Chapter 4
Access Flaps for Surgical Root Surface Debridement
Aim
The aim of the chapter is to review the indications and contraindications for surgical root surface debridement and to discuss the procedure in detail.
Outcome
Having read this chapter, the reader should be able to decide which clinical situations may necessitate surgical access for RSD and have a clear understanding of the procedures involved.
Introduction
Periodontitis is an inflammatory lesion, mediated by host-parasite interactions, that results in loss of connective tissue attachment to the root surface and destruction of adjacent alveolar bone. The disease process initially involves apical migration of the junctional epithelial attachment along the root surface, prior to thickening of the epithelial lining to form an occlusive pocket-lining epithelium.
Suprabony pocketing arises where the apical extent of the pocket is coronal to the alveolar crest; this occurs as a result of horizontal bone loss (Fig 4-1). Infrabony pocketing is where the apical extent of the pocket lies apical to the alveolar crest; this arises normally as a result of vertical bone loss (Fig 4-2).
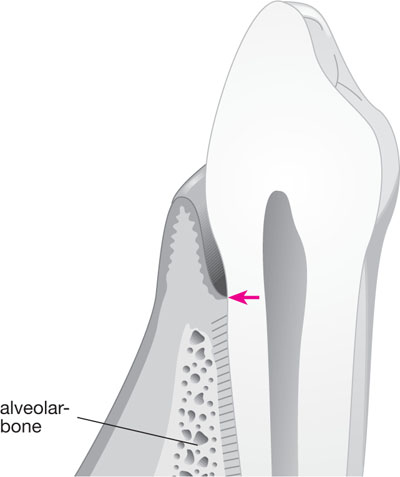
Fig 4-1 Suprabony pocketing.
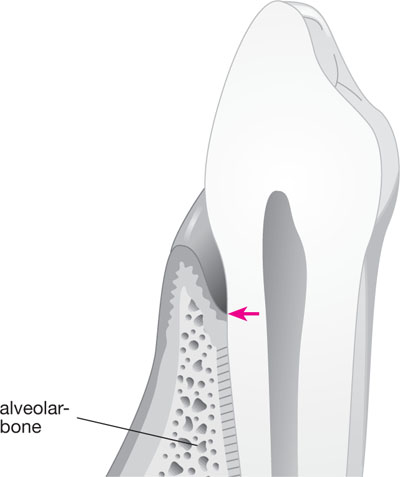
Fig 4-2 Infrabony pocketing.
The choice of treatment for patients with periodontitis varies according to the extent and pattern of attachment loss, local anatomical variations, type of periodontal disease and treatment objectives.
Presurgical Management
All patients should have a comprehensive examination to include radiographic analysis, detailed pocket charting, assessment of furcation status, bleeding on probing, mobility status and presence of suppuration. This information should be recorded at the initial visit and is important for diagnosis, treatment planning and determining prognosis. The same details should be recorded during and after presurgical therapy and surgical treatment as they give an indication of treatment success and may draw attention to specific problems or areas requiring further therapy.
All but the most aggressive forms of periodontitis require an initial phase of non-surgical therapy. This usually includes:
-
Patient education in their disease and associated risk factors.
-
Rigorous oral hygiene.
-
Smoking cessation advice.
-
Control of contributing systemic risk factors, e.g. diabetes mellitus.
-
Supra- and subgingival scaling and RSD. The objective of scaling and RSD is the complete removal of bacteria, biofilm, endotoxin and calculus to achieve a biologically acceptable root surface.
-
Local factors contributing to chronic periodontitis should be removed or controlled. Consideration should be given to carrying out the following:
-
removal of overhanging restoration margins
-
reshaping or replacing over-contoured crowns
-
replacement of poorly designed and fitting removable prostheses
-
restoration of carious lesions
-
orthodontic treatment
-
treatment of occlusal trauma.
-
Teeth with a poor prognosis, requiring extraction, need to be identified. Extractions of compromised teeth should be carried out expediently to aid the overall treatment plan.
Aggressive Periodontitis
Patients with aggressive forms of periodontitis will usually require referral to specialist services for non-surgical therapy with adjunctive antibiotics. Adjunctive antibiotic therapy is of proven value in the treatment of aggressive periodontitis, which often involves several specific pathogens that have the potential to invade pocket epithelium and connective tissue, and to colonise non-gingival reservoir sites. Where disease is refractory to this approach, surgical intervention may be considered.
Outcomes following scaling and RSD include:
-
reduction of clinical inflammation
-
microbial shift to a less pathogenic sub-gingival flora
-
decreased probing depth
-
gain of clinical attachment
-
slower disease progression
-
gingival recession
-
tightening of the gingival cuff and pocket reduction.
Surgical Management
If the results of initial therapy do not control the periodontitis, surgery may be considered. Several factors may limit the effectiveness of non-surgical RSD:
-
complex root anatomy
-
furcations
-
deeper pockets
-
patient-specific factors (see Chapter 1).
Surgical access is often necessary to facilitate mechanical instrumentation of the roots. This approach provides direct access to the root surface. Surgical RSD largely involves procedures to improve access for instrumentation and surgical elimination of the pocket to enable the patient to clean to the depth of the sulcus.
Objectives of Surgical Root Surface Debridement
-
Improved visibility of the root surface.
-
Accessibility for exploration of the root surface and instrumentation.
-
Removal of plaque, calculus and other plaque retentive features.
-
Elimination of periodontal pockets > 4 mm.
-
Creation of a dentogingival morphology to facilitate oral hygiene procedures.
-
Allowing placement of regenerative materials (Chapter 5).
A drawback to surgical RSD is the potential for gingival recession. This may lead to dentine hypersensitivity and leave the root surface vulnerable to caries, and may also have implications for aesthetics around anterior teeth. The risk of gingival recession should be discussed thoroughly with the patient prior to any treatment as part of the informed consent process. Indications and contraindications to surgical RSD are listed in Table 4-1.
| Indications | Contraindications |
| Pocketing ≥ 5 mm with clinical signs of inflammation, which has not resolved using non-surgical methods | Any medical condition that contraindicates surgery |
| To facilitate placement of regenerative materials | Poor plaque control/motivation |
| Difficult access to root surfaces | Positive smoking status |
| Previous multiple failed attempts |
Two commonly used flap designs that allow access for RSD are discussed below and advantages of each technique are shown in Table 4-2.
| Advantages of simple replaced flap | Advantages of modified Widman flap (page 57) |
| Good access and visualisation of root surfaces and alveolar bone | Close adaptation of soft tissues to the root surfaces |
| Technically less demanding | Pocket depth can/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


