Chapter 5 Aesthetic problems
The meaning of an aesthetic problem is vague as perfectly normal looking teeth can appear unacceptable to a patient. So the first stage in any assessment is to determine with the patient what the problem is and to assess what can be done. This chapter details the specific aesthetic problems a patient may present with and some simple solutions to address some of these, such as direct composite additions and vital and non-vital bleaching. Chapter 15 revisits some of the issues raised in this chapter and addresses how optimum aesthetics can be created in indirect restorations and describes in detail aspects such as tooth shaping and correct shade matching.
Causes of aesthetic problems
The shape and size of teeth
The teeth that are visible for most patients are the upper canines and incisors; however, in some patients, premolar teeth or even molar teeth are visible when the patient talks and smiles. The position of the lips in the extreme natural position of smiling is called ‘the smile line’ by many prosthodontists. The visible shape of teeth consists of the length, width and their relationship to other teeth. Generally, upper incisors are about 1 cm long and have a width between 0.75 and 0.80 cm (Figure 5.1). Although these dimensions vary considerably, teeth made too wide or too long appear unnatural (Figures 5.1 and 5.2). Therefore, as a base line, knowing the average tooth length and width can be useful in determining what is abnormal and what can be done to teeth in the smile line (see Chapter 15 for creating the ideal aesthetics and average tooth dimensions).

Figure 5.2 The addition of composites to the patient in Figure 5.1 has widened the teeth beyond an acceptable level, leading to less than ideal aesthetics.
The other important criteria in an assessment of the smile line are the gingival contours, particularly along the margins of the upper anterior teeth. For some patients the smile line is low and the gingival margins are not visible; thus aesthetic anomalies are therefore relatively unimportant. In others, the smile line is high and gingival margins are clearly visible, variations from the norm having a high impact (Figure 5.3). In health, the gingival margins of the canines and central incisors are normally at the same horizontal level and more apical to the lateral incisors (Figure 5.4). The incisal edges of the upper central incisors and the tips of the canines are also usually at the same approximate level but the lateral incisors are normally slightly shorter. The horizontal line along the incisal edges from the incisors to the canines is normally convex and follows the line of the lower lip (Figure 5.5).
Colour of teeth
A frequent patient complaint regarding dental aesthetics is that teeth tend to discolour or darken with increasing age. The reason for this change is believed to be caused by the gradual thinning of enamel from tooth wear. As the enamel wears, the darker dentine shines through and becomes more dominant in the colour of the teeth. An unacceptable colour is personal and subjective. What might appear to be a perfectly normal colour may be unacceptable to a patient. A common example of this is the colour of the canine tooth (Figure 5.6). Naturally, this tooth has a higher saturation of the colour yellow than other incisor teeth and the difference in colour is unacceptable for some patients.
Occasionally, more serious discolorations of teeth present. This may be a result of fluorosis (Figure 5.7) or tetracycline staining (Figure 5.8). The former can present in patients born overseas where there is a high fluoride content found naturally in spring water, or those given too high a dose of fluoride during tooth development. Our understanding of the action of fluoride is now clearer and the most important preventive effect is from its topical application, systemic fluoride supplements such as drops or tablets are rarely given today due to the disfiguring white and brown mottled defects that can occur (Figure 5.7).
Tetracycline staining is very unlikely to occur to someone born in the UK as the disfiguring side effect of tooth discolouration is well known (Figure 5.8), hence it is rarely given to children during tooth development. For those born outside the UK the chances of developing tetracycline staining will depend on the availability of the drug over-the-counter. In some parts of Asia, for example, drugs which would be prescription delivered in the UK are available over-the-counter and this is particularly true of antibiotics. Tetracycline staining can be clearly distinguished as the teeth fluorescence under ultraviolet light.
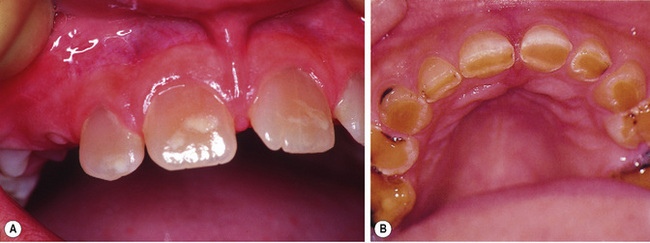
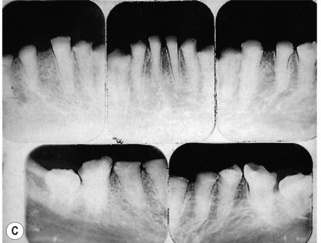
Genetic disorders such as dentinogenesis and amelogenesis imperfecta also affect tooth development, with both having varying impact upon the teeth. Mild forms of either condition can be difficult to distinguish but more severe forms are characteristic and differentiated by the anatomy of the roots. In dentinogenesis imperfecta there are bulbous roots with root canal obliteration which are visible on radiographs (Figure 5.9), whereas teeth with amelogenesis imperfecta have normal root formation but abnormal enamel development.
Dentinogenesis imperfect (Figure 5.9) is inherited as an autosomal dominant trait, with one parent usually having the condition. The disorder is the result of a defective DSPP (dentine sialophosphoprotein) gene. Three types have been identified: Type I is associated with osteogenesis imperfecta, whilst Type II (some have progressive hearing loss) and Type III are not associated with other inherited disorders and some believe they form a single disorder. It can affect both primary and permanent dentitions. The crowns of teeth affected by dentinogenesis imperfecta appear blue–grey or yellow–brown and translucent; the condition has also been referred to as hereditary opalescent dentine. The defective dentine leads to early loss of the enamel and rapid wear.
Numerous forms of amelogenesis imperfecta have been described based upon the appearance of the teeth and the way in which the disorder is inherited; most cases are inherited as an autosomal dominant trait. Amelogenesis imperfecta results from mutations in the genes that are responsible for the production of proteins that are important in the formation of enamel. It can also affect both primary and permanent dentitions. The teeth are usually discoloured with a pitted or grooved appearance and can break and wear down rapidly (Figure 5.10). Some forms of amelogenesis imperfecta can be difficult to distinguish from fluorosis (see Figure 5.7), as both conditions can lead to hypoplastic changes to the surface of the enamel.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses