Part 2: Selected Topics
4
The Treatment of Class II Malocclusion—Have We the Evidence to Make Decisions?
We will outline the evidence base for the treatment of children with Class II malocclusion by confining our sources to randomized trials and systematic reviews. We will base the chapter around common clinical dilemmas that are faced by all orthodontists on a daily basis.
These are as follows:
1. Should we provide treatment when the child is in the early transitional dentition as a phase I treatment with a functional appliance or headgear, followed by a phase II course of treatment when the child is an adolescent?
2. If a decision is made to wait until the child is in adolescence, should we provide treatment with a functional appliance or headgear to attempt to modify the growth or alternatively carry out treatment to correct the overjet using fixed appliances?
3. Should we carry out a treatment at all in adolescence compensating for skeletal discrepancies or perhaps wait until the child’s jaw growth is almost complete and then provide orthognathic surgical treatment?
Over the last 10 years, there have been several high level trials and systematic reviews that have provided us with a substantial amount of information on the evidence base for the treatment of Class II malocclusion. It is also important to point out that these studies have largely defined the patients according to their overjet. As a result, it may be more appropriate to consider that this discussion is primarily focused on the treatment of children with increased overjets. This then removes the need to discuss the perennial argument that Class II malocclusion cannot be readily categorized and treated by a “cookbook” approach that has its origins in clinical trials (Trenouth 2009; Hayes 2009).
Obtaining Research Evidence for Treating Increased Overjets in Class II Malocclusions
One of the most important publications in the treatment of increased overjets associated with Class II malocclusion was published over 20 years ago in 1990 (Tulloch et al. 1990). This paper did not change clinical practice overnight; however, it certainly inspired many orthodontic researchers to study treatment using randomized controlled trial (RCT) methodology and therefore is worth considering as an extremely valuable source of information. It was one of the first systematic reviews of the orthodontic literature, and the authors aimed to not only review the quality of the literature but also to answer the question on whether “methodological considerations—including sampling procedures, selection of comparison groups, choice of research design, consideration of confounding variables and statistical methods—might suggest that conclusions either supporting or refuting the growth modification effect of functional appliances should be regarded with caution.” The authors systematically reviewed the literature from 1980 to 1987 that had been published in the American Journal of Orthodontics, Angle Orthodontist, The British Journal of Orthodontics, and the European Journal of Orthodontics. They evaluated four main groups of variables that described the features of each study. These were (1) the type of appliance, (2) the research design, (3) the treatment setting and provider, and (4) the nature of the statistical analysis. They identified 50 studies, and it was clear that the most commonly used study design was retrospective (74%) compared with only 22% that were prospective. They also identified numerous problems with the treatment setting, data analysis, lack of sample size calculations, and selection bias.
It is worth quoting their final conclusion:
Given the problems of the multiple and limited indices of growth used by orthodontists—coupled with the weak research designs most frequently employed, the small sample sizes studied, and the ambiguous and incomplete reporting of important information—it is difficult to endorse conclusions supporting or refuting the growth-promoting influence of orthodontic appliances. Even the best of these studies suffer from methodologic limitations that make the interpretations of the results difficult. This review suggests that increased consideration of design, analysis and reporting would strengthen the value of clinical studies and permit more ready access to important information.
In short, the quality of evidence that underpinned the treatment of Class II malocclusion at that time was neither sufficient to confirm validity of, nor to lead to a change in, clinical practice. This realization, in many ways, inspired investigators to attempt to improve the quality of research in orthodontics and more specifically into the treatment of increased overjets or Class II malocclusion. There are, however, considerable ethical issues associated with this type of research.
Ethical Issues in Class II Research
It is essential when investigators are planning a randomized trial that they are in a “position of equipoise” as to the effects of the interventions that they are hoping to assess in their study. It is clear that investigators have addressed these issues well in studies that have evaluated the effect of early orthodontic treatment provided to children aged 8 to 10 years old. This is because there are no ethical dilemmas randomizing this age group of patients to either early treatment, when they are in the transitional dentition (i.e., two phase), or to delayed treatment that is provided as one phase in adolescence.
However, when we consider that perhaps the most important question in Class II research is How much growth modification occurs as a result of this functional or headgear treatment in adolescence? It is therefore difficult to ethically design a study that would involve randomizing half the patients to an untreated control group. Consequently, most studies have been confined to an evaluation of the effectiveness of early treatment compared to later treatment or comparisons between two types of appliances on groups of age-matched patients. Nevertheless, these studies have revealed a sufficient amount information that helps us answer the dilemma that we are faced with when we consider the treatment of a child with an increased overjet.
Early Orthodontic Treatment for Class II Malocclusion
Over the last 20 years, the provision of treatment when children are 8–10 years old with the aim of “intercepting” a developing Class II malocclusion has become popular. Treatment involves intervention when the child is in the early mixed dentition (phase I) followed by a second course of treatment when they are in early adolescence (phase II). The proponents of this type of treatment suggest that this early intervention normalizes the skeletal pattern, reduces the length of any subsequent phase II treatment, or at least makes further treatment simpler by reducing the need for extractions. These claims have been tested in several randomized trials that have evaluated the effectiveness of early orthodontic treatment (Courtney et al. 1996; Dolce et al. 2007; O’Brien et al. 2003a; O’Brien et al. 2003b; O’Brien et al. 2009; Tulloch et al. 2004; Wheeler et al. 2002). The findings have also been incorporated into a systematic review of Class II treatment (Harrison et al. 2007), and we shall now consider the findings of this review, which has been published by The Cochrane Collaboration. This review was carried out according to Cochrane guidelines and summarizes the current state of knowledge. The authors systematically searched the literature confining the search to randomized and controlled trials that evaluated treatment to correct prominent incisors in children who were under the age of 16 years old. They were specifically interested in the outcome measures of incisor overjet, skeletal relationship, self-esteem, and any possible harms as a result of treatment. They searched electronic databases and carried out a hand search, including trials that were not in the English language. They also carried out a quality assessment of each of the trials that were identified.
The electronic searches identified 185 studies, from which they obtained 105 full reports. After exclusions, they identified four trials concerned with early treatment for children aged 8–10 years old and four that evaluated the effects of treatment of children who were 10–15 years old. One problem that they identified was that there were multiple publications for three of the trials. They classified the trials according to their setting as follows: Florida, North Carolina, New Zealand, and UK.
All four studies were concerned with a comparison of active early treatment with an untreated control group. The Florida, North Carolina, and the UK study all followed the patients through to the conclusion of all orthodontic treatment; however, the New Zealand study only followed the patients to the conclusion of phase I. The Cochrane Review reported a meta-analysis that was carried out at the end of phase I and at the end of phase II.
The four studies all used slightly different treatment protocols for phase I treatment. The UK group used a Twin Block as the active intervention; the New Zealand group used a Frankel or a Harvold appliance; Florida evaluated two interventions, cervical pull headgear/biteplane combination and a bionator; and the North Carolina group evaluated cervical pull headgear and Bionator. All studies enrolled an untreated control group.
The results of these four high-quality studies are very similar and clinically important. When we consider the effect of early treatment compared to untreated controls, it appears that when a functional appliance was used, there was a modest difference in skeletal pattern (1.3 degrees), with a marked difference in incisor prominence (−4.0 mm). Similarly, the use of headgear resulted in small differences in ANB (−0.72 degrees) and overjet (−1.0 mm). The UK-based study also showed an increase in self-esteem for the treatment group. These trials were published at the end of the first phase of treatment, and although they were interesting, it could be suggested that the most important outcomes of this research were at the conclusion of all treatment when the child was an adolescent.
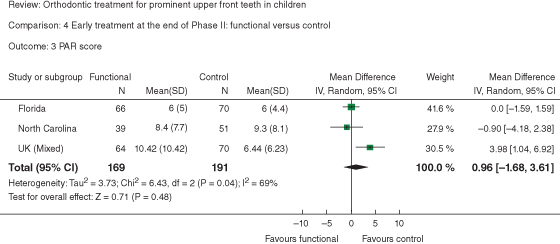
Three of the trials were extended to follow the patients through to the conclusion of orthodontic treatment, and the findings were included in the review (Harrison et al. 2007). A meta-analysis was carried out for final overjet, skeletal pattern, occlusal alignment (Peer Assessment Rating), incisal trauma, and self-esteem (O’Brien et al. 2009; Tulloch et al. 2004; Wheeler et al. 2002). The results of this analysis in the form of forest plots are shown for the effects of early treatment with a functional appliance versus one-phase treatment for final overjet, skeletal pattern (ANB), and occlusal alignment (PAR) in Figures 4.1–4.3. They concluded that
all the treatment was effective, in that incisor prominence had been reduced. Nevertheless, there were no differences in treatment outcome between the groups of children who had received one or two phases of treatment. As a result, it appears that two-phase treatment does not have any advantages over one phase treatment.
Figure 4.1 The effect of early treatment on overjet at the end of phase 2: functional appliance versus control
(Harrison et al. 2007). Reprinted with permission.
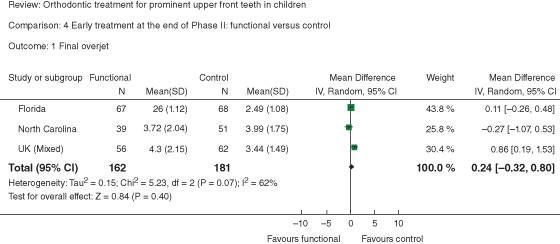
Figure 4.2 The effect of early treatment on final ANB at the end of phase II: functional versus control
(Harrison et al. 2007). Reprinted with permission.
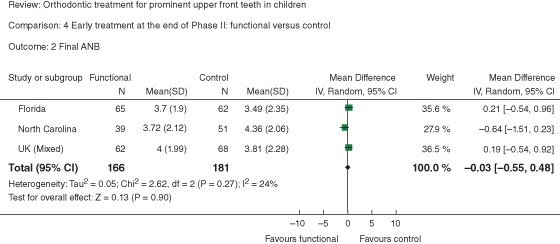
Figure 4.3 The effect of early treatment on PAR score at the end of phase II: functional versus control, outcome 3 PAR score
(Harrison et al. 2007). Reprinted with permission.
This is a compelling conclusion derived from a high level of scientific evidence and really suggests that early treatment does not confer any advantages of treatment that is provided in one phase during adolescence, apart from a transient increase in self-esteem.
Stability of Treatment
There has been very limited prospective research on the stability of treatment, and the only quality publication is one of the final reports of the early treatment trial carried out in Florida (Pavlow et al. 2008). This paper reported on the stability of the occlusions for 208 subjects who completed phase II treatment using the Peer Assessment Rating (PAR) as an outcome measure (Richmond et al. 1992). They collected records on 173 (83%) who had at least one follow-up visit, with a median follow up of 5 years. The analysis of this dataset was complex due to several different retention methods and the time periods of follow-up. They concluded that the final PAR index scores were influenced by the PAR score at the end of treatment, years in retention, and PAR score at the start of phase II treatment. This suggested that patients who have early phase I treatment might have more stable post-treatment occlusions; however, the magnitude of this differences was not likely to be clinically significant according to the authors. Interestingly, they did not find any other predictors of relapse.
These findings are clearly the highest level of evidence regarding the effectiveness of early treatment for increased overjets. While the conclusions have been readily accepted, it is not clear if any influential authorities have changed their clinical guidelines for early treatment.
In the UK, our approach has not fundamentally changed, in that there is not really a great deal of early treatment being undertaken unless it is specifically indicated. Unless a child is being teased at school about his or her prominent teeth or his or her parents are unduly concerned about the prominence, then t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


