4
Endodontic Examination and Diagnosis
As was mentioned above, as many as 90% of patients with oral or maxillofacial pain should be examined for endodontic diseases. A correct diagnosis is arrived at by combining information from the patient and sometimes the patient’s physician with the actual clinical findings. Although the diagnosis may often appear obvious and straightforward, the clinical examination should always be thorough and systematic. Only then can the dentist’s knowledge and clinical experience be fully utilized. A good chart system is invaluable in this regard.
History
Taking the history is an important part of the clinical examination, often giving information that immediately points to the patient’s illness. Since there are virtually no systemic contraindications to endodontic treatment, the medical history can normally be short and of a summary nature. However, it is necessary to form a picture of the general health of the patient, and not infrequently this information will contribute directly to the dental diagnosis. The following questions must be included in a medical history:
Do you have heart problems?
Are you allergic to anything?
Are you diabetic?
Have you been infected with hepatitis or HIV?
Are you taking any medication at the moment?
What is your physician’s name, address, and phone number?
Depending on the patient’s answers, the history will develop in as great a depth as is deemed necessary. Do not hesitate to call the patient’s physician for information, and with obviously sick patients it is advisable to treat them with the knowledge of and in cooperation with their physicians.
The dental history should identify the reason why the patient is seeking dental care (chief complaint). First the patient must be allowed to describe this reason in his or her own words. Afterward the dentist asks necessary leading questions to expand on the information given by the patient. During the interview the patient usually remembers additional information and a rather complete picture of the patient’s problem will develop.
Clinical Examination
The clinical examination begins with an extraoral inspection while taking the patient’s history. The examination is then extended to the area the patient has referred to in the history and to adjacent and contralateral areas. One quick glance may be enough to arrive at the diagnosis and to decide on appropriate therapy. For example, a tooth may be so damaged by caries that a remaining root rest will have to be extracted. Other times visual findings like caries, discolorations, swellings, fistulae, etc. may lead to other considerations. The clinical examination then continues with the aid of a mirror, explorer, periodontal probe, and other instruments and devices as found to be practical or necessary for a general oral/dental examination.
Percussion and Palpation Tests
The percussion test is a simple but extremely useful examination method which is used to ascertain an inflammatory condition in the apical periodontium of a tooth. The handle of a hand instrument, usually a mirror, is used to tap on the teeth in a vertical direction. A tooth with symptomatic apical periodontitis will then be more sensitive to the percussion than the contralateral or neighboring teeth. Only remember, healthy teeth may be somewhat sensitive to percussion as well and if the symptoms from an apical periodontitis are weak or uncertain, it is important to test several teeth repeatedly in no special order to ensure consistency in the observations. Pulpal diseases cannot be revealed by means of the percussion test until the apical periodontium is involved. On the other hand, a pe riodontal abscess or even asymptomatic periodontal disease with severe loss of marginal bone may render teeth tender to percussion. However, such teeth will react mostly to horizontal percussion, i. e., percussion perpendicular to the long axis of the tooth and less to vertical percussion like endodontically involved teeth. The percussion test is the examination method that will first give clinical indications of an apical periodontitis.
Palpation is performed to ascertain tenderness, swelling, fluctuation, hardness, and crepitation in underlying tissues. Here again it is important to make comparative examinations of neighboring and contralateral areas. Intraorally the palpation test preferably is carried out with the tip of an index finger. Sometimes and in special areas like the floor of the mouth it may be practical to use the index finger on both hands. During extraoral palpation of lymph nodes, swellings, sinus, and tempero-mandibular joint areas, etc., two to three fingers on one or both hands are used. The palpation test may be very useful during an endodontic examination and its usefulness will only increase with increasing skill and clinical experience.
Sensitivity Tests
Sensitivity tests are performed in an effort to determine whether the pulp of a tooth is vital or not. This test is often of crucial importance. The sensitivity of a tooth can be tested in many ways. Normally heat, cold, or electrical stimulation are used. With all test methods it is imperative that the tooth to be tested be clean and completely dry so that the possibilities for conduction of the stimulus to nerves of the gingiva and the periodontal ligament are minimized. For a heat test, temporary stopping (gutta-percha) may be used. It is heated over an alcohol flame and with a plastic instrument applied with slight pressure to assure good contact to the incisal edge or to the buccal surface of the tooth away from the gingiva. It is immediately removed if the patient shows a reaction, otherwise it is left in place until it cools off.
A cold test can be performed with ice, but more effective are frozen sticks of carbon dioxide (–78 °C). Effective tests can also be carried out with a cotton pellet sprayed with difluorodichloromethane (DDM) (–50 °C), which is immediately placed in good contact with the incisal edge or buccal surface of the tooth. The cotton pellet is removed if there is a reaction, or it is left in place until it has lost its effect.
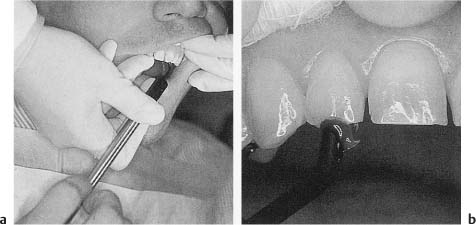
For electric sensitivity testing a special apparatus, an electric pulp tester, is required. The electric pulp tester is equipped with an electrode that is placed in contact with the tooth to be tested as described for the thermal tests (Fig. 4.1). An electric current can then be supplied to the tooth through the electrode, and the current (or the voltage) is increased manually or automatically until the patient shows a reaction. The electrode is then immediately removed. Otherwise the test continues until maximum stimulus has been reached.
Fig. 4.1
a Electric pulp tester in use. Since the dentist wears rubber gloves, the patient needs to touch the hand-piece of the testing device to complete the electric circuit.
b Test electrode in contact with the incisal edge of a tooth. Toothpaste is used to ensure good contact.
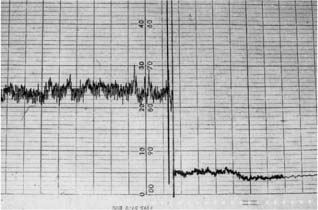
Fig. 4.2 Vitality testing of contralateral teeth with a laser Doppler flowmeter. Curve to the left, vital pulp with blood circulation. Curve to the right, non-vital pulp without blood circulation.
The sensitivity tests are not always reliable and the results of these tests obviously have to be evaluated together with other findings and symptoms. The electric test is considered by many to be the least reliable method. However, this method has many advantages and an electric pulp tester should be part of the armamentarium of every dental office. The main advantage of the electric test is that a spe/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses