increasing the lingual fossa of a patient’s canines (b) to correspond to large amounts of condylar Bennett movement (B), then there would have to be abnormal (flat) posterior crown morphology to avoid lateral interferences. Flat occlusal morphology produces functional overload.

Fig 5-41a Compare the natural crown morphology to the unnatural morphology in Fig 5-41 b.

Fig 5-41b Note the abnormal flattening (low vertical profile) of the posterior artificial crowns because of the unnatural (poor) overbite of the canine.
Posterior tooth guidance
There has been a great deal of emphasis placed on canine guidance or disclusion since it was first postulated by D’Amico17 in the late 1950s. According to some authorities, the canine teeth should receive all eccentric tooth contacts in lateral border movements of the mandible.17,18,20 However, canine guidance is not the only factor of importance in medial guidance of the mandible. Young children in the most formative years of their lives (ages 6 to 12) have no canine guidance. It seems that if canines were the only teeth of vital importance in medial guidance of the jaw, nature would have placed these teeth early in the mouth. If the teeth are the primary guidance factors for occluding the teeth (which research shows), it is obvious that at age 6 it is the cusps of the 6-year molars that guide the lateral closures, followed later by the premolars (Fig 5-42). Finally, at about 12 years of age, the canines erupt into guiding function. Kawamura reported that even though the incisors are the most sensitive teeth to presoreception in the periodontal ligament, the posterior teeth are also extremely sensitive.23 This posterior exquisite sensitivity can be demonstrated clinically on some patients with mylar occlusal ribbons that are only 0.01 mm thick.
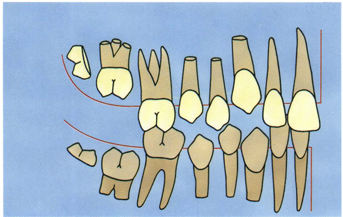
Fig 5-42 In the most formative years of life (6 to 12 years), nature provides only posterior tooth guidance in lateral movements.
Perhaps the best rule to follow in treating patients is to simulate the tooth relationships found in untreated, nontraumatic, long-lasting natural dentitions. Observations of these people show the following:
1. Good masticating and swallowing function.
2. Minimal wear on the teeth.
3. Minimal stress on the TMJ.
4. Minimal stress on the periodontium.
5. Comfortable muscle activity.
6. Good esthetics.
These people have anterior teeth with similar characteristics. The crowns of maxillary central incisors are relatively large and long, the lateral incisors are shorter and rounded mesiodistally on the incisal edges, and the canines are long and pointed (Figs 5-43c, 5-44a, and 5-45a). The vertical anterior overbite ranges from 3 to 5 mm and the horizontal overbite of the incisors ranges from 2 to 3 mm. The horizontal overbite of the canine teeth is less than 1 mm. These patients also have relatively unworn posterior teeth with sharp occlusal morphology, which is compatible with their naturally steep canine guidance (65° to 70°). The IP of the teeth is less than 0.5 mm from the CR position of the condyles. They usually have few dental restorations, especially artificial crowns. These patients show 2- to 3-mm spaces between their posterior teeth when they touch the incisal edges of their mandibular incisors or canines against the maxillary anterior teeth (Figs 5-43b and c, 5-44b and c, and 5-45b and c).

Fig 5-43a A 36-year-old woman with nontraumatic natural occlusion showing large central incisors, short rounded lateral incisors, and long pointed canines.
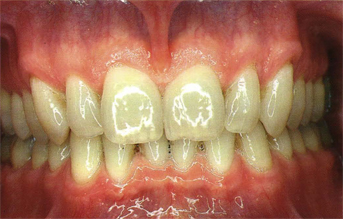
Fig 5-43b A 55-year-old man with nontraumatic natural occlusion showing large central incisors, short rounded lateral incisors, and long pointed canines.

Fig 5-43c An 85-year-old man with nontraumatic natural occlusion showing large central incisors, shorter lateral incisors, and long canines. Note the attrition on the incisal edges of all of his anterior teeth.

Fig 5-44a

Fig 5-44b

Fig 5-44c
Figs 5-44a to c The same three patients as in Figs 5-43a to c, respectively, in an edge-to-edge incising position. Note that the incisal edge of the maxillary central incisors meets the incisal edges of the mandibular four incisors. The maxillary lateral incisors are higher on the incisal edges to make space for the cusp tips of the mandibular canines. There is a space of 2 to 3 mm between the posterior teeth cusps.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


