Chapter 5
Aesthetic restorative materials
There are many different types of aesthetically sound restorative materials available. The operator must choose the most suitable materials based on durability, cost, fluoride-releasing properties, aesthetics, chairside time and ease of use.
RESIN COMPOSITE
A resin composite material, by definition, is a material made from two or more substances (see Composition below). Resin composite materials have a number of clinical applications.
There are many types of resin composites on the market. The characteristics of some them are shown in the chart given below:
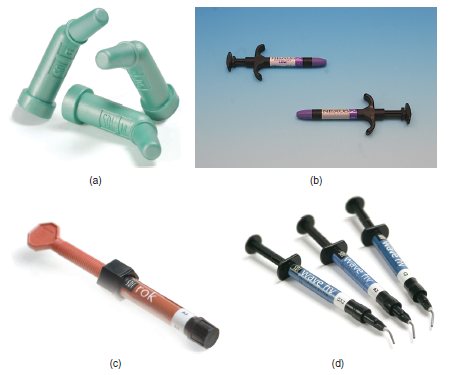
| Dispensing options | Curing options | Flowability options |
| • Single use compule form (Figure 5.1a) | • Dual cure | • Flowable resin composites |
| • Two-paste system (Figure 5.1b) | • Self-cure | • Packable/condensable resin composites |
| • Syringe form (Figure 5.1c and 5.1d) | • Light cure | •Hybrid materials |
| • Nanofilled |
Figure 5.1 (a) Single-use compule. (b) Two-paste system. (c) Syringe form. (d) Syringe form.
Resin composites may be used in conjunction with acid etch, primers and bonding agents. The manufacturer’s instructions for use should always be followed, as these may depend on each individual product.
Material constituents/composition
Resin composites consist of an organic resin, reinforcing filler and a coupling agent. The resin allows resin composite to be moulded and set by polymerisation (light or chemical curing); the filler contributes to the strength and hardness of the material; and the coupling agent binds the components together. Different types, sizes and shapes of fillers (powdered glass, quartz, ceramic particles and silica) affect the characteristics of individual resin composites.
There are various classifications of resin composite materials. Particle size varies between the types of resin composites. It can be classified into fine, microfill or a combination of both, which are referred to as ‘hybrid’ and, most recently, nanofilled.
Properties
- Strong
- Wear resistant
- Less durable than amalgam, but more aesthetically pleasing
- Used in conjunction with acid etch (phosphoric acid solution), primer and bonding agent
- Placed in increments with polymerisation (light curing) in between to ensure the curing of all layers and to reduce the opportunity for shrinkage
- Less dense than amalgam
Advantages
- Aesthetically pleasing
- Working time of light-cured resin composite can be operator controlled
- Strong
- Mechanically bonds to the tooth structure
- Operator can be conservative during restorations (due to mechanical bond)
Disadvantages
- It is not condensable or packable (this includes posterior composite materials in the true sense of packable)
- Technique sensitive (follow the manufacture’s instructions for specific product specifications and usage)
- Shrinkage upon polymerisation
- Time consuming (takes approximately three times longer than placing an amalgam restoration of comparable size)
- Does not release fluoride
- Moisture intolerant
- Tends to ‘stick’ to dental instruments; may require use of special dental instruments
Indications and contraindications for use
Indications
- Permanent restorations – especially on anterior teeth
- Core buildups
- Temporary/provisional restorations
- Direct veneers
- Class I, Class II, Class III, Class IV and Class V restorations
- Specially formulated resin composite materials are available for Class II posterior applications
Contraindications
- Not to be used with cavity varnish (prevents adhesion)
- Unsuitable for use where it may be difficult to maintain good moisture control
- Patients with grinding (bruxism) habits
- Replacement of posterior cusps (due to high load, which increases risk of wear and fracture on resin composite)
- Large restorations on posterior teeth (the larger the restoration, the greater the polymerisation shrinkage)
- Deep restorations extending subgingivally (difficult to achieve good marginal seal and effective moisture control)
Trade names
| Trade name | Manufacturer | Usage |
| EsthetX Flow ® | Dentsply | Flowable resin composite |
| FiltekTM Supreme | 3M ESPE | Nanofilled |
| Glacier (Figure 5.2a) | SDI | Anterior and posterior restorations |
| Herculite® (Figure 5.2b) | Kerr | Small particle hybrid (anterior and posterior restorations) |
| Ice | SDI | Various usages |
| IntegrityTM | Dentsply | Temporary/provisional restorations |
| P60TM | 3M ESPE | Packable/condensable resin composite |
| RevolutionTM (Figure 5.2c) | Kerr | Flowable resin composite |
| Rock | SDI | Posterior restorations |
| SurefilTM | Dentsply | Packable/condensable resin composite |
| Tetric | Ivoclar | Different types available for different usages |
| Wave (Figure 5.2d) | SDI | Flowable resin composite |
Figure 5.2 (a) Glacier – SDI. (b) Herculite® – Kerr. (c) RevolutionTM – Kerr. (d) Wave – SDI.

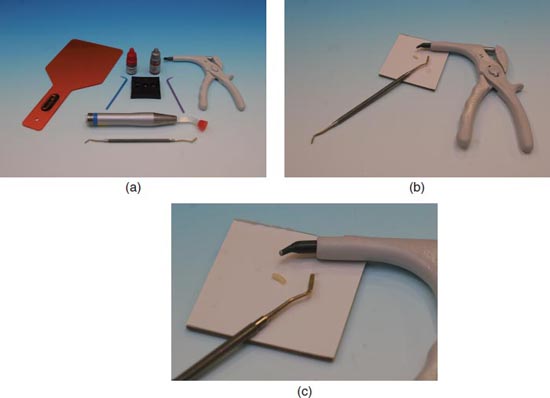
Manipulation (Figures 5.3a–5.3c)
Wearing personal protective equipment:
Figure 5.3 (a) Resin composite set-up. (b) Step 3 – resin composite dispensed. (c) Step 4 – resin composite ready for transfer to the operator.
Follow the manufacturer’s instructions for storage of resin composite material. Most products are best stored in the refrigerator and brought to room temperature prior to use.
- The operator will administer local anaesthetic, if indicated
- Pass the operator the shade guide for shade selection (using a natural light source) of the tooth/teeth being treated (prior to drying of the teeth)
- Tooth is appropriately prepared and isolated, and if liners, bases and bonding agents are needed, they are applied prior to resin composite placement
- Prepare the tooth for resin composite placement using operator’s choice of acid etchant and bonding system (see Chapter 6)
- The choice of delivery system for resin composite will determine dispensing instructions
- If using the two-paste system, dispense equal lengths of both the catalyst and base on the waxed paper pad, taking care that they do not touch. When requested, mix them together (mixing time: 30 seconds) with a plastic mixing spatula until a uniform colour is reached
- Both compule and syringe type resin composites can be added directly to the preparation (ensure the cap(s) is replaced after placement, as the material is light sensitive)
- Resin composite may be added directly over the bonding agent and needs to be added incrementally (2mm) to ensure complete polymerisation of each increment and to reduce the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


