41
Parathyroid Dysfunction Disease States: Assessment, Analysis, and Associated Dental Management Guidelines
PARATHYROID GLAND PHYSIOLOGY, FACTS, AND DYSFUNCTION OVERVIEW
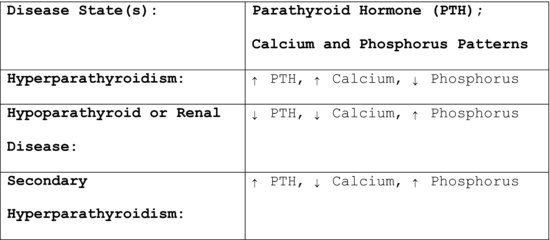
Parathyroid dysfunction is frequently associated with disturbances in the bone. Presence of some form of bone pathology may prompt a dentist to evaluate tests to measure serum calcium, phosphorus, and alkaline phosphatase levels. These tests are primarily used to diagnose hyperparathyroidism, Paget’s disease, metastatic bone disease, and disturbances in calcium absorption (Figure 41.1). Knowing the normal calcium metabolism and bone remodeling processes helps to better understand the changes in bone and blood tests that occur with associated disease states. The parathyroid glands, vitamin D, kidney, and gut are intricately involved in calcium metabolism and the remodeling of healthy bones.
Figure 41.1 PTH, calcium, and phosphorus changes and associated disease states.
Parathyroid Gland Physiology
There are two pairs of parathyroid glands embedded in the posterior surface of the thyroid gland, and there are several different populations of cells within the parathyroid glands.
The parathyroid glands are linked to the hypothalamus by negative homeostatic feedback mechanisms. Negative feedback mechanisms decrease the deviation from an ideal normal value and are important in maintaining homeostasis. The chief cells in the parathyroid glands secrete parathyroid hormone/parathormone/PTH, which activates vitamin D, affects bones and the kidney, and ultimately regulates the blood calcium level. If calcium ions decrease in the surrounding extracellular fluids, the parathyroid glands perceive the decrease and secrete more parathyroid hormone/PTH. The parathyroid hormone/PTH then stimulates calcium release from the bones by stimulating osteoclasts and inhibiting osteoblasts. PTH also increases intestinal absorption of calcium and reduces the urinary excretion of calcium ions through the kidneys. All of these mechanisms increase the calcium uptake into the bloodstream.
If blood calcium levels rise, the parathyroid glands reduce parathyroid hormone production. Thus, both responses are negative feedback responses and the effects are opposite of the stimulus.
Roles of the Gut, Parathyroid Glands, Vitamin D, and Kidney in Calcium Metabolism
- Calcium is an essential nutrient for mineralization of bone, increasing bone density, and decreasing the risk of fractures. Calcium increases bone density because it is a weak anti-resorptive agent that actually prevents bone breakdown and bone resorption, and also slightly modifies bone formation. Data show that patients given calcium have a greater decrease in alkaline phosphatase level, which confirms greater suppression of bone turnover, further showing that calcium works in terms of bone density.
- In terms of calcium supplementation and heart disease, high normal serum calcium is associated with increased carotid artery plaque thickness, an increased abdominal aortic calcification, an increased incidence of coronary heart disease and stroke, and an increased incidence of mortality. To prevent fractures, treatments with proven anti-resorptive agents are much better than calcium supplementation, but adequate calcium intake is important for normal bone health.
- Calcium balance is best determined by assessment of bone mass and a history of fracture rates.
- Elemental calcium is the calcium that is available for absorption, as with supplements containing calcium in addition to calcium from food sources. Most calcium is absorbed in the small intestine and the absorption in the gut occurs through active and passive mechanisms.
- Active mechanism: The active mechanism results in the trans-cellular movement of calcium, and this active transport is regulated primarily by 1,25(OH)2D, which is saturable. This regulated active transport of calcium is critically important when dietary calcium is very low. When there is no 1,25(OH)2D/calcitriol, active calcium absorption is essentially zero. As 1,25(OH)2D levels increase in the gut, active calcium absorption increases. Patients with normal 1,25(OH)2D levels can be in neutral calcium balance on very low calcium intakes because of the role of 1,25(OH)2D in increasing gut calcium absorption.
- Passive mechanism: The passive, para-cellular calcium movement in the gut is not regulated by vitamin D, nor is it dependent on 1,25(OH)2D. Adequate calcium absorption can occur with passive absorption of calcium that is not dependent on vitamin D to maintain balance.
- Dietary vitamin D and vitamin D absorbed from sunlight are converted in the liver to 25(OH)D (25-hydroxycholecalciferol /Calcidiol/25-hydroxyvitamin D). 25(OH)D is the specific vitamin D metabolite that is measured in the serum to determine a patient’s vitamin D status.
- PTH activates 1-alpha-hydroxylase in the kidney, which helps convert 25(OH)D to 1,25-dihydroxycholecalciferol (1,25-dihydroxyvitamin D3/calcitriol). This hormone then circulates in the blood, regulating the concentration of calcium and phosphate in the bloodstream and promoting the healthy growth and remodeling of bone. It is important to note that excess vitamin D is associated with an excess of calcium and this can increase the incidence of renal stones in the patient.
- Kidney disease is associated with a decrease in the production of active vitamin D3, causing hypocalcemia, secondary hyperparathyroidism, hyperphosphatemia, and renal osteodystrophy. Patients with renal osteodystrophy are prone to accelerated alveolar bone loss and it is not uncommon to discover Brown tumors in the jaws of such patients.
- Secondary hyperparathyroidism develops in chronic kidney disease because of hyperphosphatemia, hypocalcemia, decreased renal synthesis of 1,25-dihydroxycholecalciferol (1,25-dihydroxyvitamin D, or calcitriol), intrinsic alteration in the parathyroid gland, which gives rise to increased PTH secretion, as well as increased parathyroid growth and skeletal resistance to PTH.
- Calcium and calcitriol are primary feedback inhibitors for PTH; hyperphosphatemia is a stimulus to PTH synthesis and secretion. Phosphate retention begins in early chronic kidney disease. When the GFR falls, less phosphate is filtered and excreted, but serum levels do not initially rise because of increased PTH secretion, which increases renal excretion. As the GFR falls toward chronic kidney disease stages 4–5, hyperphosphatemia develops from the inability of the kidneys to excrete the excess dietary intake. Hyperphosphatemia suppresses the renal hydroxylation of inactive 25-hydroxyvitamin D to calcitriol, so serum calcitriol levels are low when the GFR is less than 30mL/min. Hypocalcemia develops primarily from decreased intestinal calcium absorption because of low plasma calcitriol levels. With the persistently elevated PTH levels, high-turnover bone disease or renal osteodystrophy occurs. Therefore, renal osteodystrophy is associated with hypocalcemia and high PTH levels.
- Therefore, bone disease and vascular calcification are common complications of chronic kidney disease (CKD). As previously discussed, CKD results in a fundamental disruption of the normal regulation of extracellular calcium, bone calcium, and vascular calcification. Abnormalities associated with serum phosphorus, PTH, vitamin D levels, and alkaline phosphatase occur as they relate to bone metabolism.
- According to the Institute of Medicine’s recommendations on calcium intake for women ages 19–50, and for men ages 19–70, the recommended daily allowance of calcium from dietary and supplement intake should be 1,000mg, and for both men and women older than 70, it should be 1,200mg. No increased intake is recommended for pregnant or lactating patients.
The parathyroid hormone regulates the excretion of phosphate by the kidneys, and hyperparathyroidism is associated with low phosphorous levels. Phosphorous levels are increased in patients with hypoparathyroidism and renal disease.
Alkaline phosphatase (ALP) is a hydrolase enzyme that is responsible for the release of phosphate from proteins and other molecules. This enzyme is found in the liver, bones, bile duct, lining of the intestine, kidney, and placenta. Alkaline phosphatase is a product of osteoblasts and is therefore related to bone growth. This accounts for higher-than-normal ALP levels among growing children compared to adults. Likewise, during the third trimester of pregnancy, the ALP level is on the higher side, as it is normal for the placenta to produce additional ALP. This enzyme is needed for the synthesis of proteins in the cells, and it has a vital part in the calcification of bones and cartilage.
Biliary stasis, pregnancy, growing bones, Paget’s disease, bone fractures, rheumatoid arthritis, osteoporosis, hyperparathyroidism, adrenal cortical hyperfunction, rickets, osteomalacia, osteosarcoma, metastatic bone disease, and renal and intestinal tumors can all cause increases in the alkaline phosphatase levels. Fatty liver, liver malignancy, hepatitis, cirrhosis, cholecystitis, cholangitis, and infection caused by Cytomegalovirus are other liver-related causes associated with elevated ALP. Phenytoin, ranitidine, erythromycin, carbamazepine, verapamil, and allopurinol are some of the drugs that can also elevate ALP levels.
Hyperparathyroidism
Hyperparathyroidism is associated with high calcium levels and high PTH. It usually manifests as a single adenoma but all four parathyroid glands may be affected. Autonomous production by the glands causes dysfunction of the negative feedback mechanism and consequent elevation of calcium and PTH levels. Oral findings encountered include bones of the jaw are less radio-dense, lamina dura may be absent, and radiolucent areas and central giant cell granulomas may occur.
Hypoparathyroidism
Hypoparathyroidism is associated with low calcium and low PTH levels. The condition is usually autoimmune. Hypoparathyroidism may be associated with oral candidiasis, hypoplasia of enamel, dentin, short roots, and delayed eruption of the teeth.
Osteomalacia
Osteomalacia is associated with vitamin D deficiency and it can be familial or acquired. Rickets and hypocalcification of dentin, enamel and alveolar bone are findings associated with vitamin D deficiency.
Vitamin D Excess
Excess vitamin D is associated with an excess of calcium. High vitamin D levels are associated with less bleeding on gingival probing.
Endogenous Causes
Endogenous causes of vitamin D excess include sarcoidosis, lymphoma, or TB. The immune cells make vitamin D in excess, which causes the calcium levels to be high.
Exogenous Causes of Vitamin D Excess
The exogenous cause is the presence of too much vitamin D in the milk.
Hypercalcemia from Tumors
Hypercalcemia can be caused by calcium-producing tumors from the lungs or breast.
BONE REMODELING PROCESS AND OSTEOPOROSIS
Bone Remodeling
Knowing the normal bone remodeling process and the associated blood tests demonstrating bone turnover rates helps to better understand the changes that occur with osteoporosis. The role of bone density tests and bone turnover markers in the diagnosis and management of osteoporosis is discussed at length in the following paragraphs.
Healthy bones are made up of living tissue—mainly collagen. Strong, healthy bones are maintained through a continuously balanced bone remodeling. Bone mass stays constant when bone resorption and bone formation are in balance. Bone turnover occurs exclusively on the surface of bone.
The bone remodeling process has two phases: breakdown/resorption and formation/deposition. Bone resorption, or bone breakdown, occurs first. Osteoclasts excavate small pits on the bone surface, releasing bone collagen and minerals in the circulatory system. Osteoclastic activity occurs over 7–10 days. The osteoclastic phase is then followed by bone formation/bone deposition, when osteoblasts deposit new tissue. Osteoblastic activity occurs over 2–3 months. The resting phase follows the bone remodeling phases, which are the combined osteoclastic and osteoblastic phases. The bone is mineralized in the resting phase, and the remodeling cycle begins again. The entire remodeling process takes 4–8 months (range: 3–24 months). Bone-remodeling phase cycle: resorption phase + formation phase + resting phase.
C-terminal telopeptide (CTx) and N-terminal telopeptide (NTx) markers: CTx and NTx are serum-based bone turnover biochemical markers of bone remodeling and particularly bone resorption. Together, these markers represent each end of the three strands of type 1 collagen, and each is used in tests that monitor bone turnover. Bone breakdown by-products appear in the urine and blood. CTx and NTx are dynamic measurements of the rate of bone breakdown. CTx and NTx tests measure these biochemical markers.
NTx test: NTx is a stable and specific breakdown product of bony collagen. NTx assay has been validated for the prediction of risk for osteoporosis and response to therapy. The serum NTx test is a very reproducible test demonstrating current osteoclastic activity. Increased serum NTx indicates increased bone turnover and increased risk for osteoporosis. Bisphosphonates decrease osteoclastic activity. Therefore, a decreased NTx value with bisphosphonate use indicates good response to bisphosphonate therapy. The NTx test is the more acceptable test compared with the CTx test.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


