4 Anesthesia Considerations for Cosmetic Facial Surgery
Local Anesthesia for Cosmetic Facial Surgery
No one can argue that one of greatest medical advances in the history of mankind was the discovery of local anesthetic agents. Virtually no other single innovation has done so much so safely to mitigate human suffering. Local anesthetics are agents that reversibly block nerve conduction in a limited area when injected or topically applied1 and exhibit their effect by blocking noxious stimuli from reaching the brain.2
Mechanism of Action of Local Anesthetics
Local anesthetics block the sensation of pain by interfering with the propagation of impulses along peripheral nerve fibers without significantly altering normal resting membrane potentials.3 Local anesthetics depolarize nerve membranes and prevent achievement of a threshold potential. A propagated action potential fails to develop, and conduction blockade is achieved. This occurs through the interference of nerve transmission by blocking the influx of sodium through the excitable nerve membrane.4
Sensory Anatomy of the Head and Neck
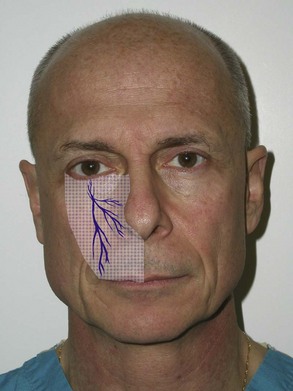
The main sensory innervation of the face is derived from cranial nerve V (trigeminal nerve) and the upper cervical nerves (Figure 4-1).
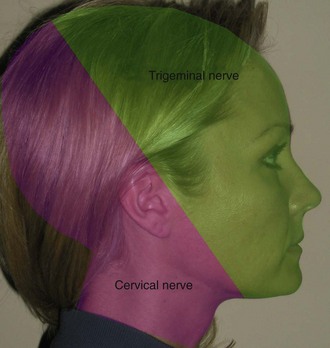
FIGURE 4-1 Sensory innervation of the head and neck is derived from the trigeminal and upper cervical nerves.
Trigeminal Nerve
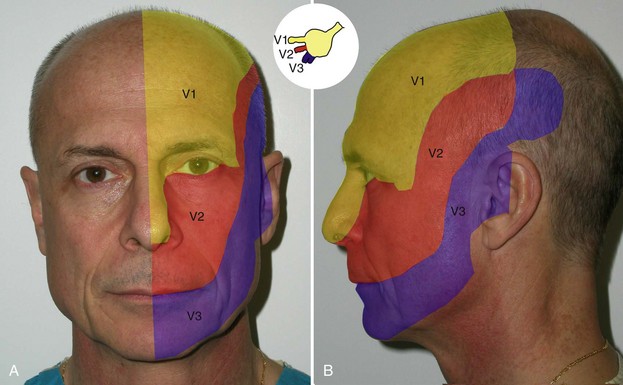
The trigeminal nerve is the fifth of the 12 cranial nerves. Its branches originate at the semilunar ganglion (gasserian ganglion) located in a cavity (Meckel’s cave) near the apex of the petrous part of the temporal bone. Three large nerves, the ophthalmic, maxillary, and mandibular, proceed from the ganglion to supply sensory innervation to the face (Figure 4-2).
Often referred to as the great sensory nerve of the head and neck, the trigeminal nerve is named for its three major sensory branches. The ophthalmic nerve (V1), maxillary nerve (V2), and mandibular nerve (V3) are literally “three twins” (trigeminal) carrying sensory information of light touch, temperature, pain, and proprioception from the face and scalp to the brainstem. The commonly used terms V1, V2, and V3 are shorthand notation for cranial nerve V, branches one, two, and three, respectively. In addition to nerves carrying incoming sensory information, certain branches of the trigeminal nerve also contain nerve motor components. (The ophthalmic and maxillary nerves consist exclusively of sensory fibers; the mandibular nerve is joined outside the cranium by the motor root.) These outgoing motor components include branchial motor nerves (nerves innervating muscles derived embryologically from the branchial arches) as well as “hitchhiking” visceral motor nerves (nerves innervating viscera, including smooth muscle and glands). The trigeminal nerve exits the trigeminal ganglion and courses backward to enter the mid-lateral aspect of the pons at the brainstem.5
The ophthalmic nerve (V1) leaves the semilunar ganglion through the superior orbital fissure, the maxillary nerve (V2) leaves the semilunar ganglion through the foramen rotundum at the skull base, and the mandibular nerve (V3) leaves the semilunar ganglion through the foramen ovale at the skull base5 (see Figure 4-2, inset). The remainder of this chapter will only discuss the sensory components of this nerve system as they relate to local anesthetic blocking techniques for cosmetic facial procedures.
Ophthalmic Nerve (V1)
The ophthalmic nerve, or first division of the trigeminal, is a sensory nerve. It supplies branches to the cornea, ciliary body, and iris; to the lacrimal gland and conjunctiva; to part of the mucous membrane of the nasal cavity; and to the skin of the eyelids, eyebrows, forehead, and upper lateral nose (see Figure 4-2, V1). It is the smallest of the three divisions of the trigeminal and divides into three branches: the frontal, nasociliary, and lacrimal.5 The frontal nerve divides into the supraorbital and supratrochlear nerves, providing sensation to the forehead and anterior scalp.
Maxillary Nerve (V2)
The maxillary nerve, or second division of the trigeminal, is a sensory nerve that crosses the pterygopalatine fossa, traverses the orbit in the infraorbital groove and canal in the floor of the orbit, and appears upon the face at the infraorbital foramen as the infraorbital nerve.5 At its termination, the nerve divides into branches which spread out upon the side of the nose, the lower eyelid, and the upper lip, joining with filaments of the facial nerve.5 Terminal branches include the following:
Mandibular Nerve (V3)
The mandibular nerve supplies the teeth and gums of the mandible, the skin of the temporal region, part of the auricle, the lower lip, and the lower part of the face (see Figure 4-2, V3). The mandibular nerve also supplies the muscles of mastication and the mucous membrane of the anterior two-thirds of the tongue. It is the largest of the three divisions of the fifth cranial nerve and is made up of a motor and sensory root.5
Sensory branches of the mandibular nerve include the auriculotemporal nerve, which supplies sensation to the skin covering the front of the helix and tragus (see Figure 4-2), and the inferior alveolar nerve, the largest branch of the mandibular nerve. It descends with the inferior alveolar artery and exits the ramus of the mandible to the mandibular foramen. It then passes forward in the mandibular canal, beneath the teeth, as far as the mental foramen, where it divides into two terminal branches, incisive and mental nerves. The mental nerve emerges at the mental foramen and divides into three branches; one descends to the skin of the chin, and two ascend to the skin and mucous membrane of the lower lip.5 The buccal nerve supplies sensation to the skin over the buccinator muscle.
Local Anesthetic Techniques
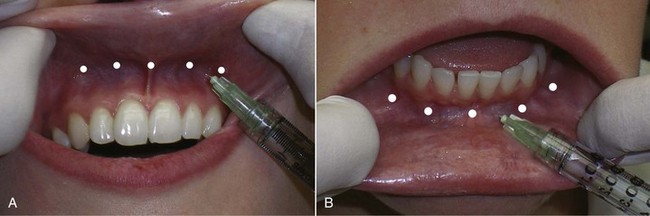
Technique for Upper and Lower Lip Anesthesia
As soon as the patient is seated in the treatment room, a potent topical anesthesia compound of 20% benzocaine, 6% lidocaine, and 4% tetracaine is applied intraorally in the depth of the anterior maxillary and mandibular vestibule. The vestibule is the sulcus formed at the junction of the attached gingiva and the unattached mucosa. The same topical is applied to the external lip mucosa. A 1-mL syringe of 2% lidocaine, 1 : 100,000 epinephrine, and a 32-gauge needle are used. Injections of 0.2 to 0.3 mL of local anesthetic solution are given in four to five areas between the canine teeth (Figure 4-3, A). The injection is submucosal in the potential space between the mucosa and the periosteum. This is a soft-tissue injection, so the needle need not touch bone. If both lips are to be injected, the same procedure is performed in the lower vestibule as well (see Figure 4-3, B). After several minutes, the lips and perioral areas are adequately anesthetized for filler injection. This infiltration, if done properly, will approach the profound level and extent of anesthesia experienced with bilateral nerve block and is well suited for cutaneous and vermilion filler injection of the lips. The area anesthetized may extend to the nasal tip in the maxilla and to the mentolabial fold in the mandible. Return of sensation generally progresses between 30 and 60 minutes. No significant anatomic structures traverse this area of the vestibule, and the author has experienced no complications with thousands of these injections.
Technique for Nasolabial Fold Anesthesia
Using the 1-mL syringe with a 32-gauge needle, 0.1 to 0.2 mL of local anesthesia is injected deep in the nasolabial fold (so as not to distort the fold and effect filler accuracy) in two to three areas from the nostril to the corner of the mouth (Figure 4-4). Only a small amount of local anesthesia is required to produce acceptable anesthesia. Although many practitioners use no anesthesia for cutaneous injection, I can attest to patient appreciation of this simple technique.
Local Anesthetic Techniques for Blocking the Main Sensory Nerves of the Head and Neck
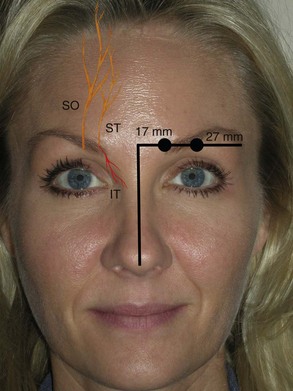
Scalp and Forehead
The frontal nerve exits through a notch (in some cases a foramen) on the superior orbital rim approximately 27 mm lateral to the glabellar midline (Figure 4-5). This supraorbital notch is readily palpable in most patients. After exiting the notch or foramen, the nerve traverses the corrugator supercilii muscles and branches into a medial and lateral portion. The lateral branches supply the lateral forehead, and the medial branches supply the scalp. The supratrochlear nerve exits a foramen approximately 17 mm from the glabellar midline (see Figure 4-5) and supplies sensation to the middle portion of the forehead. The infratrochlear nerve exits a foramen below the trochlea and provides sensation to the medial upper eyelid, canthus, medial nasal skin, conjunctiva, and lacrimal apparatus6 (see Figure 4-5).
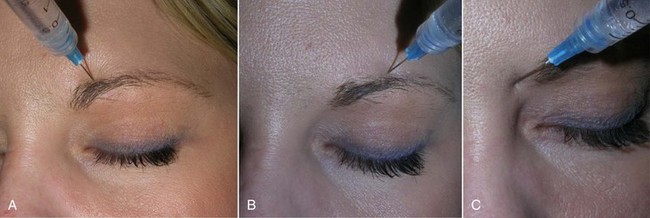
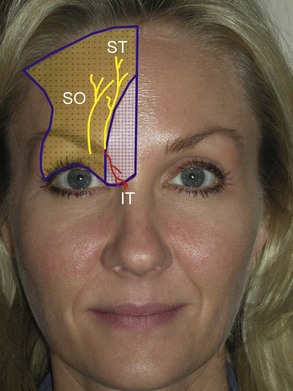
When injecting this area, it is prudent to always use the free hand to palpate the orbital rim to prevent inadvertent injection into the globe! To anesthetize this area, the supratrochlear nerve is measured 17 mm from the glabellar midline, and an injection of 1 to 2 mL of 2% lidocaine, 1 : 100,000 epinephrine is given (Figure 4-6, A). The supraorbital nerve is blocked by palpating the notch (and or measuring 27 mm from the glabellar midline) and injecting 2 mL of local anesthetic solution (see Figure 4-6, B). The infratrochlear nerve is blocked by injecting 1 to 2 mL of local anesthetic solution at the junction of the orbit and the nasal bones (see Figure 4-6, C). In reality, one can block all three of these nerves by simply injecting 2 to 4 mL of local anesthetic solution from the central brow proceeding to the medial brow. Figure 4-7 shows the regions anesthetized by the described blocks.
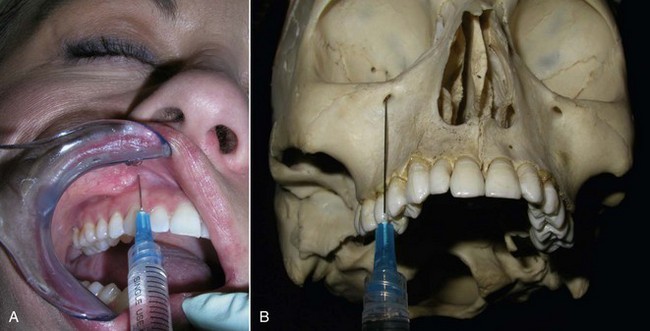
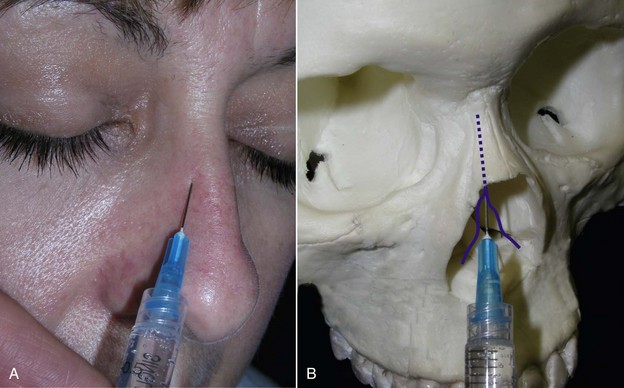
Infraorbital Nerve Block
The infraorbital nerve exits the infraorbital foramen 4 to 8 mm below the orbital rim in an imaginary line dropped from the medial limbus of the iris6 or the pupillary midline. The anterior superior alveolar nerve branches from the infraorbital nerve before it exits the foramen, so some patients will manifest anesthesia of the anterior teeth and gingiva if the branching is close to the foramen. Areas anesthetized include the lateral nose, anterior cheek, lower eyelid, and upper lip on the injected side. This nerve can be blocked by intraoral or extraoral routes. To perform an infraorbital nerve block from an intraoral approach, topical anesthesia is placed on the oral mucosa at the vestibular sulcus just under the canine fossa (between the canine and first premolar tooth) and left for several minutes. The lip is then elevated, and a  -inch 27- gauge needle is inserted in the sulcus and directed superiorly toward the infraorbital foramen (Figure 4-8). It is unnecessary for the needle to enter the foramen for a successful block. The anesthetic solution need only contact the vast branching around the foramen to be effective. It is imperative to use the other hand to palpate the inferior orbital rim to avoid injecting the orbit; 2 to 4 mL of 2% lidocaine with 1 : 100,000 epinephrine are injected in this area for the infraorbital block.
-inch 27- gauge needle is inserted in the sulcus and directed superiorly toward the infraorbital foramen (Figure 4-8). It is unnecessary for the needle to enter the foramen for a successful block. The anesthetic solution need only contact the vast branching around the foramen to be effective. It is imperative to use the other hand to palpate the inferior orbital rim to avoid injecting the orbit; 2 to 4 mL of 2% lidocaine with 1 : 100,000 epinephrine are injected in this area for the infraorbital block.
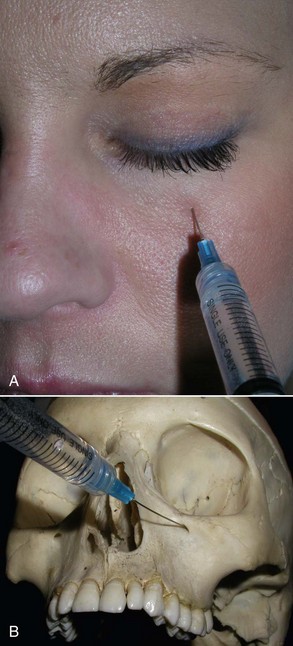
The infraorbital nerve can also be very easily blocked by a facial approach, and this is the author’s preferred route. It may also be the preferred route in dental-phobic patients. A 32 gauge  -inch needle is placed through the skin and aimed at the foramen in a perpendicular direction. An injection of 2 to 4 mL of local anesthetic solution is given at or close to the foramen (Figure 4-9). Again, the other hand must constantly palpate the inferior orbital rim to prevent inadvertent injection into the orbit. A successful infraorbital nerve block will anesthetize the infraorbital cheek, the lower palpebral area, the lateral nasal area, and superior labial regions, as shown in Figure 4-10.
-inch needle is placed through the skin and aimed at the foramen in a perpendicular direction. An injection of 2 to 4 mL of local anesthetic solution is given at or close to the foramen (Figure 4-9). Again, the other hand must constantly palpate the inferior orbital rim to prevent inadvertent injection into the orbit. A successful infraorbital nerve block will anesthetize the infraorbital cheek, the lower palpebral area, the lateral nasal area, and superior labial regions, as shown in Figure 4-10.
The aforementioned techniques provide anesthesia to the lateral nasal skin but do not provide anesthesia to the central portion of the nose. A dorsal (external) nasal nerve block will supplement nasal anesthesia by providing anesthesia over the area of the cartilaginous nasal dorsum and tip. This supplementary nasal block is accomplished by palpating the inferior rim of the nasal bones at the osseous cartilaginous junction. The dorsal nerve (anterior ethmoid branch of the nasociliary nerve) emerges 5 to 10 mm from the nasal midline at the osseous junction of the inferior portion of the nasal bones (the distal edge of the nasal bones) (Figure 4-11). The dotted line in Figure 4-11 shows the course of this nerve under the nasal bones before emerging.
Two often overlooked nerves in facial local anesthetic blocks are the zygomaticotemporal and zygomaticofacial nerves. These nerves represent terminal branches of the zygomatic nerve. The zygomaticotemporal nerve emerges through a foramen on the anterior wall of the temporal fossa. This foramen is actually behind the lateral orbital rim posterior to the zygoma at the approximate level of the lateral canthus (Figure 4-12).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



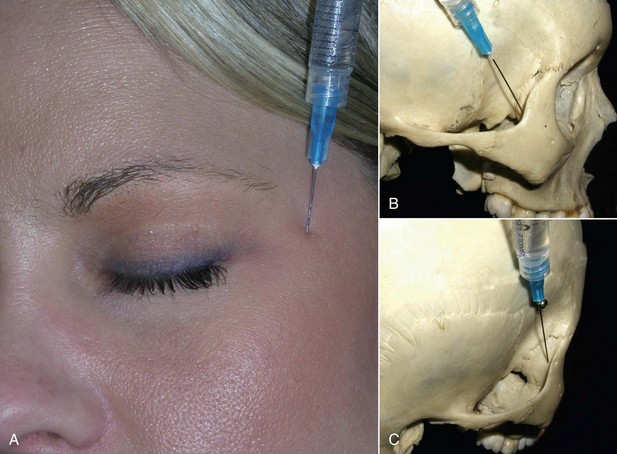
 -inch needle behind the concave portion of the lateral orbital rim. It is suggested that one closely examine this area on a model skull prior to attempting this injection; it will make the technique simpler. To orient for this injection, the doctor needs to palpate the lateral orbital rim at the level of the frontozygomatic suture (which is frequently palpable). With the index finger in the depression of the/>
-inch needle behind the concave portion of the lateral orbital rim. It is suggested that one closely examine this area on a model skull prior to attempting this injection; it will make the technique simpler. To orient for this injection, the doctor needs to palpate the lateral orbital rim at the level of the frontozygomatic suture (which is frequently palpable). With the index finger in the depression of the/>