CHAPTER 47
Surgical Management of the Neck
Anthony B.P. Morlandt1 and Jon D. Holmes2
1Department of Oral and Maxillofacial Surgery, University of Florida Health Science Center, Jacksonville, Florida, USA
2Clark Holmes Oral and Facial Surgery; and Department of Oral and Maxillofacial Surgery University of Alabama, Birmingham, Alabama, USA
Indications for Neck Dissection
A complex cervical lymphovascular system, containing approximately 300 lymph nodes (40% of the body’s estimated 800 nodes), drains the head and neck region. Cervical lymph node involvement in head and neck tumors is the single most important prognostic indicator, resulting in a 50% decreased overall survival and immediate classification as stage 3 or 4. Timely and appropriate management of at-risk cervical lymphatics therefore serves two critical purposes: to remove disease (macroscopic or microscopic) and to properly stage the neck, guiding adjuvant therapies based on histopathologic features. Neck dissection is indicated in nearly all cases of oral cavity cancer, although the extent and levels of dissection have evolved over the past four decades. In contemporary practice, neck dissections may be classified into two broad categories based on the therapeutic intent or purpose:
- Elective neck dissection is the removal of at-risk cervical nodal basins in a patient without clinically or radiographically evident cervical metastases.
- Therapeutic neck dissection is the removal of at-risk node-bearing tissues in the patient with clinically or radiographically evident neck disease.
Neck Dissection Classification
The first widely used classification system was presented in 1991 by the American Society of Head and Neck Surgery and was adopted by the American Academy of Otolaryngology—Head and Neck Surgery. This system was revised in 2002 and clarified in 2008 with respect to boundaries between sublevels. In 2011, Ferlito et al. proposed an updated, concise classification system based on three parts:
- Symbol ND with laterality indicated
- Specific lymphatic levels removed (Ia/b, IIa/b, III, IV, Va/b, VI, and VII)
- Specific nonlymphatic structures removed (sternocleidomastoid muscle [SCM]; internal jugular vein [IJV]; cranial nerve [CN] XII [hypoglossal nerve]; CN XI [spinal accessory nerve]; skin [SKN]; external carotid artery [ECA], etc.). (See Table 47.1.)
Table 47.1. Neck dissection classification systems
| Robbins et al. (1991) | Robbins et al. (2002/2008) | Ferlito et al. (2011) |
| Radical neck dissection | Radical neck dissection | ND (I–V, SCM, IJV, CN XI) |
| Modified radical neck dissection (preservation of CN XI) | Modified radical neck dissection (preservation of CN XI) | ND (I–V, SCM, IJV) |
| Selective (supraomohyoid) neck dissection | Selective neck dissection (SND I–III) | ND (I–III) |
| Selective (lateral) neck dissection | Selective neck dissection (SND II–IV) | ND (II–IV) |
| Extended neck dissection with removal of skin and hypoglossal nerve | Extended neck dissection with removal of skin and hypoglossal nerve | ND (I–V, SCM, IJV, CN XI, SKN, CN XII) |
Note: SCM, sternocleidomastoid muscle; IJV, internal jugular vein; CN, cranial nerve; CN XII, hypoglossal nerve; CN XI, spinal accessory nerve; SKN, skin; ECA, external carotid artery.
Relevant Anatomy
Neck dissection requires detailed knowledge of the anatomy of the entire neck, extending from the mandible to the clavicle and from the midline to the trapezius muscle. Selective neck dissection of levels I, II, and III (Figure 47.3) demands understanding the fascial layers enveloping the neck contents and the maneuvers necessary to “unwrap” the muscles to deliver an intact specimen.
Levels and key structures include the following (Figures 47.1 and 47.2):
- Level I
- Ia (submental): Extends from the mandible superiorly to the hyoid bone inferiorly, and is bounded laterally by the anterior bellies of the digastric muscles bilaterally. The submental artery will be encountered and must be preserved if the submental island flap is planned.
- Ib (submandibular): Bounded by the mandible superiorly to the anterior and posterior bellies of the digastric muscle anteroinferiorly, and the stylohyoid muscle posteriorly. The perifacial lymph nodes, facial artery and vein, and submandibular gland are encountered, as well as the marginal mandibular, lingual, and hypoglossal nerves.
- Level II (upper jugular)
- IIa: Includes the tissues bounded by the skull base superiorly, inferiorly by the hyoid bone radiographically and carotid bifurcation surgically, the stylohyoid muscle anteriorly, and posteriorly by the spinal accessory nerve. The jugulodigastric node (i.e., the principal node of Kuttner), the retromandibular vein, hidden in the tail of the parotid gland, is commonly encountered and ligated.
- IIb (“submuscular recess”): The posterosuperior extension of level IIa and IIb is delineated anteriorly by a vertical line at the level of the spinal accessory nerve and posteriorly by the posterolateral edge of the SCM. The superoinferior boundaries are identical to those of level IIa.
- Level III (midjugular): Level III is bounded superiorly by the inferior aspect of level II, anteriorly by the sternohyoid muscle, and posterolaterally by the posterolateral edge of the SCM. The inferior edge is demarcated by the omohyoid muscle surgically and cricoid cartilage radiographically. The jugulo-omohyoid node is contained in level III.
- Level IV (lower jugular): Extends from the inferior border of level III superiorly to the clavicle inferiorly, and from the lateral border of the sternohyoid muscle anteriorly to the posterolateral edge of the SCM. Level IV contains the transverse cervical artery and, in the left neck, the thoracic duct. A smaller accessory thoracic duct may be encountered in the right neck.
- Level V (posterior triangle): Extends from the posterior edge of the SCM to the anterior edge of the trapezius muscle, and inferiorly to the clavicle. Level V contains the spinal accessory nerve as it penetrates the SCM, coursing posteroinferiorly to innervate the trapezius muscle on its deep surface.
- Level VI (central compartment): Bounded by the hyoid bone superiorly and the suprasternal notch inferiorly, and extending to the carotid sheaths bilaterally, level VI contains the pretracheal (Delphian), prelaryngeal, and paratracheal lymph nodes.
- Level VII (superior mediastinal): Extends from the suprasternal notch superiorly to the level of the innominate artery inferiorly, and bounded laterally by the carotid sheaths. Although often considered outside the boundaries of the neck, the definition of level VII nodes as an inferior extension of paratracheal lymph nodes into the superior mediastinum persists in contemporary literature and is included here in the interest of completeness.
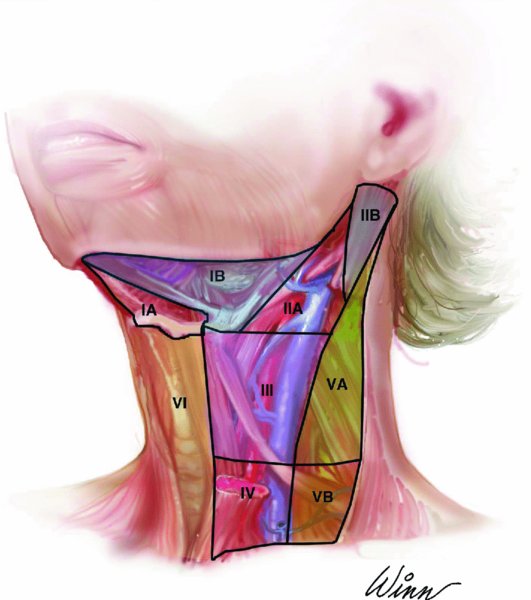
Figure 47.1. Schematic illustration depicting the levels of the neck.
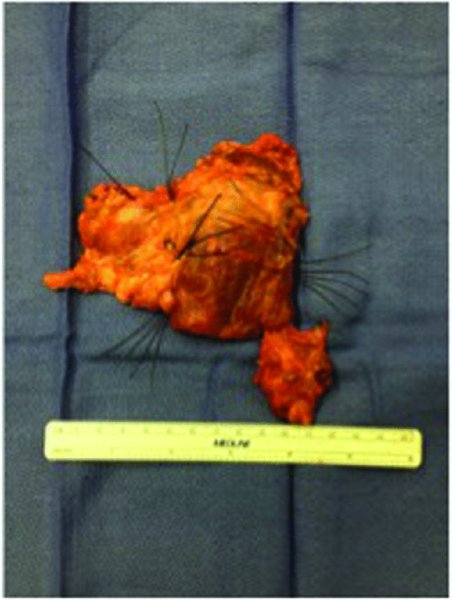
Figure 47.2. Sutures identifying the corresponding levels of the neck after lymphadenectomy.
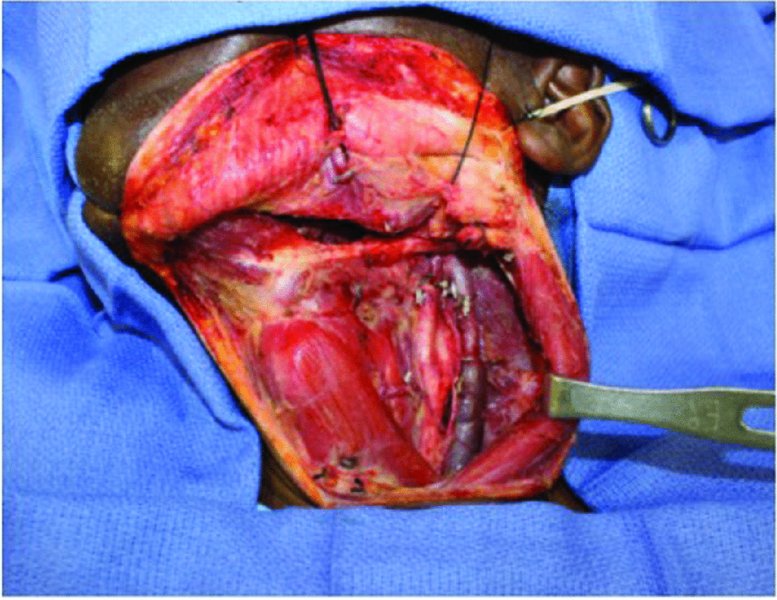
Figure 47.3. Selective neck dissection Levels I, II, and III.
Surgical Technique
Selective Neck Dissection, Levels I–III
- With the patient in the supine position, a vertically oriented shoulder roll is placed, allowing the scapulae to drop and spread laterally, exposing the anterolateral neck. Using monopolar electrocautery (or a scalpel blade), a curvilinear incision is made in a natural skin crease from the mastoid process to the midline at the level of the cricoid cartilage. If unilateral neck dissection is planned, the incision must be carried past the midline to allow sufficient exposure of level Ia with retraction of the platysmal flaps.
- The incision is carried through skin and subcutaneous tissues using electrocautery until the platysma muscle is exposed along the length of the incision. Skin hooks or Lahey clamps may be used to aid in skin retraction.
- The platysma is incised along its length, and subplatysmal flaps are raised superiorly to the inferior of the mandible and inferiorly to just above the clavicle. The platysma is deficient in the midline and posteriorly, and in these areas skin flap elevation is in the subcutaneous plane. Keeping the greater auricular nerve and external jugular vein down on the SCM at this step indicates that elevation is proceeding in the proper plane. Superior traction with skin hooks or finger grip and countertraction with a Kittner or sponge facilitate expeditious subplatysmal flap elevation in a relatively avascular plane (Figure 47.4).
- The neck dissection may proceed in an anterior-to-posterior direction, starting in level Ia with elevation of the fibrofatty node-bearing contents off of the anterior bellies of the digastric muscles bilaterally, the mandibular symphysis superiorly, and the mylohyoid muscle on the deep aspect. The submental artery will be encountered The specimen is brought inferiorly to the level of the hyoid bone, then slightly posterior as the strap muscles are encountered to elevate the fascia and nodal tissue from the surface of the sternohyoid muscle.
- The specimen is then freed sharply from the underlying musculature using monopolar electrocautery and carried posteriorly, crossing the digastric tendon, until the posterior edge of the mylohyoid muscle is encountered in level Ib. The inferior border of the mandible is cleaned superiorly, taking care to control vessels in this area with vascular clips or suture ligatures.
- Attention is then directed to the submandibular gland, which may be appreciated as a bulge just beneath the superficial layer of deep cervical fascia. The fascia is incised at the inferior aspect of the gland, approximately 2 cm below the inferior border of the mandible, and elevated (Figure 47.5). Care is taken to protect the marginal m/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


