45
Liver Function Tests, Hepatitis, and Cirrhosis: Assessment, Analysis, and Associated Dental Management Guidelines
LIVER FUNCTION TESTS
Liver function tests (LFTs) indicate how well the liver is functioning. LFTs should always be evaluated along with the patient’s history and physical examination. LFTs are not very sensitive, nor are they very specific.
Albumin, bilirubin, and PT/INR are true indicators of the biosynthetic capacity of the liver or overall liver function. ALT (SGPT), AST (SGOT), gamma-glutamyltransferase (GGT), and alkaline phosphatase are markers of disease, and they all indicate the status of hepatocellular damage.
LIVER STATUS ASSESSMENT COMPONENTS
The components that typically assess the liver status are the total protein, serum albumin, serum globulin, prothrombin time/international normalized ratio (PT/INR), alanine aminotransferase (ALT/SGPT), aspartate aminotransferase (AST/SGOT), total bilirubin, conjugated plus unconjugated bilirubin, alkaline phosphatase, and gamma-glutamyltransferase (GGT).
When LFTs are requested, most laboratories provide information on all components listed above with the exception of the PT/INR. When needed, the PT/INR always has to be requested separately. The PT/INR and the partial thromboplastin time (PTT) are provided together when coagulation studies are requested for surgical preoperative assessment. For discussion purposes, PT/INR will be included in the next section because it assesses liver biosynthetic function.
DETAILED DISCUSSION
Total Protein
The total protein constitutes the amount of albumin and globulin in the blood. The total protein value helps with the diagnosis of kidney disease, liver disease, liquid (blood) cancer, or malnutrition. The normal albumin to globulin ratio is 2:1; with cirrhosis, the ratio is reversed to 1:2. Normal total protein reference range is 6.5–8.2 g/dL.
Albumin
Albumin is a major protein and a true indicator of liver function. It is exclusively synthesized by the liver. The half-life of albumin is 20 days. Albumin, serum bilirubin, and prothrombin time are the three true indicators of liver function. Chronic liver disease causes a decrease in the amount of albumin produced. Therefore, in more advanced liver disease, the level of the serum albumin is reduced (less than 3.5mg/dL). Low albumin results in fluid leakage from the blood vessels into the tissues causing edema of the extremities. Albumin levels are always normal in acute liver disease and decreased in cirrhosis. Decreased levels, however, are not specific to liver disease, because protein-losing intestinal disease, colitis, acute or chronic infection, malnutrition, or chronic kidney disease can also cause a lowering of the albumin level. The normal albumin range is 3.5–5.0 g/dL.
Globulin
Globulins are made by the immune system and the liver cells. Globulins help fight infections. Globulin levels are increased in cirrhosis. Additionally, significant elevations of serum globulin in blood, associated with the presence of antinuclear antibodies or anti-smooth muscle antibodies, provide clues to the diagnosis of autoimmune hepatitis.
Low Albumin and Normal LFT Profile
Low albumin and normal LFTs are associated with proteinuria; acute inflammatory states caused by trauma, sepsis, and burns; and a chronic inflammatory state caused by active rheumatic disorders. Note that albumin values are lower in pregnancy.
Prothrombin Time/International Normalized Ratio
Prothrombin time or PT is a test that is used to assess blood clotting. Blood clotting factors are proteins made by the liver. When the liver is significantly injured, these proteins are not normally produced. The prothrombin time is also a useful test of liver function because there is a good correlation between abnormalities in coagulation measured by the prothrombin time and the degree of liver dysfunction. Thus, PT/INR, like albumin and serum bilirubin, is a true indicator of liver function.
- The liver produces Clotting Factors II, V, VII, IX, and X. An elevated PT/INR can result from a vitamin K deficiency in patients with chronic cholestasis (bile flow obstruction) or fat malabsorption from disease of the pancreas or small bowel and due to blood-thinning medications. Thus, a prolonged PT/INR is not specific to liver disease. The PT/INR does not become abnormal until more than 75–80% of liver synthetic capacity is lost. An abnormal PT/INR prolongation may be a sign of serious liver dysfunction. Bleeding will occur with INR >1.5.
- Factor VII has a short half-life of about six hours and it is sensitive to rapid changes in liver synthetic function. In fact, compared with other clotting factors, Factor VII has the shortest half-life. Thus, PT/INR is very useful for monitoring liver function in patients with acute liver failure. Normal PT/INR range is 0.9–1.2, average 1.
ALT and AST
Enzymes alanine aminotransferase (ALT)/SGPT and aspartate aminotransferase (AST)/SGOT are indicators of liver cell damage. The ALT and AST help the liver metabolize amino acids and thus make proteins. The ALT and AST show liver damage and are sensitive indicators of liver injury, especially acute liver injury. ALT is a more specific indicator of liver inflammation, as AST may be elevated in diseases of other organs. The ALT and AST are present in low levels in normal patients. ALT (SGPT) is predominately found in the liver and is present in the cytosol of the hepatocytes. The normal ALT range is 5–60 IU/L.
AST (SGOT) is found in the liver, cardiac muscle, skeletal muscle, kidney, brain, pancreas, lungs, RBCs, and WBCs, and in the cytosol and mitochondria of the hepatocytes. The normal AST range is 5–43 IU/L.
Mild or moderate elevations of ALT or AST are nonspecific and may be caused by a wide range of liver diseases. Mild elevations of ALT or AST in asymptomatic patients can be evaluated by initially considering alcohol abuse, hepatitis B, or hepatitis C. In acute viral hepatitis, the ALT and AST may be elevated to the high 100s or over 1,000IU/L. In chronic hepatitis or cirrhosis, the elevation of these enzymes may be minimal (less than two to three times normal) or moderate (100–300IU/L).
ALT, AST Levels of Elevation, and Hepatocellular Necrosis Etiology
The following are ALT and AST elevation levels:
- Mild ALT and AST elevation (<250 IU/L): Mild elevations can be due to drugs, bile stones, viral infection, alcohol, or exercise.
- Moderate ALT and AST elevation (250–1,000 IU/L): Moderate elevations can be due to EBV or HSV infection or NSAIDS.
- Severe ALT and AST elevation (>1,000 IU/L): Severe elevations can be drug- or toxin-induced, or due to an acute viral infection, choledocolithiasis, or primary graft failure.
Bilirubin
Bilirubin is formed primarily from the breakdown of “heme.” It is taken up from blood processed through the liver, and then secreted into the bile by the liver. Normal individuals have only a small amount of bilirubin circulating in blood (less than 1.2mg/dL).
Conditions that cause increased formation of bilirubin, such as destruction of red blood cells or decreased removal from the blood stream, as with liver disease, may result in an increase in the level of serum bilirubin. Levels greater than 3mg/dL are usually noticeable as jaundice. The bilirubin may be elevated in many forms of liver or biliary tract disease, and thus it is also relatively nonspecific.
Thus, serum bilirubin is generally considered a true test of liver function, because it reflects the liver’s ability to take up, process, and secrete bilirubin into the bile. Total bilirubin indicates the status of bile transportation, and bilirubin is the product of hemoglobin breakdown. Conjugated and unconjugated bilirubin are measured when LFTs are ordered.
Unconjugated Hyperbilirubinemia Etiology
Gilbert’s syndrome is the most common cause of benign hyperbilirubinemia and it is associated with impaired uptake or impaired conjugation of bilirubin.
Conjugated Hyperbilirubinemia Etiology
Hepatocellular disease, intra- or extrahepatic bile duct obstruction, or sepsis are common causes of conjugated hyperbilirubinemia.
Alkaline Phosphatase
Alkaline phosphatase (AP) is found in the liver, bone, placenta, kidney, intestine, and WBCs. AP metabolizes phosphorus and thus is an energy source for the body. AP levels are higher in men than in women. The normal range of AP is 30–115 IU/L.
AP is a marker of chronic cholestasis disease due to bile duct obstruction caused by stricture/stones or infiltrative disease caused by sarcoidosis/TB/cancer. Nonpathologic elevations of AP may occur during the third trimester of pregnancy, during adolescence, or as a normal part of aging. With cholestasis, alkaline phosphatase is markedly elevated when compared with the aminotransferases or bilirubin levels. The total bilirubin will be increased with cholestasis disease.
< ?enlrg?>
Alkaline phosphatase (AP) and gamma-glutamyltranspeptidase (GGT) are elevated in a large number of disorders that affect the drainage of bile such as a gallstone or tumor blocking the common bile duct, or alcoholic liver disease or drug-induced hepatitis blocking the flow of bile in smaller bile channels within the liver. Alkaline phosphatase and GGT indicate obstruction to the biliary system, either within the liver or in the larger bile channels outside the liver. Thus, AP and GGT are often labeled “the cholestatic enzymes” because they spill from the liver into the bloodstream, with obstruction. The AP and gamma-glutamyltransferase (GGT) levels typically rise to several times the normal level after several days of bile duct obstruction or intrahepatic cholestasis. GGT helps differentiate if AP is coming from the liver or bone. With biliary obstruction, the GGT will be increased. With bone disease, the GGT is unaltered.
The highest AP levels, often greater than 1,000 U/L, or more than six times the normal value, are found in diffuse infiltrative diseases of the liver, such as infiltrating tumors and fungal infections. Both AP and GGT levels are elevated in about 90% of patients with cholestasis. An elevated AP value originating from the liver is usually accompanied by an elevated GGT value, an elevated 5′-nucleotidase value, and other LFT abnormalities. 5′-nucleotidase is a subset of alkaline phosphate.
Cholestasis Etiology
Etiological factors associated with cholestasis are:
Isolated Elevation of AP in an Asymptomatic Patient with Normal GGT
Consider bone growth or injury, or primary biliary cirrhosis. AP levels rise in late pregnancy.
Gamma-Glutamyltransferase (GGT)
GGT is found in the hepatocytes and the biliary epithelial cells and brings oxygen to tissues. GGT is a sensitive indicator of hepatobiliary disease. It is not elevated in bone disease. GGT is most useful for confirming the hepatic origin of elevated alkaline phosphatase. Therefore, GGT is utilized as a supplementary test to ensure that the elevation of alkaline phosphatase is coming from the liver or the biliary tract. Unlike AP, GGT is not elevated in diseases of bone, placenta, or intestine.
Isolated Elevation of GGT Level Assessment
Isolated elevation of GGT level is induced by alcohol and there is usually no actual liver disease. The elevation of GGT alone, with no other LFT abnormalities, often results from enzyme induction by alcohol or seizure medications in the absence of liver disease. The GGT level is often elevated in persons who take three or more alcoholic drinks per day. A mildly elevated GGT level is a typical finding in patients taking anticonvulsants and by itself does not necessarily indicate liver disease. The normal GGT level is 5–80 IU/L.
Other Specific Tests Diagnosing Causes of Liver Disease
- Elevations in serum iron, the percent of iron saturated in blood, or the iron storage protein ferritin may indicate the presence of hemochromatosis, a liver disease associated with excess iron storage.
- Wilson’s disease is associated with an accumulation of copper in the liver, a deficiency of serum ceruloplasmin, and excessive excretion of copper into the urine.
- Low levels of serum alpha-1-antitrypsin may indicate the presence of lung and/or liver disease in children or adults with alpha-1-antitrypsin deficiency.
- A positive anti-mitochondrial antibody indicates the underlying condition of primary biliary cirrhosis.
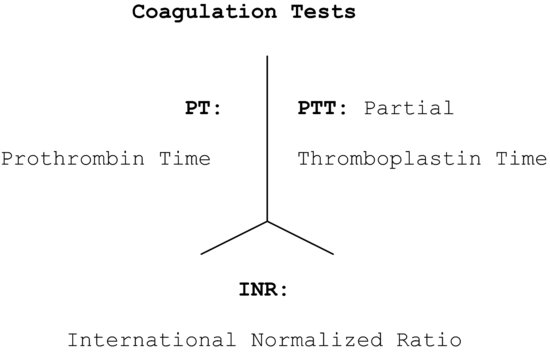
LFTs and Coagulation Studies: Medical Case Note/Medical Record Lattice Recording
LFTs, PT/INR, and PTT are often recorded in a standardized lattice pattern in medical records or medical case notes, and every practitioner should be able to read the tests when written as such. Figure 45.1 and 45.2 show the LFTs and coagulation studies lattice recordings.
Figure 45.1 Liver function tests lattice recording.
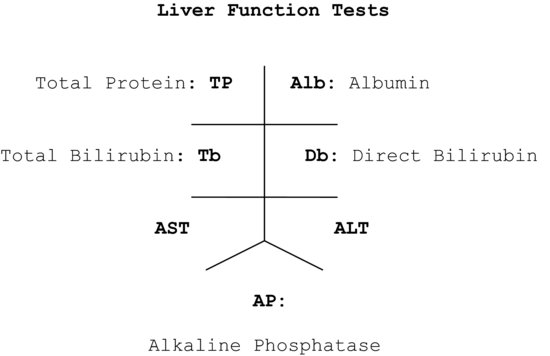
Figure 45.2 Coagulation tests lattice recording.
ACUTE VIRAL HEPATITIS: HEPATITIS A AND E
Acute and Chronic Viral Hepatitis Introduction
Viral hepatitis can present as an acute or chronic disease state, and viral infections of importance in the dental setting are hepatitis A, B, C, D, and E. Hepatitis A and E are grouped as the acute types of hepatitis. Hepatitis B, C, and D are grouped as the chronic types of hepatitis.
Hepatitis A and E: General Overview
Hepatitis A and E are caused by the hepatitis A virus (HAV) and the hepatitis E virus (HEV), respectively. Hepatitis A is universal in occurrence and is associated with endemic outbreaks. Hepatitis A affects all age groups, and jaundice commonly co-occurs.
Hepatitis E occurrence in the United States is very rare; it is, however, prevalent in South Asia and North Africa. Hepatitis E is more prevalent among pregnant women and is a serious concern during the third trimester.
The incubation period is two to six weeks for hepatitis A and two to nine weeks for hepatitis E. There is no chronic state, nor is there any sexual transmission with either type of hepatitis.
Transmission
Transmission of both types is by contaminated food and water. Person-to-person transmission is more common with hepatitis A than with hepatitis E.
Symptoms and Signs
Nausea, vomiting, abdominal pain, loss of appetite, fatigue, dark urine, and jaundice occur with both types of hepatitis.
Infection Markers
The occurrence of jaundice heralds the start of recovery, especially with hepatitis A. Jaundice usually occurs in 70% of the cases infected with the hepatitis A virus. Infection with hepatitis A or E is indicated by the presence of anti-HAV IgM or anti-HEV IgM in the blood, respectively. The patient is infected and infectious to others during this phase. Presence of anti-HAV IgG or anti-HEV IgG indicates immunity to hepatitis A and E, respectively. The antibodies provide lifelong immunity following recovery from hepatitis A; lifelong protection with the hepatitis E antibody is questionable.
Acute Viral Hepatitis LFT Profiles
ALT levels often rise to several thousand units per liter in patients with acute viral hepatitis. The highest ALT levels, often more than 10,000 IU/L, are usually found in patients with acute toxic injury subsequent to acetaminophen overdose. AST and ALT levels usually fall rapidly after an acute insult. In typical viral or toxic liver injury, the serum ALT levels rise more than the AST value, reflecting the relative amounts of these enzymes in hepatocytes.
Vaccinations
Hepatitis A infection can be prevented with the hepatitis A vaccine, which is given in two doses, 6–18 months apart. The vaccine is recommended for children in day-care settings, cafeteria workers, and those traveling to areas with a high risk of transmission.
Of the adults vaccinated, 94–100% develop antibodies one month after the first injection, and 100% of the vaccinated adults develop protective antibodies after the second dose. Hepatitis A vaccine gives lifelong immunity. Immune globulin (IG) is given after the first dose to travelers who plan to travel in less than one month after the first dose of the vaccine. There is no vaccine for Hepatitis E.
CHRONIC HEPATITIS: HEPATITIS B, C, AND D
Hepatitis B, C, and D: General Overview
Transmission
Hepatitis B, C, and D are chronic or gradual in onset; the transmission is via contaminated blood.
Symptoms and Signs
Nausea, vomiting, diarrhea, constipation, fever, skin rash, anorexia, weight loss, joint pains, dark-colored urine, yellowing of the skin or eyes, and aversion to smoking are the common complaints.
Hepatitis B: Detailed Discussion
The incubation period for hepatitis B is two to six months. The hepatitis B virus is transmitted by exposure to contaminated blood and from intravenous (IV) drug use. Mother-to-child transmission can occur and there is a high rate of sexual transmission with the virus.
Jaundice occurs in 30% of the patients. For most adults, it is a form of infection that ultimately resolves; for most children it is a form of infection that persists as a chronic state of infection. HBV attacks the liver and it can cause lifelong infection, cirrhosis, liver cancer, and even death. Of adult patients, 1–3% are affected with chronic hepatitis. Hepatitis B can predispose to liver cancer in the absence of cirrhosis.
Hepatitis B: Serological Markers
Hepatitis B virus is associated with three distinct antigen markers: HBsAg, HBeAg, and HBcAg. Each antigen has a definite timeline of appearance during the infection cycle and each triggers the appearance of a corresponding antibody in the blood indicating recovery or otherwise. Anti-HBs, anti-HBe, and anti-HBc are the antibodies triggered by the antigens HBsAg, HBeAg, and HBcAg, respectively.
The Hepatitis B Antigen–Antibody Cycle Graph
Figure 45.3< ?anchor c45-fig-0003?> depicts the sequential pattern of the rise and fall of the antigen–antibody markers associated with hepatitis B. Each of the markers is discussed in the following sections, and Figure 45.3 is used as a reference.
Figure 45.3 Classic hepatitis B antigen–antibody cycle.
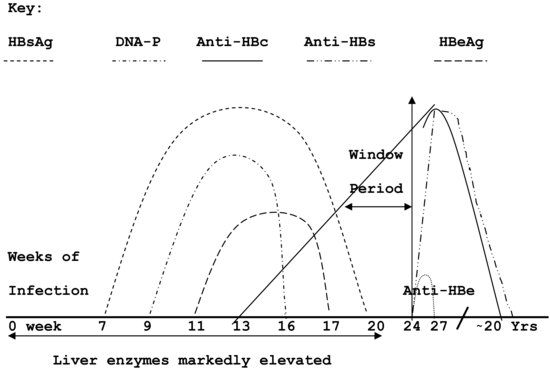
Serological Markers Facts
HBsAg (Surface Antigen)
The presence of HBsAg on hepatic serology indicates the presence of current infection. HBsAg is the first marker to appear in the blood, roughly around the seventh week from the start of an acute infection. In patients with a resolving infection, the HBsAg disappears completely from the blood by about the twentieth week from the start of infection.
A patient is said to be a simple “carrier” patient when the HBsAg does not disappear as expected and continues to be detected on serology, beyond the twenty-fourth week of infection. The carrier state occurs more commonly in children than adults.
Anti-HBs (Surface Antibody)
The presence of anti-HBs on hepatic serology indicates immunity. The presence of anti-HBs can be a result of hepatitis B immunization or it can appear in the blood after HBsAg from a natural infection that has completely cleared the system.
With a natural infection, anti-HBs appears around the twenty-fourth week from the start of the infection and persists for fifteen to twenty years, providing the patient with immunity during that time. It can be present, along with anti-HBc IgG, following recovery from a natural infection.
Anti-HBs is the only antibody formed with hepatitis B immunization. Anti-HBc IgM or anti-HBc IgG are not formed with vaccination.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


