Aesthetic Alteration of the Nose
Evaluation and Surgery
• Classic Rhinoplasty Maneuvers
• Facial versus Nasal Proportions and Effects on the Aesthetic Perspective
• The Nasal Airway: Anatomy and Physiology
• Anatomic Locations and Causes of Nasal Obstruction
• Evaluation of the Nasal Airway
• Surgical Approach to Open the Nasal Airway
• Outcome Assessment of Surgery to Improve Nasal Breathing
• Initial Rhinoplasty Consultation
• Definitive Rhinoplasty Planning
• Open versus Closed Approach to the Nose
• Complications Associated with Rhinoplasty
• Primary Septorhinoplasty: Step-by-Step Approach
• Congenital and Posttraumatic Saddle-Nose Deformities
• Cocaine-Related, Autoimmune and Iatrogenic Saddle-Nose Deformities
Nasal Surface Anatomy
The external nose may be described as consisting of three parts: the osseocartilaginous vault, the lobule/tip, and the base (Fig. 38-1).
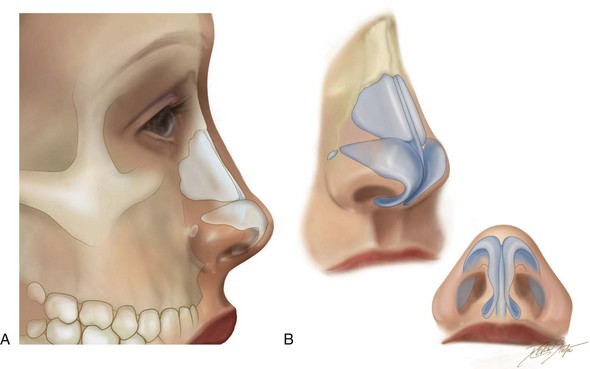
Figure 38-1 A, Illustration of the soft tissues and skeletal anatomy of the nose as seen in profile view. B, Illustration of the skeletal anatomy of the external nose and the lower lateral cartilages as seen in three-quarter and worm’s-eye views.
The osseocartilaginous vault consists of the bony vault (the nasal bones, the nasal process of the frontal bones, and the nasal process of the maxilla) and the cartilaginous vault (the upper lateral cartilages [ULCs] and the dorsal aspect of the cartilaginous septum). The transition from bony to cartilaginous dorsum is called the keystone area.49 The caudal aspects of the nasal bones overlap the cephalic portions of the ULCs in the keystone area. The width of the nasal bones and ULCs is greater in the keystone area than at either the radix or the supratip regions.
To the experienced clinician, the appearance of the external nasal anatomy will give an indication of the anatomic causes of subjective nasal airway obstruction.249 Middle-vault collapse, pinched nasal sidewalls, asymmetric nostrils, and a crooked dorsum are all outward indications of obstructions to nasal airflow; this is discussed later in this chapter.
Classic Rhinoplasty Maneuvers
Classic rhinoplasty maneuvers include the following 1) nasal osteotomies (i.e., to reduce the nose’s width, to straighten a crooked nose, and to close an open roof) 2) dorsal reduction (bone and cartilage) 3) the selective removal of cephalic portions of the lower lateral crura (maintenance of 6 mm of caudal rim) 4) suturing of the LLCs (i.e., interdomal and transdomal areas) and 5) augmentation with cartilage grafts (i.e., caudal strut graft, alar contour grafts, lateral crural strut grafts, shield tip graft, columellar tip graft, spreader grafts, dorsal strut graft).47,51,69,93,138,142–144,182,207,219,237
Grafts are indicated when other lesser maneuvers to improve the projection and definition of the nasal tip are not adequate.* When indicated, a graft that will be used to alter the nasal tip can be fashioned from removed quadrangular cartilage or from another source (e.g., the conchal floor, the rib cartilage).201 A caudal strut graft remains the workhorse for the addition of support to weak LLCs and for the control and maintenance of the nasal tip position. The caudal strut graft also functions as a central scaffold on which the tip structures can be unified. When a shield tip graft is used, it is placed over the domes with the inferior margin extending to the mid columella. A shield graft is effective for increasing infratip lobular definition and projection. Columellar tip grafts extend superiorly and are often secured to the ULC above and the caudal margin of the medial crura below. They are more useful in thick-skinned individuals in whom there is an additional need to improve tip definition beyond the usual rhinoplasty maneuvers. In thin-skinned individuals, tip grafts are only used cautiously, because they may result in visible irregularities.
Interdomal sutures are placed in mattress fashion in the region of the middle crura.89,98,199 This suturing technique is effective for reducing interdomal distance and thereby increasing tip projection and refinement. Medial crural fixation sutures are placed to unify the medial crura beneath the domes of the LLC and to reduce flaring. These sutures are typically placed after a caudal strut graft is secured. Transdomal sutures are placed in a horizontal mattress fashion and then across the dome of the middle crura. All of these suture techniques can be effective to alter the tip position, to narrow the distance between the tip-defining points, and to correct domal asymmetries.
Spreader grafts may be either horizontal or vertical, and they are used to correct deficiencies of the cartilaginous vault.24,38,46,87,88,92,95,97,208,209,255 Vertical spreader grafts are generally paired and extend from just deep to and then flush with the nasal bones. They are secured on each side of the dorsal septum and then generally to the ULCs with sutures. The caudal end of each vertical spreader graft may continue beyond the septal angle and below the LLCs to elongate the nose and to derotate the tip. They are typically 15 to 20 mm in length and approximately 2 to 4 mm in width. A horizontal spreader graft is a single dorsal graft that is inset between the ULCs and that forms a “T” with the dorsal septum. Spreader grafts are used as a technique to prevent or correct the narrowing of the internal nasal valve, to preserve or correct the nasal dorsum or dorsal aesthetic lines, and to correct and stabilize a “crooked” dorsal septum.
There are four aspects of the nasal base that may be considered for surgical modification5:
1. Selective reduction of the caudal aspect of the quadrangular cartilage (septum) may be completed to limit columella show in profile. Augmentation of the deficient caudal septum may be required after overaggressive rhinoplasty or to reconstruct congenital deficiencies (e.g., Binder syndrome).
2. Modification of the anterior nasal spine may be carried out to alter the nasolabial angle or to augment a congenital deficiency (e.g., Binder syndrome).
3. Deepening of a high nasal floor and widening of narrow pyriform apertures by recontouring (e.g., using a rotary drill with a bur) may be indicated to improve the airway and to enhance aesthetics (i.e., in those with a long face growth pattern). Augmentation of this region may also be carried out to reconstruct a deficiency (e.g., Binder syndrome, alveolar clefting).
4. A cautious approach to excision of the alar rims (i.e., Weir excisions) may be performed to achieve a preferred interalar width (i.e., just less than the intercanthal width). It is preferred to accept a slightly increased interalar width rather than to end up with an “operated” look from either overresection of the rims or resulting scarring.
Facial versus Nasal Proportions and Effects on the Aesthetic Perspective
The surgeon must distinguish between the aesthetics of the nose (i.e., nasal proportions) and the aesthetics of the face (i.e., overall facial proportions) (Fig. 38-2).* Establishing the Euclidean proportions of the full face represents a different aesthetic objective than simply establishing pleasing proportions of the nose as an isolated aesthetic unit. The individual who is seeking rhinoplasty often perceives that his or her aesthetic objectives can be met by addressing the nose only. In these circumstances, after cosmetic rhinoplasty, the surgeon may be pleased with improvements in the nasal aesthetic unit, but the patient may express displeasure with the results. This will more frequently occur in the individual with either a long face growth pattern, a short face growth pattern, or an isolated sagittal mandibular deficiency growth pattern who perceives that he or she still has a “big” nose, even after rhinoplasty (Fig. 38-3). The patient may have initially sought out a cosmetic surgeon and requested a rhinoplasty with the goal of achieving a “smaller” nose. The surgeon may create a well-proportioned nasal aesthetic unit, but the nose may still remain “big” in proportion to the rest of the face. The surgeon may then be asked to revise the rhinoplasty to create a “smaller” nose.192,193 When the surgeon further reduces the nasal bones and cartilage beneath the soft-tissue envelope, an “operated” look may result, and the overall facial proportions may move even further out of balance.
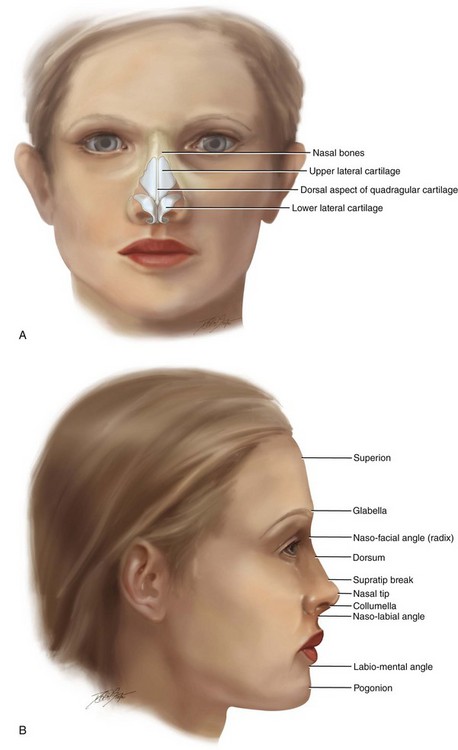
Figure 38-2 A, Frontal and B, profile views of a well-proportioned face, including the underlying skeletal anatomy, are illustrated.


Figure 38-3 The clinician must distinguish between the aesthetics of the nose (i.e., the nasal aesthetic proportions) and the aesthetics of the face (i.e., the facial aesthetic proportions). Establishing the Euclidean proportions of the overall face represents a different aesthetic objective than simply establishing pleasing proportions of the nose as an isolated aesthetic unit. The individual who is seeking rhinoplasty often perceives that his or her objectives can be met by addressing the nose only. Errors in aesthetic judgment are especially frequent when viewing an individual with the following uncorrected issues: 1) a long face growth pattern (see Chapter 21); 2) a primary mandibular deficiency growth pattern (see Chapter 19); 3) a short face (maxillomandibular deficiency) growth pattern (see Chapter 23); or 4) a maxillary deficiency with a relative mandible excess growth pattern (see Chapter 20). Four case examples are shown to illustrate the importance of aesthetic perspective. A, A woman in her mid 20s with a long face growth pattern is shown before and after undergoing successful orthognathic surgery to correct facial disproportion. Before surgery, the nasal aesthetic unit was reasonably well proportioned but appeared “big” when viewing the face in profile. After successful orthognathic surgery, the same nose appears well proportioned with respect to the rest of the face. The procedures performed included Le Fort I osteotomy, sagittal split ramus osteotomies, and osseous genioplasty (see Fig. 21-5). B, A woman in her late 20s requested the evaluation of a “big” nose and a “small” chin. After successful orthognathic correction, which included sagittal split ramus osteotomies and osseous genioplasty the nose appears well proportioned with respect to the rest of the face (see Fig. 19-7). C, A teenage girl with a short face growth pattern (maxillomandibular deficiency with excess overjet) had previously undergone orthodontics to neutralize the occlusion. She complains of a “big” nose and a “small” chin. She is shown before and after successful orthognathic surgery that included Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation), sagittal split ramus osteotomies (horizontal advancement, and clockwise rotation), and osseous genioplasty (vertical lengthening). After surgery, the nose no longer appears big and is well proportioned with respect to the rest of the face (see Fig. 23-2). D, A 20-year-old college student with a maxillary deficiency and a relative mandibular excess growth pattern arrived for a surgical evaluation with complaints of a “big” nose and “prominent” chin. He is shown before and after successful orthognathic surgery. The patient’s procedures included Le Fort I osteotomy (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation) and sagittal split ramus osteotomies (clockwise rotation). After surgery, the nose no longer appears to be prominent, and the chin region of the lower jaw assumes improved proportions within the face (see Fig. 20-4).
The Nasal Airway: Anatomy and Physiology
Symptomatic nasal obstruction is a condition in which the individual feels that he or she has inadequate nasal airflow. Although it is a subjective feeling, it should have a foundation in objective anatomic and physiologic findings (Fig. 38-4). Knowledge of both nasal anatomy and physiology is required for the accurate diagnosis and treatment of the subjective sensation of obstructed nasal breathing.*
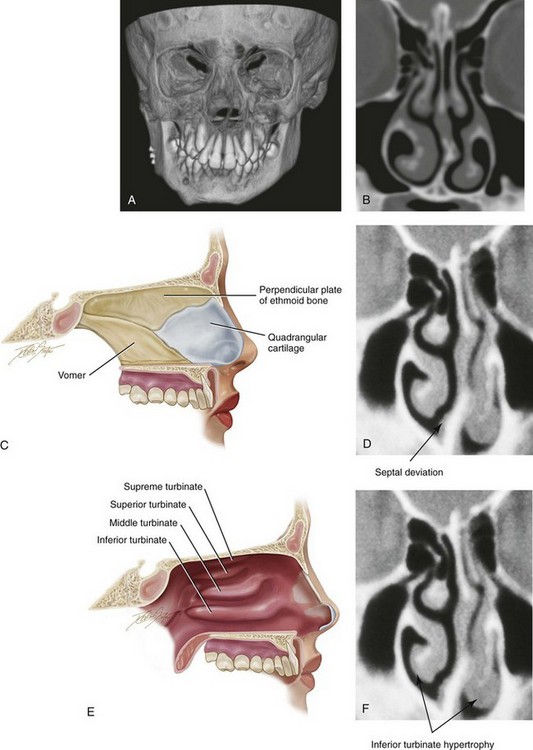
Figure 38-4 A, A three-dimensional computed tomography (CT) scan view of a mixed-dentition skeleton with a deviated septum. B, A coronal CT view through the nasal cavity and maxilla demonstrates a deviated septum and enlarged inferior turbinates. C, A sagittal section through the nasal cavity and the maxilla is illustrated. The anatomy of the septum is highlighted. D, A CT scan through the nasal cavity (coronal cut) demonstrates a deviated septum. E, A sagittal section through the nasal cavity and the maxilla is illustrated. The anatomy of the turbinates is highlighted. F, A coronal CT view through the nasal cavity demonstrates a deviated septum and enlarged inferior turbinates.
Bony Anatomy
The anterior (pyriform) aperture generally represents the narrowest bony aspect of the nasal airway.123 Its anatomic boundaries include the paired nasal bones (i.e., the nasal pyramid), which join to the ascending process of the maxilla laterally. The bony floor of the nose is formed by the superior aspect of the premaxillary alveolus anteriorly and the secondary palate posteriorly. The anterior nasal spine is in the anterior midline of the nasal floor, and the posterior nasal spine is in the posterior midline of the nasal floor. These spines provide the anterior and posterior limits of the inferior aspect of the cartilaginous and bony septum, respectively.
Cartilaginous Anatomy
The cartilaginous anatomy of the nose also includes the paired ULCs, the paired LLCs, and the variable sesamoid cartilages (see Fig. 38-1). The ULCs are trapezoidal in shape and articulate with the nasal bones superiorly, with the quadrangular cartilage over the midline dorsum, with limited connections laterally to the bony pyriform aperture, and also to small sesamoid cartilages inferiorly. The LLCs connect to the ULCs superiorly via fibrous tissue. The LLCs are responsible for much of the form and shape of the nasal tip and the ala. Components of the LLC include the medial, middle, and lateral crura (see Fig. 38-4).
Intranasal Anatomy
Within the nose, sites of obstruction tend to occur at specific locations, including the external nasal valves, the internal nasal valves, the turbinated cavities, and the posterior nasal (choanae) apertures (see Fig. 38-4).
Nasal Physiology and Function
The five major functions of the nose are respiration, filtration, humidification, protection, and temperature regulation. Filtration is accomplished through the vibrissae (located in the vestibule) and the mucosal cilia, which line the airway. Humidification and temperature regulation of the air are controlled by specialized vascular tissues that are regulated by sympathetic and parasympathetic nerve fibers. The capillary system is supplemented by venous sinuses that may constrict and result in enlargement, especially of each inferior turbinate.103 Protection from bacteria and viruses is both mechanical and chemical. Chemical protection is provided by immunoglobulin A and muramidase, which are found in the mucus on the membranes of the nasal cavities. Mechanical clearing of trapped organisms is provided by the beating cilia, which move the mucous blanket into the nasopharynx every 20 minutes. During respiration, the nose resists the inspiration of air by providing almost 50% of the total airway resistance.
Anatomic Locations and Causes of Nasal Obstruction
External Nasal Valve
Common causes of static narrowing of the external nasal valve include alar malpositioning or scarring of the skin or nasal vestibule, caudal septal deflections, and nasal tip ptosis (see Fig. 38-4).77 These may be seen after overzealous cleft lip nasal procedures. Dynamic collapse of the external nasal valve may be the result of weakened or deficient LLCs and nasal ala. During rhinoplasty, external nasal valve collapse is generally prevented by avoiding overaggressive resection of the LLCs and by preserving the soft-tissue support of the mobile alar walls. Secondary reconstruction to correct this deformity requires cartilage support grafts that are applied to the LLCs.
Posterior Nasal (Choanae) Apertures
Obstruction of the posterior nasal apertures may result from the skeletal structures that compose the choanae (i.e., the vomer and the palatine bones) or from the overlying soft tissues (i.e., polyps, adenoids, and turbinates).210 Choanal atresia may also be associated with congenital anomalies such as CHARGE syndrome, Treacher Collins syndrome, and Apert syndrome.
Evaluation of the Nasal Airway
Nasal airway resistance is greatly affected by the inferior turbinates, which periodically swell and decrease the internal valve area. Inferior turbinate hypertrophy may be physiologic or pathologic. For the majority of the population, a normal “nasal cycle” of the congestion and decongestion of the turbinates and the nasal mucosa is ongoing, with reciprocal changes on the two sides. The total nasal airway resistance in the healthy nose is remarkably constant, with changes occurring every 2 to 4 hours in the turbinates and the mucosal lining. When the inferior turbinates are markedly enlarged and when the process is not reversible with the use of vasoconstrictors and anti-inflammatory agents, then surgical reduction of the turbinate hypertrophy (often in combination with septoplasty) is the treatment of choice and will generally relieve the symptoms. Doing so will often open the internal nasal valve and the whole turbinated cavity. A variety of surgical techniques are used to accomplish the goal of inferior turbinate reduction (e.g., partial excision, electrocautery, submucosal resection, radiofrequency ablation, microdebridement).157,173 The overaggressive resection of the inferior turbinates has, on occasion, resulted in rhinitis sicca or “dry nose.”
Outcome Assessment of Surgery to Improve Nasal Breathing
Attempts to objectively measure alterations in nasal function after medical or surgical interventions that are carried out for the purpose of improving nasal breathing have proven to be difficult.31,113–115,118,128,152,171,185,187,189,190,195,215,222,223,226,243 Through acoustic rhinometry and rhinomanometry, attempts at objective postoperative assessments of the nasal airway have been carried out. Consistent findings with the use of these measurement techniques are mixed at best. A spectrum of studies by different investigators has demonstrated conflicting results with similar research designs. Studies by Lindemann and colleagues confirm that nasophysiologic functions (e.g., the heating and humidifying of inspired air) were improved after successful septoplasty and appropriate inferior turbinate reductions.126 This positive effect is believed to be derived from increased volumes and the direction of physiologic airflow to key places within the nasal passage, which increases mucosal contact with the nasal airstream. The improved flow dynamics may also improve the filtration of particulate matter more effectively.
In addition to objective instrumentation measures of nasal breathing, researchers have sought a standardized assessment of results from the patient’s perspective. These efforts have taken the form of symptom-based questionnaires. The most rigorously developed disease-specific measure for nasal obstruction was created by the Nasal Obstruction Symptom Evaluation (NOSE) study investigators.233,234 The NOSE Scale generates an integral patient-specific score out of a possible 100 points and thus facilitates quantitative comparisons within subjects at different time points or among groups of subjects who are undergoing different treatments. The NOSE Scale is now considered the reference standard for the assessment of alterations in nasal breathing. Considering the extent of nasal obstructive treatment carried out in the United States alone, which is estimated to cost $5 billion per year, emphasis on standardization and measurable results seems to be indicated (see Chapter 10).
Initial Rhinoplasty Consultation
Difficulty with breathing through the nose is often chronic, with a longstanding mouth-breathing habit. If this is the case, the facial morphology may be that of a long face growth pattern (i.e., vertical maxillary excess typically with an anterior open-bite Class II malocclusion; see Chapter 21). The obstructive nasal breathing is often made worse in the presence of chronic allergies or with ambient changes in humidity. Examination of the internal nose may reveal septal deviations or perforations, external valve stenosis, internal nasal valve obstructions, posterior nasal aperture stenosis, turbinate enlargement, or an irritated nasal mucosal lining. Consideration should also be given to the adenoids and tonsils, which may be enlarged and obstructive. The internal nasal valves, the turbinated cavities, the external nasal valves, and the posterior nasal aperture may be obstructed by any one of a number of anatomic structures (e.g., turbinates, septum, ULC, LLC, nasal skeletal walls or floor, soft tissues).
It is also essential for the surgeon to understand the patient’s psychological reasons for requesting surgery on the nose and then to assess that patient’s emotional maturity and stability. Constantian has outlined specific red flags for the surgeon to be concerned about, including the patient who is seeking surgery for specific external gain (e.g., an individual who expects that nasal changes will improve his or her career); the narcissistic male; and the perfectionist.41 He also warns against operating on an individual whom “you just don’t like” (i.e., with whom you are not able to effectively communicate). Picavet and colleagues documented a high prevalence of body dysmorphic disorder symptoms among patients who are seeking rhinoplasty (see Chapter 7).176 Individuals who request revision rhinoplasty and those with a psychiatric history are particularly at risk for ongoing dissatisfaction.
Definitive Rhinoplasty Planning
Basic questions for the surgeon to consider include the following:
• Are there any medical or psychosocial contraindications to elective nasal surgery?
• What are the functional nasal findings? Do they correlate with the patient’s symptoms?
• Are there associated maxillomandibular disproportions that affect the individual’s facial aesthetics?
• What aspects of the patient’s nose would the surgeon like to change?
• Given the quality of the patient’s overlying nasal skin and the underlying skeletal and cartilaginous structures, what are the reasonable surgical options?
• Do the patient’s requests match the surgeon’s thoughts when taking into account any biologic limitations of the tissues?
• Does the surgeon think that he or she can interact effectively with the patient should a complication or suboptimal result occur?
Open versus Closed Approach to the Nose
In the hands of a limited number of experienced nasal surgeons, the closed (endonasal) approach to gain exposure of the nose allows for the predictable management of the patient’s needs.91,198,202,217–221 In this author’s clinical practice, the open (columella-splitting and bilateral marginal incisions) approach provides the preferred direct exposure of the nasal structures in most patients. After elevation of the nasal soft-tissue envelope via an open approach, direct inspection of the osseocartilaginous framework and tip should confirm the preoperative clinical diagnosis. This direct exposure facilitates technical maneuvers such as the following: 1) bony and cartilaginous reduction 2) excision and suturing of the LLCs 3) the placement and stabilization of grafts and 4) septal modification. By understanding normal nasal physiology and what the osseocartilaginous framework and nasal tip should look like and then seeing the anatomy under direct vision, the intended results are achieved more often than not.
As pointed out by many authors, the open approach has advantages that include the following3,4,33,50,72–76,84,91,101,112:
1. Securing a cartilage (strut) graft to the caudal septum to help control or maintain the tip position
2. Suturing the middle crura to each other and then over the top of the secured caudal (strut) graft to improve tip projection and shape
3. Controlling the columellar–lobular angle by altering the axis of the caudal strut graft
4. Suturing additional nasal tip grafts in place over the top of the LLCs
5. Accurately placing and securing spreader grafts to correct nasal valve collapse, to straighten the nose, and to correct saddle deformities
6. Placing and suturing cartilage grafts to reinforce, change the shape of, or replace missing segments of the lateral crura
7. Placing and securing onlay grafts (over the bony or cartilaginous vault) to reconstruct or augment the dorsum of the nose
8. Visualizing and then reducing the bony and cartilaginous nasal dorsum
9. Visualizing and then reducing or modifying the radix, including the placing and securing of grafts
Complications Associated with Rhinoplasty
Fortunately, in the hands of an experienced nasal surgeon, the vast majority of well-informed patients undergo an uneventful operative and postoperative course and are pleased with their initial and long-term function and their aesthetic results. However, as with any surgical procedure, perioperative problems may occur (e.g., infection, bleeding, airway compromise) in addition to problems that are specific to rhinoplasty (e.g., septal perforation, persistent nasal obstruction, suboptimal cosmetic results).* These potential problems must be considered and openly discussed in advance to limit patient dissatisfaction.
Infection
Infection occurs in approximately 1% of patients who are undergoing elective rhinoplasty.35,37,54,83,109,129,166 The routine use of prophylactic antibiotics that are started just before surgery and continued postoperatively (at least until all internal nasal packs have been removed) is recommended. If infection occurs, appropriate drainage and culturing of the fluid is carried out. The antibiotic regiment is altered, as indicated.
Airway Obstruction
The assessment of nasal breathing and of the entire upper airway should be carried out and the findings discussed with the patient and the family before rhinoplasty occurs.16,18,20,43,94,111,150,151,194,214 The importance of doing this has been confirmed by Thomson240 and Hellings,104 who independently reported the presence of persistent nasal airway obstruction as a frequent complaint that leads to need for revision rhinoplasty. The nasal airway may also be compromised as a result of rhinoplasty. Synechiae may form between the septum, the lateral nasal wall, or the turbinates and require release in the office or, occasionally, in the operating room. Residual septum deflections may require removal. Further turbinate reduction may also be advantageous. The clinician should not ignore the nasal airway if a favorable result and a satisfied patient are desired.
Dry Nose Syndrome
Atrophic rhinitis is uncommon, but it may be seen after turbinate reduction.59,149 There may be gradual and progressive atrophy of the nasal mucosa with a lack of moistening secretions that leads to crusting that accumulates. The crusts harbor bacteria; when this is associated with poor aeration and drainage, an unpleasant odor (ozena) may result.
Burn Injuries
The occurrence of operating room fires and airway burns is rare. Nevertheless, there is a risk of ignition in the operating room with any application of electrocautery or lasers. This risk is increased in the setting of nasal-cannula or face-tent supplemental oxygen. It can also be a problem in the intubated patient in whom there is an “air leak.” Facial burns, intraoral and intra-airway burns, and even patient demise have all been reported. Although burn injuries in the operating room are rare, they represent approximately 20% of all malpractice claims for cases performed under monitored anesthesia care, and 95% of these cases involve surgery of the head and neck.196
Patient Dissatisfaction
Studies indicate that, on average, 15% of patients who have undergone cosmetic rhinoplasty procedure will express at least some dissatisfaction with the result.* In general, rhinoplasty patients differ from facial aging patients with regard to their psychological complexity. Most individuals who are seeking rhinoplasty have always been dissatisfied with some aspect of their facial appearance, which they attribute to nasal dysmorphology. Alternatively (at least in theory), the adult facial aging patient is seeking rejuvenation to restore a previous “satisfactory” appearance. The rhinoplasty patient is more likely motivated by lifelong body-image undercurrents that mold his or her perception of the nasal appearance. This will influence his or her expectations for surgery in a way that different from those of the facial aging patient.
Adamson and colleagues report that patients who request primary rhinoplasty commonly cite their rationale as including a “dorsal hump” (50%); a “too large” nose (44%); a bulbous tip (41%); and an “obstructed nasal airway” (33%).32 Because half of the patients seeking primary rhinoplasty cited a “dorsal hump” as the chief concern, the achievement of an aesthetically pleasing nasal profile is essential. This is contingent on a thorough understanding of the underlying nasal anatomy and a complete facial analysis, which includes the assessment of the true dorsal hump as well as looking for the presence of a deep radix or an underprojected tip. Care should also be taken to establish a pleasing contour and transition between the dorsum and the tip (i.e., the supratip break) and to prevent iatrogenic deformities (i.e., supratip “Polly beak” deformity). Other surgical causes of patient dissatisfaction include cartilage graft warping, resorption, and palpability. Another frequent reason for a primary rhinoplasty consult is a nose that is “too large” (44%). The achievement of a good nasal profile will therefore frequently depend not only on the anatomy of various nasal parts but also on the interplay of the other facial parts (i.e., the maxilla, the mandible, and the chin region). The discerning clinician must separate out these aspects (i.e., dentofacial disharmony versus nasal disharmony) if patient satisfaction and a favorable outcome are to be achieved (see Chapters 19 through 23 and Fig. 38-2).
Rohrich and colleagues pointed out the importance of understanding the psyche of the male rhinoplasty patient.200 These patients are more likely to present with nonspecific complaints, to be more demanding of the end result, and to be less attentive during the consultation visit. The clinician must painstakingly set clear and realistic expectations of the operation to achieve patient satisfaction. These authors recommend allowing 6 to 12 months of healing before agreeing to further nasal modifications. In most reported series, only 50% of patients who undergo revision rhinoplasty will move into the satisfied category.41
Primary Septorhinoplasty: Step-by-Step Approach (Figs. 38-5 through 38-9)
Preparation and Draping
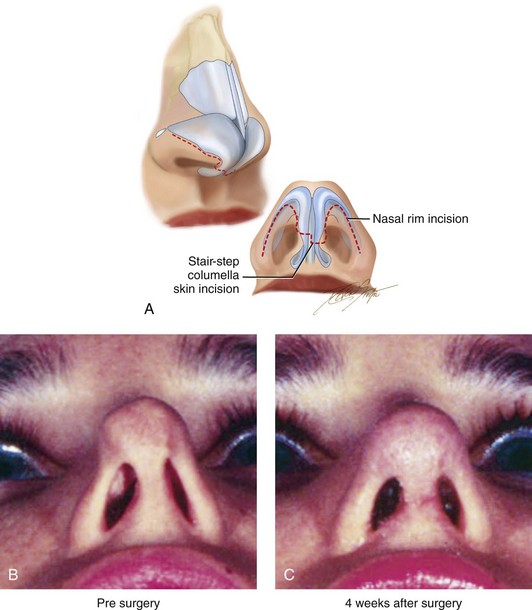
Figure 38-5 Incisions that are used for an open technique rhinoplasty are demonstrated. A, Stair-step columella (skin) and bilateral (intranasal) rim incisions are illustrated in two views. B, Worm’s-eye views of the nose before and C, 4 weeks after an open-technique secondary rhinoplasty. Four weeks after surgery, the skin incision is immature (i.e., red and raised), and the soft tissues remain swollen.
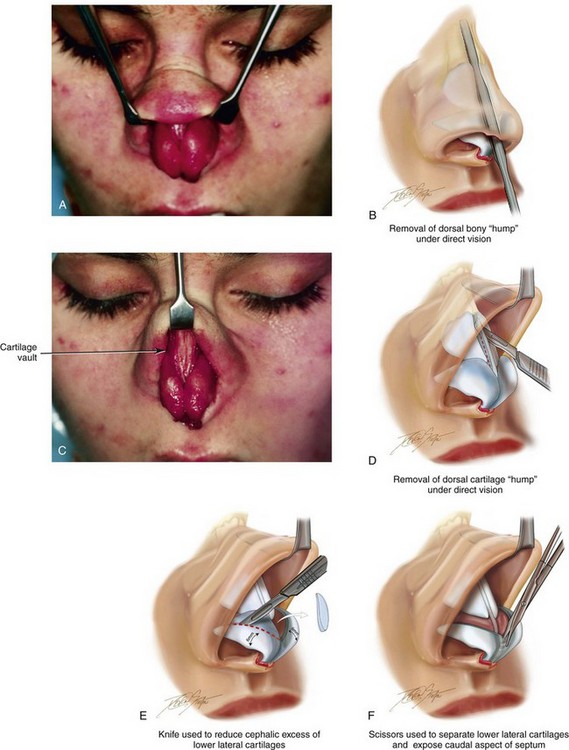
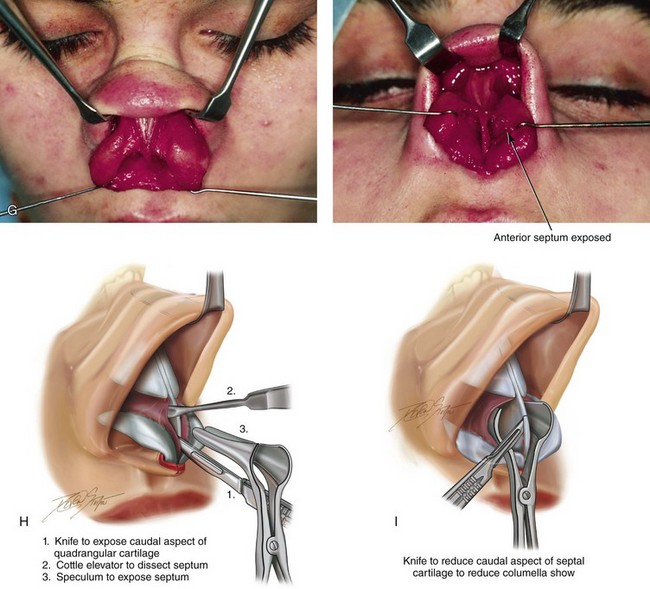
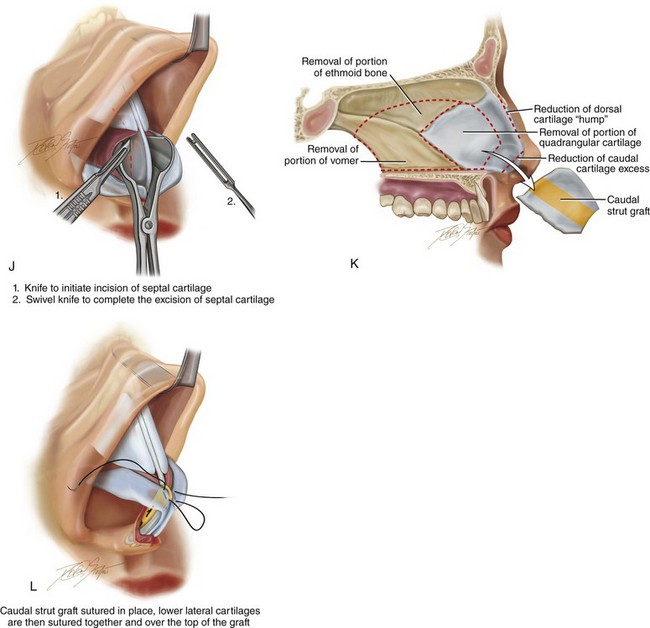
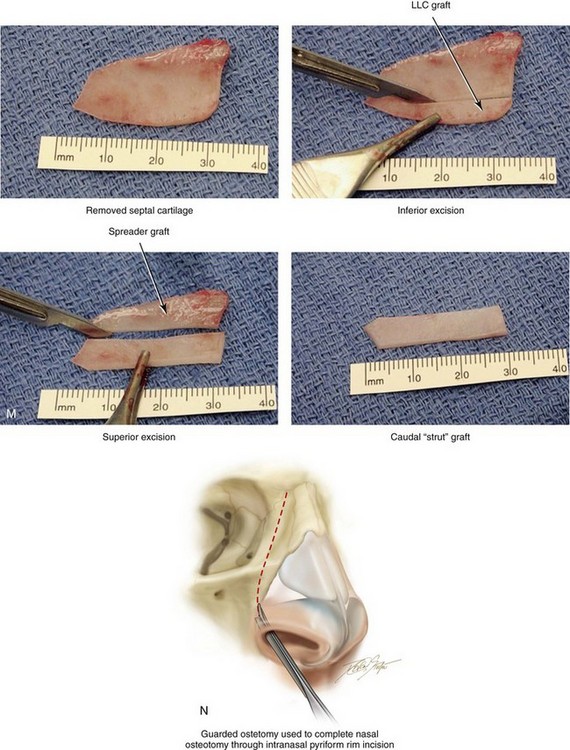
Figure 38-6 A, Exposure of the deep structures, including the lower lateral cartilages (LLCs), as viewed through an open approach after the elevation of the soft-tissue envelope of the nose. B, A rasp is used to reduce the bony dorsum of the nose. C, The upper lateral cartilages and the dorsal aspect of the quadrangular cartilage are also directly visualized through the open approach. D, Dorsal bone reduction (as described in B) is followed by the sharp knife excision of the cartilaginous dorsal hump. The illustration shows the Aufricht retractor in place, with a knife (no. 15 blade) used to excise excess dorsal septal cartilage. E, Measurement of the LLCs is carried out with a caliper. In general, a 6-mm caudal rim of LLC is maintained. The cephalic excess is incised with a knife (no. 15 blade) and then removed with a Stevens scissors. F, An illustration that shows the scissors dissection to separate the LLCs and to expose the caudal aspect of the quadrangular cartilage. G, Two intraoperative views show the LLCs separated to expose the caudal aspect of septum. H, An illustration that shows the following: 1) a knife (no. 15 blade) that is used to remove the final layer of perichondrium from the caudal edge of the septal cartilage before subperichondrial dissection; 2) a Cottle elevator that is used for exposure of the quadrangular cartilage and bony septum (i.e., vomer and ethmoid); and 3) a speculum that is inserted with a blade placed on each side of the septum. I, If there is excess columella show, then the caudal aspect of the quadrangular cartilage is reduced (excised) to improve aesthetics. The illustration demonstrates the planned caudal reduction. J, An illustration showing an incision through the quadrangular cartilage to initiate submucous resection. It is important to maintain an uninjured and adequate dorsal and caudal strut of cartilage to structurally support the nose. (1) A knife (no. 15 blade) is used to initiate the incision in the septal cartilage. (2) A swivel knife will then be introduced to complete the actual submucous resection of the septal cartilage. The cartilage excision corresponds with needed graft for augmentation or with the removal of septum that is interfering with breathing. K, An illustration of the extent of maximum septum (bone and cartilage) that may be removed to improve the airway. This includes much of the quadrangular cartilage and bone (i.e., vomer and perpendicular plate of ethmoid). The removed quadrangular cartilage available graft is shown. The yellow-colored aspect of the removed quadrangular cartilage indicates the planned caudal strut graft. L, An illustration of the crafted cartilage (strut) graft sutured to the caudal aspect of the remaining septal cartilage. The LLCs are then sutured together and over the top of the strut graft. This type of suture has been called a medial crural fixation suture. The sutures are placed to fix one medial crus to the other, thereby unifying the medial crura beneath the domes and then above the strut graft. This combination of techniques allows for the preferred nasal tip projection, shape, and orientation. M, Intraoperative views of removed septal cartilage, which can be used as graft material to reconstruct the nose. The cartilage can be crafted as a caudal strut, spreader grafts, LLC augmentation grafts, or tip onlay grafts. N, Nasal osteotomies are completed by first identifying the piriform rim intranasally with a speculum; the speculum blades straddle the bony rim. An incision is completed through the nasal mucosa on the side of the anterior maxilla to expose the piriform rim. The speculum is removed, and a Joseph elevator is inserted. Subperiosteal tunneling in the location of the proposed osteotomy is carried out. A curved and guarded osteotome is introduced through the intranasal incision, and the osteotomy is completed. The osteotomy is performed through the pyriform rim (maxilla), lateral to the nasomaxillary suture, and then up toward the nasofrontal suture on each side. The nasal bones are then in-fractured with finger pressure and positioned as desired.
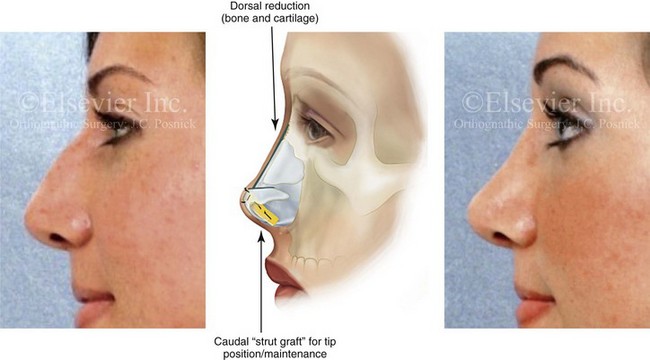
Figure 38-7 Profile views of the nose highlighting a young woman before and after rhinoplasty with the use of the techniques described in the legend for Figs. 38-5 and 38-6. An illustration highlights the combination of dorsal reduction (bone and cartilage) and nasal tip alteration (i.e., caudal strut cartilage grafting and lower lateral cartilage reshaping) typically carried out to achieve the objectives.

Figure 38-8 A woman in her 20s underwent a septorhinoplasty procedure as described previously. She is shown at 1 week and 4 weeks after surgery. At her 1-week visit, the custom-formed Aquaplast splint and skin sutures were removed.
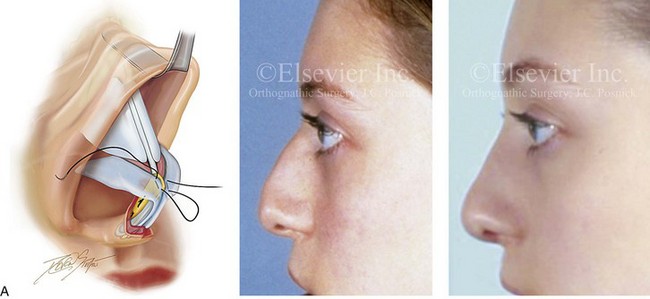
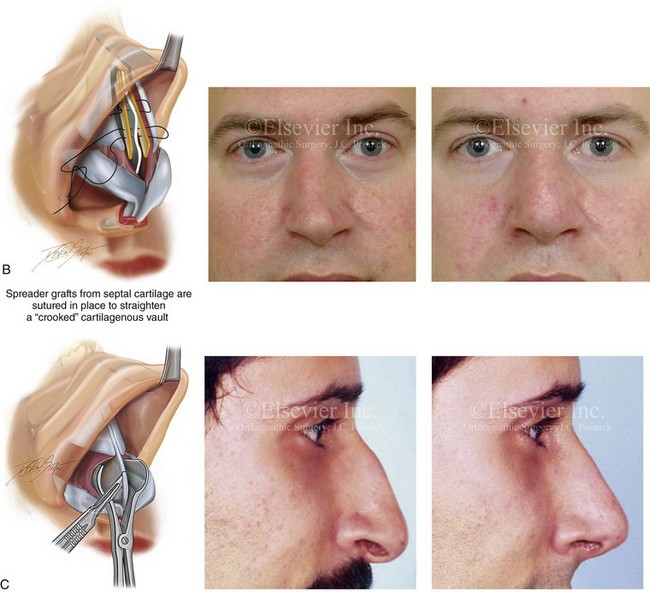
Figure 38-9 Three frequent maneuvers that are used to alter the cartilaginous vault and nasal tip are highlighted. For each of these three techniques, an illustration and a patient example are shown. Other rhinoplasty maneuvers were also simultaneously carried out on each patient. A, A frequent surgical technique to improve the position of the nasal tip is the harvesting of the septal cartilage, which is then crafted as a caudal strut. The caudal strut is sutured to the native septum and vectored to improve tip position and for maintenance. The lower lateral cartilages are then sutured together and over the top of the graft. B, Spreader grafts may be crafted from harvested septal cartilage. They are placed on each side of the dorsal aspect of the quadrangular cartilage and sutured together. Spreader grafts can be helpful to open the internal nasal valves and to straighten a crooked cartilaginous vault. C, Altering the caudal aspect of the quadrangular cartilage to achieve improved aesthetics in the columella region is often a necessary aspect of rhinoplasty. When there is excessive “columella show” seen in profile, the excision of the redundant caudal septal cartilage will be helpful. A patient example and an illustration are shown. In other circumstances, when there is inadequate “columella show” (i.e., retracted columella), augmenting the caudal aspect of the septum with a cartilage graft will be a useful approach (see Chapter 29).
• Complete the orotracheal (RAE) intubation, and tape the tube to the skin of the chin.
• Apply the ophthalmic ointment and place the corneal shields for eye protection.
• If the patient has long hair, tie it in a ponytail.
• Use Betadine solution (do not use soap, alcohol, Hibiclens and so on) to prepare the scalp, forehead, external ears, face, and neck.
• Complete draping and leave the forehead, external ears, face, and neck exposed in the operative field.
Local Anesthesia
• Inject Xylocaine (1% with 1 : 100,000 epinephrine) within the soft-tissue envelope of nose as usual for rhinoplasty.
• Inject Xylocaine (1% with 1 : 100,000 epinephrine) on each side of the septum, deep to the mucosa and superficial to the cartilage.
• Place either cocaine-soaked (5 mL of 4% solution) or Afrin-soaked pledgets in each nostril cavity.
Skin Incisions and Flap Elevation
• Incise the columella skin and the intranasal rims with a knife (#15 blade).
• Elevate the nasal soft-tissue envelope with Stevens scissors as required for an open rhinoplasty procedure.
• Elevate the overlying cutaneous soft-tissue envelope up the columella, superficial to the LLC and ULC, subperiosteal over the nasal bones (with a Joseph elevator) to the radix, and lateral toward the maxillary process on each side.
• Clean the subcutaneous tissue off of the superficial surface of each LLC with the use of Stevens scissors.
Lower Lateral Cartilage Modification
• The LLCs are separated from their midline soft-tissue connections with the use of Stevens scissors. Dissection continues down to the caudal aspect of the septum.
• The LLCs are marked with a caliper and trimmed of cephalic excess. In general, at least 6 mm of caudal LLC is retained. The redundant cephalic portions are incised with a knife (no. 15 blade) and removed with Stevens scissors.
Exposure and Resection of Portions of Septum
• Identify the anterior aspect of the caudal septal cartilage. (Dissection to the septum has already been completed with Stevens scissors.) A knife (no. 15 blade) is used to remove the final layer of perichondrium from the caudal edge of the septal cartilage before dissection. Next, use a sharp Cottle elevator to achieve submucosal exposure on each side of the septal cartilage. Extend the submucosal dissection inferiorly to the maxillary ridge and posterior to the vomer. Continue the subperiosteal dissection as required for the exposure and resection of the deviated bony septum (i.e., to the vomer and the perpendicular plate of the ethmoid).
• If the caudal aspect of the quadrangular cartilage requires reduction (i.e., to limit columella show), it is sharply incised with a knife (no. 15 blade), and the redundant portion is removed under direct visualization.
• Submucosal resection of the cartilaginous septum is initiated with the use of a knife (no. 15 blade) to control the caudal and dorsal aspects of the excision. The knife incisions are located to maintain approximately 10 mm of caudal and 10 mm of dorsal septal cartilage support for the nose. This is followed by the insertion of a swivel knife.
• The swivel knife is used to excise the deviated, buckled, or thickened septal cartilage (i.e., submucosal resection) and to harvest a graft, as indicated.
• A rongeur (either a double action or a Takahashi) is used to remove any buckled, deviated, or thickened portions of the vomer and the perpendicular plate of the ethmoid that are obstructing nasal airflow (i.e., submucosal resection).
Completion of Nasal Osteotomies
• A short nasal speculum is inserted intranasally with one forceps blade placed on either side of the pyriform rim.
• An incision is made with a knife with a no. 15 blade piercing the nasal mucosa down to the bone along the piriform rim of the maxilla.
• A Joseph elevator is used to dissect (tunnel) subperiosteally up toward the nasofrontal suture where the osteotomy is to be completed.
• A curved, guarded osteotome is inserted through the intranasal incision that saddles the pyriform rim. A mallet is used to drive the osteotome and to complete the osteotomy.
• The same procedure is completed on the other side.
• The nasal bones are in-fractured, disimpacted for adequate mobility, and then reoriented in accordance with aesthetic preference.
Reconstruction of Nasal Tip
• Craft the required grafts (e.g., caudal strut, LLC grafts, spreader grafts, tip graft) with a knife (no. 15 blade) from the full piece of harvested septal cartilage
• If a caudal strut graft is required, it is crafted and then positioned near (abutted to) the caudal aspect of septal cartilage to achieve improved nasal tip position. It is held in the preferred location with pinching forceps or a needle and then sutured to the side of the septal cartilage with the use of interrupted stitches (5-0 Vicryl).
• The LLCs, having been trimmed of cephalic excess, are sutured together and then over the caudal strut graft to form the most superficial aspect of the nasal tip (5-0 Vicryl). This type of suture has been called a medial crural fixation suture; it is used to fix one medial crus to the other, thereby unifying the medial crura beneath the domes and then above the caudal strut graft.
• The soft-tissue envelope is redraped and the nose is inspected to confirm adequate dorsal reduction, proper tip projection and position, satisfactory columella show, and straightness of the nose. Further refinements are made, if needed. (They usually are!)
Wound Closure
• After the completion of the septorhinoplasty procedure, closure of the wound is accomplished.
• To approximate the columella skin (stair-step incision), a single buried dermal suture is placed (5-0 Vicryl).
• The columella skin closure is with interrupted suture ties (6-0 nylon).
• The intranasal rim incisions are closed with interrupted ties (5-0 chromic).
Placement of Dressing
• Routine dressing is placed as they are after a septorhinoplasty procedure.
• Flexible splints (Reuter) are generally placed (one on each side of the septum) and secured together with single suture tie (3-0 nylon).
• Antibiotic ointment (Bactroban) is generally injected into each nostril cavity.
• When nasal osteotomies are carried out, nasal packing is helpful to maintain the preferred nasal bone position. Packing (folded Telfa) is generally inserted equally into each nostril cavity.
• Tape is placed over the dorsum of the nose (Steri-Strips) as it is after rhinoplasty.
• A custom splint (Aquaplast) is molded over the dorsum of the nose as it is after rhinoplasty.
Images of a series of individuals are shown to demonstrate the spectrum of presentations and the typical results achieved with the use of the techniques just described (Figs. 38-10 through 38-18 ).

Figure 38-10 A teenage girl arrived with her parents and requested a rhinoplasty to remove the “hump” that was seen in profile. She also has a lifelong history of difficulty breathing through the nose. She underwent an open rhinoplasty that included nasal osteotomies (in-fracture); dorsal reduction (bone and cartilage); nasal tip maneuvers (lower lateral cartilage modification and septal cartilage caudal strut grafting); septoplasty; and inferior turbinate reduction. A, Frontal views before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views be/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


