Chapter 5
Crescentic flap
Introduction
Webster published the first description of the crescentic perialar flap in 1955.1 Since then the crescentic flap technique has been used in many forms and with various descriptors.2-4 The basic rationale for this flap is the removal of tissue in the form of a crescent in the perialar or chin region, which then allows for the advancement of the surrounding tissues to repair an adjacent defect. This technique finds a unique niche in the repair of both upper and lower lip defects. The crescentic flap enables reconstruction of defects that would otherwise require the use of cross-lip flaps or other less elegant options.
The main advantage of using the crescentic flap is that it enables repair of the defect with minimal tissue distortion. The placement of the incision gives a less conspicuous final scar.5 Further, the use of the perialar crescentic flap to repair either upper or lower lip defects, preserves the oral sphincter.
The repair of the lip is addressed in detail in Chapter 22.
Anatomy
The anatomy as it relates to the use of the crescentic flap depends on the site where the defect is located.
The most common sites for crescentic flap repair are the upper lip or the lower lip. In cases where the defect is located in the lower lip, the anatomical area of interest will be the perialar tissues and the upper lip itself. The area of the perialar zone is an intricate anatomical region. The subtleties of the area of the nasal sill and the upper lip allow for an easy cosmetic alteration and therefore the potential for a less than ideal result. The blood supply for a flap in the alar region (i.e., the perialar crescentic flap) is the superior labial artery and the facial artery. The veins are the accompanying veins. The mobilized flap will be a portion of the upper lip supplied by the superior labial artery and vein as well as a portion of the cheek, which will be advanced medially to restore the missing tissue; thus, the facial artery and vein are the blood supply to this portion of the flap.
In cases where the flap is being used to repair of lower lip defects, the anatomical area of interest will be the area lateral to the labiomental crease. The blood supply to the portion of the lip to be mobilized is the inferior labial artery and vein and the tissues lateral to the defect site are supplied by branches from the facial artery and vein as well as the mental and submental arteries and veins.
Flap harvest
Perialar crescentic flap
- The area of the upper lip defect is measured to determine the width for the excision (Figure 5.1).
- The width is then drawn along the floor of the nose and laterally along the ala of the nose in the shape of a crescent (Figure 5.2).
- The greatest width of the crescent is equal to the width of the defect. If the width is determined to be too large, the width is divided in half and distributed to either side of the perialar region.
- The design of the perialar crescentic flap enables advancement of the cheek into the missing upper lip defect without distorting the nose.
- In cases where the defect extends below the ala of the nose to potentially undermine the support of the nose, this is taken into account when excising the crescentic area and only the skin in this area is removed, so support is provided under the nose and ala.
- Once the crescent is drawn, a full thickness excision of the area crescent is performed (unless nasal ala support is needed) (Figures 5.3 to 5.6).
- The mucosa is incised along the buccal vestibule and the path of the predicted advancement.
- The remaining lip and cheek is then advanced into the defect.
- The area is then closed in layers with first reapproximation of the orbicularis muscle (Figure 5.7).
- The mucosa is closed along the vestibule and the lip.
- Deep sutures are placed along the ala of the nose and the nasal sidewall.
- The final closure is that of skin.
- The final outcome is often very pleasing with minimal evidence of the donor site while preserving the oral sphincter (Figures 5.8 to 5.11).
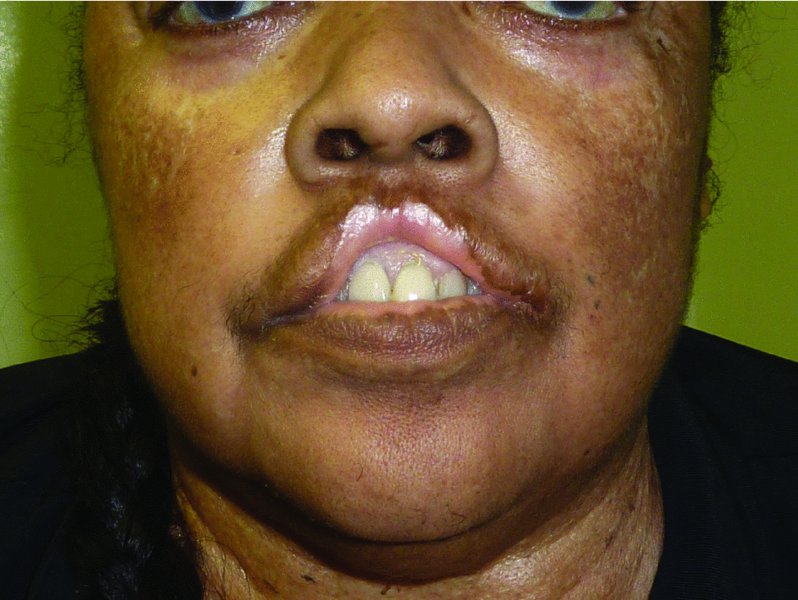
Figure 5.1 Appearance of the upper lip after loss of the central/philtral unit.
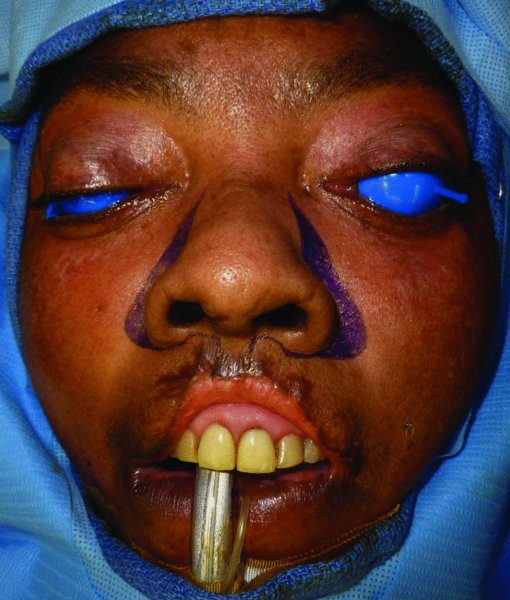
Figure 5.2 Markings for bilateral crescentic flaps.

Figure 5.3 Excision of bilateral perialar tissue to allow for advancement of bilateral upper lip flaps.

Figure 5.4 Closer view of the excised tissue and developed flaps.

Figure 5.5 Lateral view of the flap. Note that the excision is extended to the anterior wall of the maxilla.

Figure 5.6 Contralateral view of the flap.

Figure 5.7 View after bilateral advancement of the flaps.

Figure 5.8 Early postoperative view. Note that the central defect has been eliminated.

Figure 5.9 Late view of the healed upper lip after bilateral crescentic flaps.

Figure 5.10 Note that there is no restriction in mouth opening.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


