Foundations of Radiography, Radiographic Equipment, and Radiation Safety
Learning Outcomes
On completion of this chapter, the student will be able to achieve the following objectives:
• Pronounce, define, and spell the Key Terms.
• Describe uses of dental imaging.
• Name the highlights in the history of dental radiography.
• Describe the discovery of x-radiation.
• Explain what happens during ionization.
• Describe the properties of x-radiation.
• Explain how x-rays are produced.
• Label the parts of the dental x-ray tubehead and tube.
• Describe the effect of the kilovoltage on the quality of the x-ray beam.
• Describe how the milliamperage affects the quality of the x-ray beam.
• Identify the range of kilovoltage and milliamperage required for dental imaging.
• Discuss the effects of radiation exposure on the human body.
• Discuss the risks versus benefits of dental imaging.
• Identify the critical organs that are sensitive to radiation.
• Describe methods of protecting the patient from excess radiation.
• Describe measures used to protect the operator from excess radiation.
Electronic Resources
![]() Additional information related to content in Chapter 38 can be found on the companion Evolve Web site.
Additional information related to content in Chapter 38 can be found on the companion Evolve Web site.
Key Terms
ALARA concept Concept of radiation protection that states that all exposures should be kept “as low as reasonably achievable.”
Anode (AN-ode) The positive electrode in the x-ray tube.
Atom The basic unit of matter.
Bremsstrahlung radiation “Braking radiation.” The sudden deceleration of electrons as they interact with highly positively charged nuclei.
Cathode (KATH-ode) The negative electrode in the x-ray tube.
Central ray X-rays at the center of the beam.
Contrast Differences in degrees of blackness on an image.
Density The overall darkness or blackness of an image.
Dental radiography (ray-dee-OG-ruh-fee) The process of recording images of the teeth and adjacent structures by exposure to x-radiation.
Distortion Change in the size of an image caused by incorrect vertical angulation.
Dose (of radiation) The amount of energy absorbed by tissues.
Dosimeter A device used to detect and measure an accumulated dosage of radiation.
Electron A negatively charged particle in the atom.
Energy The ability to do work.
Extension arm Flexible arm that is attached to the x-ray tubehead.
Genetic (juh-NE-tik) effects Effects of radiation that are passed on to future generations through genetic cells.
Image Film-based or digitally produced recordings of anatomical structures
Image receptor A recording medium for an image, normally film. phosphor storage plate (PSP),—or a digital sensor.
Ion (EYE-on) An electrically charged particle.
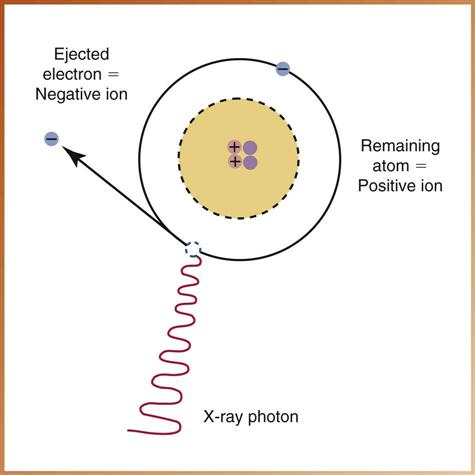
Ionization (eye-uh-ni-ZAY-shun) Process by which electrons are removed from atoms, causing the harmful effects of radiation in humans.
Ionizing (EYE-uh-nye-zing) radiation Radiation that produces ionization, resulting in harmful effects.
Kilovoltage (KIL-uh-voel-tuj) peak (kVp) Highest voltage of x-ray tube used during an exposure.
Latent (LAY-tent) period Time between exposure to ionizing radiation and appearance of symptoms.
Lead apron Device used to protect the reproductive and blood-forming tissues from scatter radiation.
Magnification The proportional enlargement of an image.
Master switch, indicator light, selector buttons, exposure button Components of control panel.
Matter Anything that occupies space and has form or shape.
Milliampere (mil-ee-AM-peer) (mA) One one-thousandth (1/1000) of an ampere; a unit of measurement used to describe the intensity of an electrical current.
Penumbra (puh-NUM-bruh) The blurred or indistinct area that surrounds an image.
Photon (FOE-ton) A minute (tiny) bundle of pure energy that has no weight or mass.
Primary beam The most penetrating beam produced at the target of the anode.
Primary radiation Same as primary beam.
Radiation Forms of waves of energy emission through space or material.
Radiation monitoring badge A device that contains a film packet used to detect and measure radiation exposure of personnel.
Radiograph (RAY-dee-oe-graf) Image produced on photosensitive film by exposing the film to radiation and then processing it.
Radiology (ray-dee-OL-uh-jee) The science or study of radiation as used in medicine.
Scatter radiation A form of secondary radiation that occurs when an x-ray beam has been deflected from its path by interaction with matter.
Secondary radiation X-radiation that is created when the primary beam interacts with matter.
Sensor A solid-state image receptor that contains a silicon chip with an electric circuit.
Sharpness A measure of how well an image reproduces the fine details or outline of an object.
Somatic (soe-MAT-ik) effects Effects of radiation that cause illness and are responsible for poor health (such as cancer, leukemia, and cataracts) but are not passed on to offspring.
Thyroid collar A flexible lead shield that is placed securely around the neck.
Tungsten target A focal spot in the anode.
X-radiation High-energy ionizing electromagnetic radiation.
The dental assistant must have a thorough knowledge and understanding of the importance and uses of dental imaging. Dental images are a necessary component of a comprehensive dental examination, as well as a part of the dental patient’s permanent record. Note: The term image receptor is used in this text when referring to either a digital imaging device or to film because the image is recorded on one or the other, depending on the system being used.
Dental imaging enables the dentist to see conditions that are not visible in the oral cavity and to identify many conditions that might otherwise remain undetected. Many dental diseases and conditions have no clinical signs or symptoms and are typically discovered only through the use of dental imaging.
To understand how dental images are produced, the dental assistant must first understand the fundamental concepts of atomic structure and have a working knowledge of ionizing radiation and the components of x-ray equipment. These are discussed later in this chapter.
Radiation, which is used to produce all types of dental images, has the ability to cause damage to all types of living tissues. Any exposure to radiation, no matter how small, has the potential to cause harmful biologic changes in the operator and the patient. The dental assistant must thoroughly understand the principles of safety when dealing with radiation.
This chapter provides a brief history of dental radiography and introduces you to radiation physics and the characteristics of radiation. You will learn the guidelines for radiation safety and methods used to protect the patient and yourself as the operator.
Discovery of X-Radiation
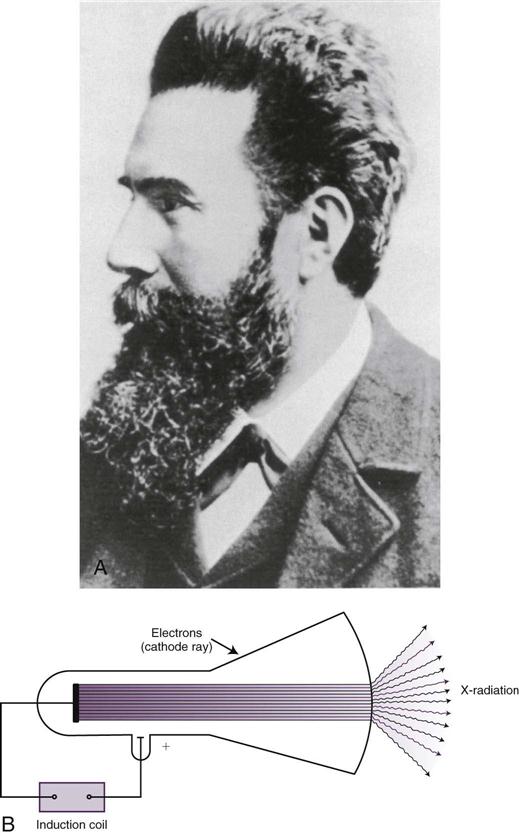
Wilhelm Conrad Roentgen (RENT-guhn), a Bavarian physicist, discovered the x-ray on November 8, 1895 (Fig. 38-1). This monumental discovery revolutionized diagnostic capabilities and changed the practice of medicine and dentistry forever.
Before discovering the x-ray, Roentgen had experimented with the production of cathode rays (streams of electrons). He used a Crookes tube (vacuum tube), an electrical current, and special screens covered with a material that glowed (fluoresced) when exposed to x-rays. While working in a darkened laboratory with a vacuum tube, Roentgen noticed a faint green glow (fluorescence) coming from some screens across the room. He realized that something was causing the glow and knew he had discovered a powerful and unknown ray. He named his discovery the x-ray. (The symbol x is used in mathematics to represent the unknown.)
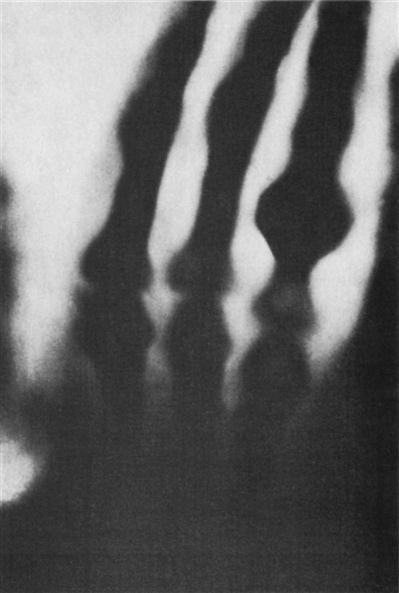
In the following weeks, Roentgen continued experimenting with the unknown rays. He replaced the fluorescent screens with photographic plates. He demonstrated that shadowed images could be permanently recorded on the photographic plate by placing objects between the tube and the plate. Roentgen placed his wife’s hand on a photographic plate and exposed it to the unknown rays for 15 minutes. When he developed the photographic plate, the outline of the bones in her hands could be seen, representing the first radiograph of the human body (Fig. 38-2).
To honor Wilhelm Roentgen for his discovery, for many years x-rays were referred to as roentgen rays, radiology was referred to as roentgenology, and radiographs were known as roentgenographs. During his lifetime, Roentgen was awarded many honors and distinctions, including in 1901 the first Nobel Prize ever awarded in physics.
Pioneers in Dental Radiography
Although Roentgen discovered the x-ray, others later helped to develop the field of dental radiography (Table 38-1). In fact, many of the early pioneers died from overexposure to x-rays. At the time x-rays were discovered, no one knew about the hidden dangers associated with the use of these penetrating rays.
TABLE 38-1
Highlights in the History of Dental Radiography
| Year | Event | Individual/Group |
| 1895 | Discovery of x-radiation | W.C. Roentgen |
| 1896 | First dental radiograph | O. Walkhoff |
| First U.S. dental radiograph (skull) | W.J. Morton | |
| First U.S. dental radiograph (live patient) | C.E. Kells | |
| 1901 | First paper on dangers of x-radiation | W.H. Rollins |
| 1904 | Introduction of bisecting technique | W.A. Price |
| 1913 | First dental text* | H.R. Raper |
| First prewrapped dental films | Eastman Kodak | |
| First x-ray tube | W.D. Coolidge | |
| 1920 | First machine-made film packets | Eastman Kodak |
| 1923 | First dental x-ray machine | Victor Radiograph |
| 1925 | Introduction of bitewing technique | H.R. Raper |
| 1933 | Proposal of rotational panoramics concept | |
| 1947 | Introduction of long-cone paralleling technique | F.G. Fitzgerald |
| 1948 | Introduction of panoramic radiography | |
| 1955 | Introduction of D-speed film | |
| 1957 | First variable-kilovoltage dental x-ray machine | General Electric |
| 1978 | Introduction of dental xeroradiography | |
| 1981 | Introduction of E-speed film | |
| 1987 | Introduction of intraoral digital radiography | |
| 1999 | Oral and maxillofacial radiology recognized as a dental specialty | American Dental Association |
| 2001 | Introduction of F-speed intraoral film | Eastman Kodak |
| 2003 | Introduction of cone beam 3-D technology |
*Modified from Iannucci J, Jansen Howerton L: Dental radiography: principles and practice, ed 4, St Louis, 2012, Saunders.
In 1895, German dentist Otto Walkhoff made the first dental radiograph. He placed a glass photographic plate wrapped in black paper and rubber in his mouth and submitted himself to 25 minutes of x-ray exposure. Also in 1895, a New York physician made the first dental radiograph in the United States using a skull.
New Orleans dentist C. Edmund Kells is credited with the first practical use of radiographs in dentistry in 1896. During his many experiments, Dr. Kells exposed his hands to x-rays every day for years. This overexposure to x-radiation caused numerous cancers to develop on his hand. His dedication to the development of dental radiography eventually cost Dr. Kells his fingers, later his hand, and then his arm. After enduring much pain and faced with the prospect of becoming a burden to his family, he committed suicide in 1928.
Dental radiography has progressed from these early discoveries to its current status as an invaluable science. New technology continues to improve dental imaging capabilities.
Radiation Physics
All things in the world are composed of energy and matter. Energy is defined as the ability to do work. Although energy cannot be created or destroyed, it can change form. Atoms are the basic form of matter, and they contain energy. Matter is anything that occupies space and has form or shape.
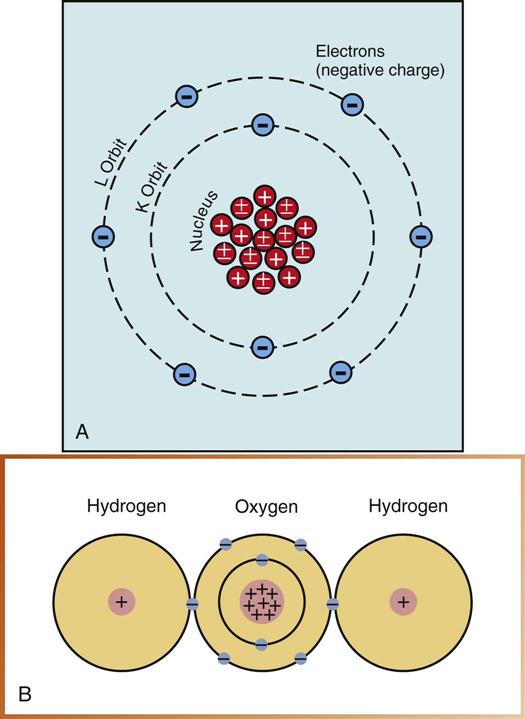
Matter has many forms, including solids, liquids, and gases. Matter is composed of atoms grouped together in specific arrangements called molecules (Fig. 38-3). A molecule is the smallest particle of substance that retains the property of the original substance (see Fig. 38-3, B). The fundamental unit of matter for discussion in this chapter is the atom (see Fig. 38-3, A).
Atomic Structure
The atom consists of two parts: a central nucleus and orbiting electrons (see Fig. 38-3, A). An atom is identified by the composition of its nucleus and the arrangement of its orbiting electrons. The arrangement within the atom is similar to that of the solar system: The atom has a nucleus (sun) at its center, and the electrons (planets) revolve (orbit) around the nucleus. Electrons remain stable in their orbit unless disturbed or moved. X-rays can disturb the orbiting electrons.
Nucleus
The nucleus, or dense core of the atom, is composed of particles known as protons and neutrons. Protons carry positive electrical charges, whereas neutrons carry no charge.
Dental x-rays do not affect the tightly bound nucleus of the atom and are changed only in direction, or scattered. Dental x-rays cannot make atoms radioactive; that is, patients do not give off x-rays after the x-ray machine stops producing x-rays.
Electrons
Electrons are tiny, negatively charged particles that have very little mass. The orbital path of an electron around the nucleus is called an electron shell. Each shell can contain only a specific number of electrons. Electrons are maintained in orbit by electron binding energy, a force similar to gravity.
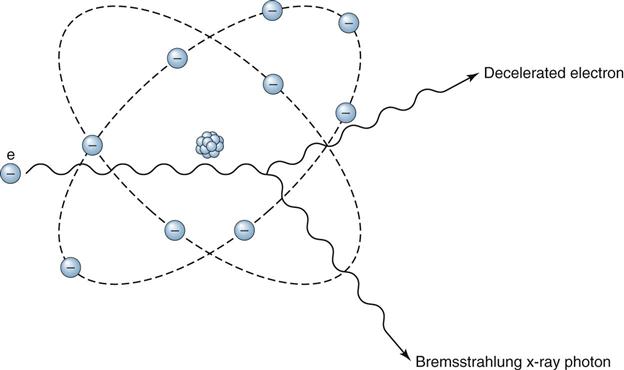
Bremsstrahlung Radiation
Bremsstrahlung radiation is produced when an electron passes near the nucleus of an atom. The negatively charged (−) electron is deflected by the positively charged (+) nucleus. Energy lost by deceleration of the electron is emitted in the form of a photon of radiation called bremsstrahlung (from the German word for “braking”). Braking radiation is the primary kind of radiation produced in the dental x-ray tubehead (Fig. 38-4).
Ionization
Electrons remain stable in their orbit around the nucleus until radiograph photons collide with them. A photon is a minute (tiny) bundle of pure energy that has no weight or mass.
Ions are atoms that gain or lose an electron and become electrically unbalanced. X-rays have enough energy to produce ions because of a process called ionization. In this process, electrons are removed from the orbital shells of electrically stable atoms through collisions with x-ray photons (Fig. 38-5).
Properties of X-Rays
The dental assistant must be familiar with the unique characteristics of x-rays (Box 38-1). X-rays are a form of energy that can penetrate matter. X-rays belong to a group classified as electromagnetic radiation (Fig. 38-6). Visible light, radar, radio, and television waves are also classified as electromagnetic radiation. Electromagnetic radiation is made up of photons that travel through space at the speed of light in a straight line with a wavelike motion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses