Dentofacial Disharmonies in Adults
Reconstruction and Rejuvenation
• Special Medical Considerations
• Functional Assessment of Head and Neck Structures
• Temporomandibular Disorders: Effects of Orthodontics and Orthognathic Surgery
• Special Wound Healing Risk Factors
• Comprehensive Dental Rehabilitation
• Unique Orthodontic Treatment Considerations
• Previous Suboptimal Facial Surgery
• Facial Aging and Rejuvenation
The techniques for the correction of a dentofacial deformity are basically the same for the middle-aged adult as they are for the teenager and the young adult. To achieve a favorable result in the adult orthognathic patient, it is essential to recognize age-related treatment pitfalls such as medical risk factors; progressive upper airway dysfunction; dental rehabilitation needs, including periodontal and restorative aspects; the effects of facial soft-tissue aging; and the often prolonged physiologic and psychosocial responses to surgery (Figs. 25-1 through 25-11).

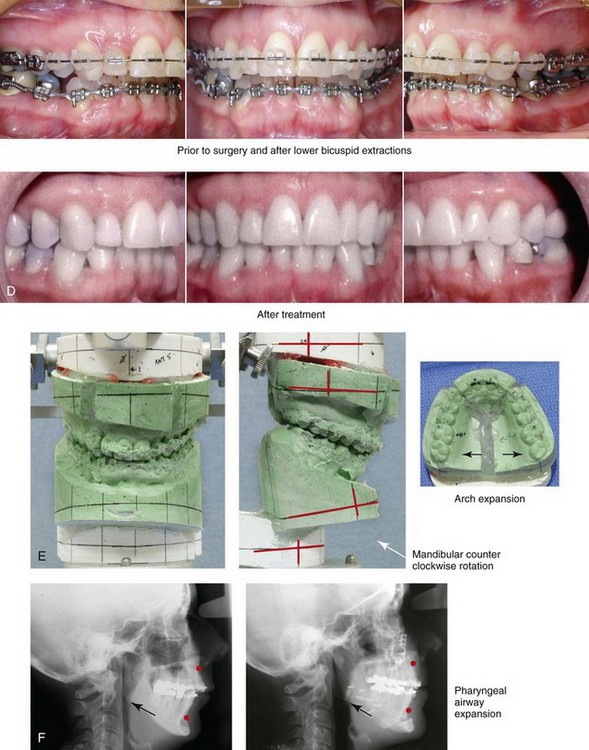
Figure 25-1 A woman in her mid 50s was referred by her general dentist to an orthodontist for the management of a longstanding Class II excess overjet malocclusion that had gradually resulted in the deterioration of the posterior dentition. The orthodontist recognized that the malocclusion resulted from a retrusive mandible and a constricted maxilla. With referral for surgical evaluation, a head and neck examination was completed. In addition to a developmental jaw deformity that involved both the maxilla and mandible, chronic obstructive nasal breathing and a sleep history consistent with obstructive sleep apnea was clarified. Suboptimal facial aging with a desire for an improved neck–chin angle was also discussed. An attended polysomnogram confirmed moderate obstructive sleep apnea. The patient agreed to proceed with orthodontics, including lower first bicuspid extractions to relieve dental compensation in combination with jaw and intranasal surgery. The objectives were to improve the airway, to enhance facial aesthetics, and to achieve improved long-term dental health. The patient’s surgical procedures included maxillary Le Fort I osteotomy in segments (horizontal advancement, counterclockwise rotation, arch expansion, and the correction of the curve of Spee); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement); an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication); and septoplasty and inferior turbinate reduction. A, Facial views before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views before and after reconstruction. Note the improved A-point to B-point relationship. D, Occlusal views with orthodontics in progress (lower bicuspid extractions) and after treatment. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after surgery. Note the improved posterior airway space documented.

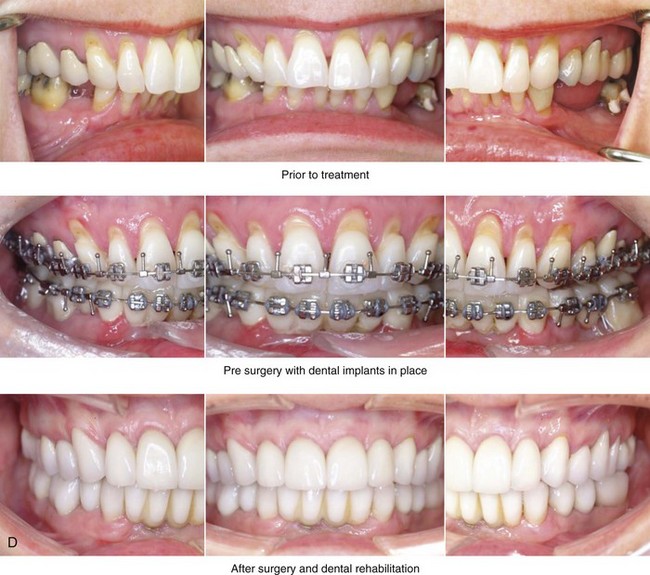
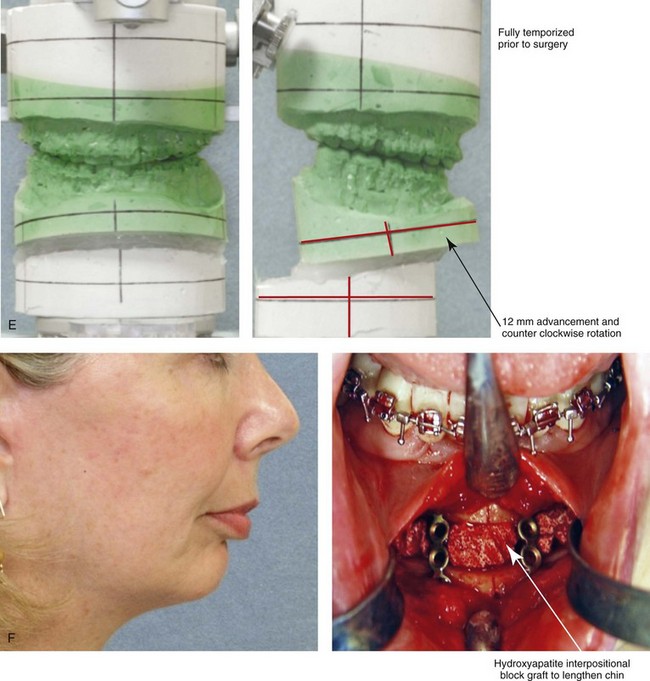
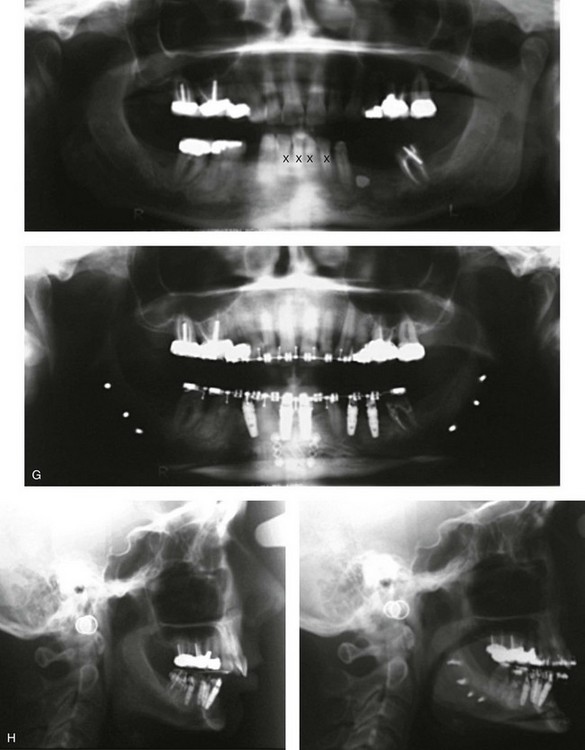
Figure 25-2 A woman in her early 50s was referred by a prosthodontist for surgical evaluation. There had been a gradual deterioration of her dentition that was at least partially a result of the longstanding Class II excess overjet deep-bite malocclusion. The head and neck evaluation confirmed a retrusive mandible, which also resulted in retroglossal airway obstruction. A desire for improved profile aesthetics was also discussed. A comprehensive approach to dental rehabilitation, improvement of the upper airway, and facial rejuvenation/reconstruction was chosen. Coordinated endodontic, orthodontic, periodontic, prosthodontic, and surgical care was required. Periodontal treatment, extractions, dental implant placement, restorative temporization, and orthodontic alignment were carried out. This was followed by surgery that included bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical lengthening) with interpositional grafting; and an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication). This was followed by crown lengthening and then by the final dental restorations. A, Frontal views before and after reconstruction/dental rehabilitation. B, Facial oblique views before and after reconstruction/dental rehabilitation. C, Profile views before and after reconstruction/dental rehabilitation. D, Occlusal views at presentation, before surgery, and after reconstruction/dental rehabilitation. E, Articulated dental casts that indicate analytic model planning. F, Profile view of the chin. The intraoperative view of the chin osteotomy indicates vertical lengthening with hydroxyapatite interpositional bloc graft. G, Panorex radiographs before and after lower jaw and chin surgery with the placement of dental implants. H, Lateral cephalometric radiographs before and after reconstruction.


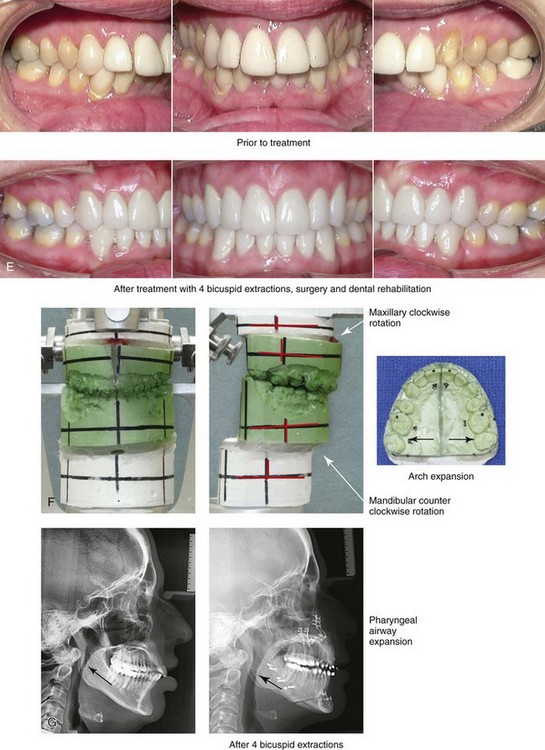
Figure 25-3 A woman in her late 40s with a long face growth pattern suffered deterioration of the dentition. Her periodontal risk factors included inadequate attached gingiva; dental root crowding within limited alveolar bone support, nasal airway obstruction with forced mouth breathing, and lip incompetence with drying of the exposed gingiva. An attended polysomnogram confirmed obstructive sleep apnea. Unfavorable soft-tissue envelope distortions and premature facial aging were also present. She agreed to a comprehensive surgical and dental rehabilitative approach. Periodontal treatment was followed by restorative temporization and orthodontic alignment, including four first bicuspid extractions. This was followed by surgery that included maxillary Le Fort I osteotomy in segments (vertical shortening, horizontal advancement, transverse widening, and limited clockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and limited counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. Note the pretreatment tendency for the patient to hyperextend her neck to achieve an improved airway. After successful surgery and with improved daytime breathing, her neck rests in a natural (neutral) position. E, Occlusal views before treatment and after reconstruction/dental rehabilitation. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment. Note the improved posterior airway space.


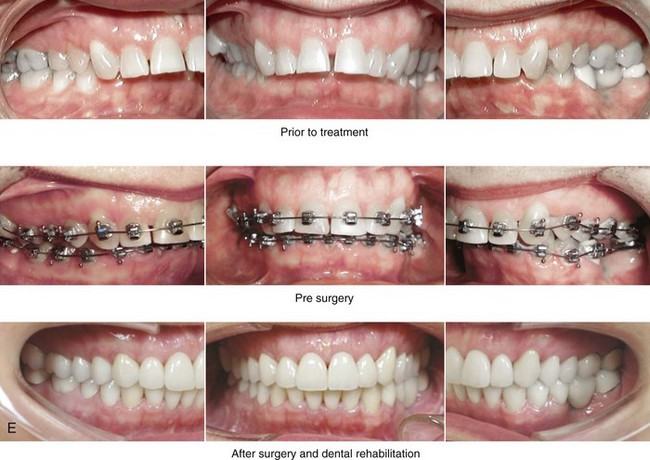
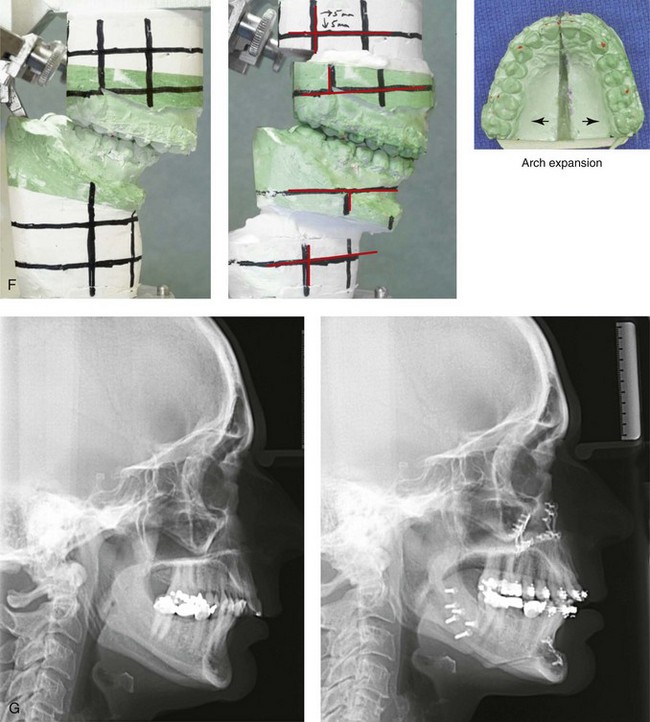
Figure 25-4 A woman in her mid 50s was experiencing significant dental deterioration as a result of occlusal trauma. An orthodontic consultation followed by surgical evaluation was carried out. The longstanding developmental jaw deformity was characterized by a short face growth pattern in combination with maxillary transverse constriction. There was a Class II deep-bite excess overjet malocclusion. The patient’s head and neck evaluation confirmed a lifelong history of obstructed nasal breathing, restless sleeping at night, and a degree of daytime fatigue that was consistent with obstructive sleep apnea. Unfavorable facial aging that is typical of maxillomandibular deficiency was recognized. A comprehensive surgical and dental rehabilitative approach was selected. The objectives included dental rehabilitation, the enhancement of facial aesthetics, and an improved airway. The patient’s procedures included maxillary Le Fort I osteotomy in segments (horizontal advancement, vertical lengthening, and arch expansion); bilateral sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (vertical lengthening and horizontal advancement); an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after reconstruction/dental rehabilitation. B, Frontal views with smile before and after reconstruction/dental rehabilitation. C, Oblique facial views before and after reconstruction/dental rehabilitation. D, Profile views before and after reconstruction/dental rehabilitation. E, Occlusal views before treatment, with orthodontics in progress, and after reconstruction/dental rehabilitation. F, Articulated dental casts indicate analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction.


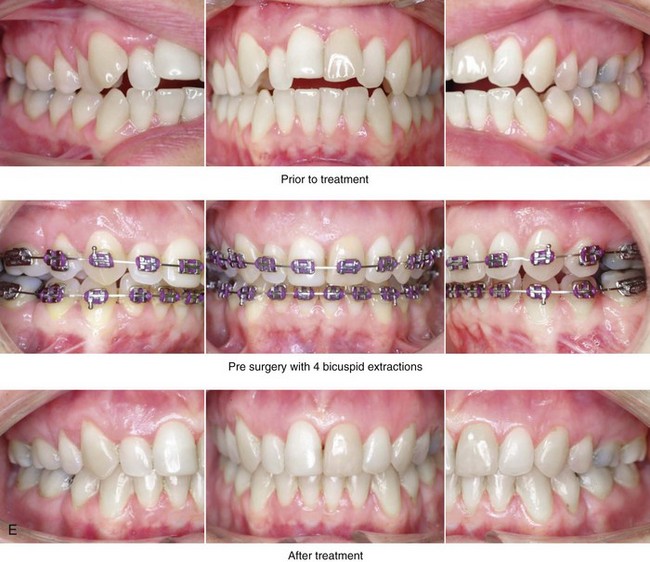
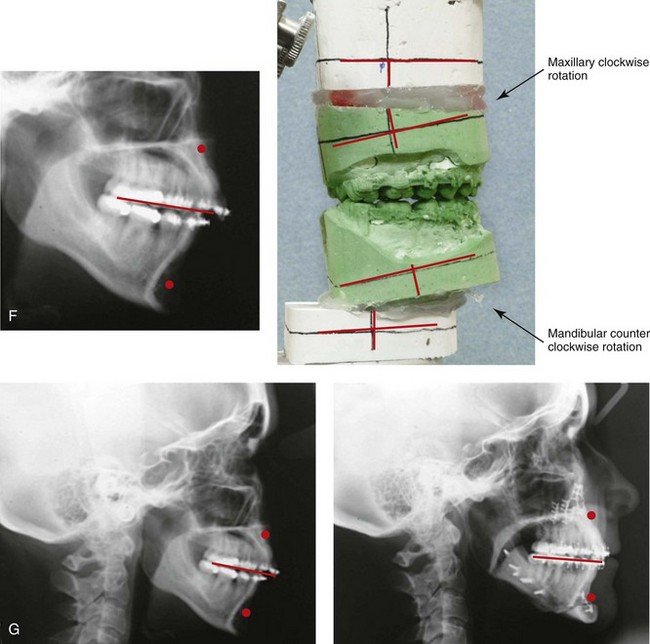
Figure 25-5 A woman in her early 40s wished to correct her malocclusion and improve her smile. She was referred to an orthodontist who then requested surgical evaluation. She was found to have a long face growth pattern and a lifelong history of obstructed nasal breathing. There was dental crowding in each arch, mild gingival recession associated with the posterior dentition, and a Class II anterior open-bite malocclusion. The patient was aware of unfavorable facial aesthetics, which included a retrusive chin and an obtuse neck–chin angle. She agreed to a comprehensive surgical and dental rehabilitative approach. She underwent extraction of four bicuspids, orthodontic alignment, and then surgery. The patient’s procedures included Le Fort I osteotomy (vertical intrusion, horizontal advancement, and counterclockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); an anterior approach to the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before treatment, with extractions and orthodontic decompensation complete, and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


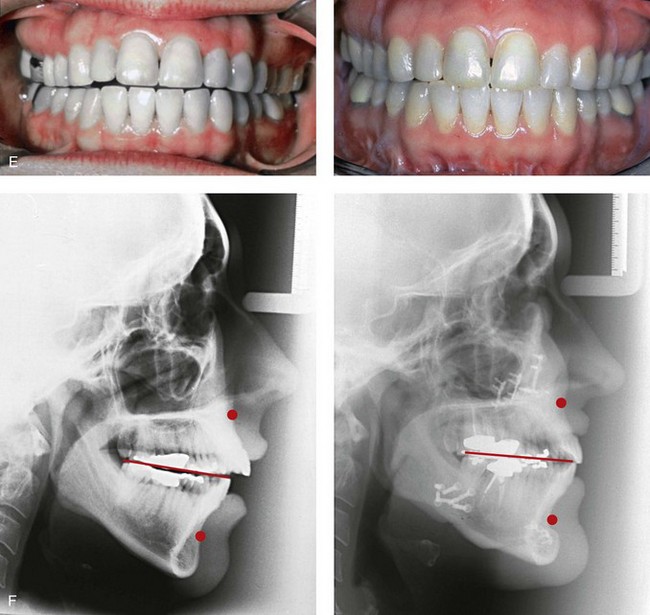
Figure 25-6 A woman in her early 50s arrived for surgical evaluation and requested facial rejuvenation. Her head and neck examination confirmed a lifelong history of obstructed nasal breathing and a long face growth pattern with gummy smile and lip incompetence. Unfavorable soft-tissue envelope facial aging added to the original dentofacial deformity. Early during her life, posterior occlusal equilibration was carried out to close down the anterior open bite; this resulted in dental deterioration that required crowns in the posterior dentition and the need for root canal therapy in many of the teeth. At this time, the patient agreed to a combined surgical and dental rehabilitation approach. After orthodontic preparation, the patient’s surgical procedures included maxillary Le Fort I osteotomy (vertical intrusion, horizontal advancement, and counterclockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal recontouring. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before and after treatment. F, Lateral cephalometric radiographs before and after surgery.


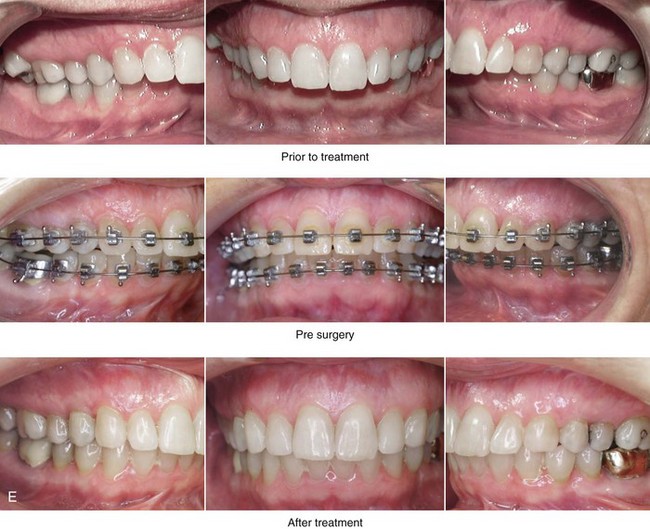
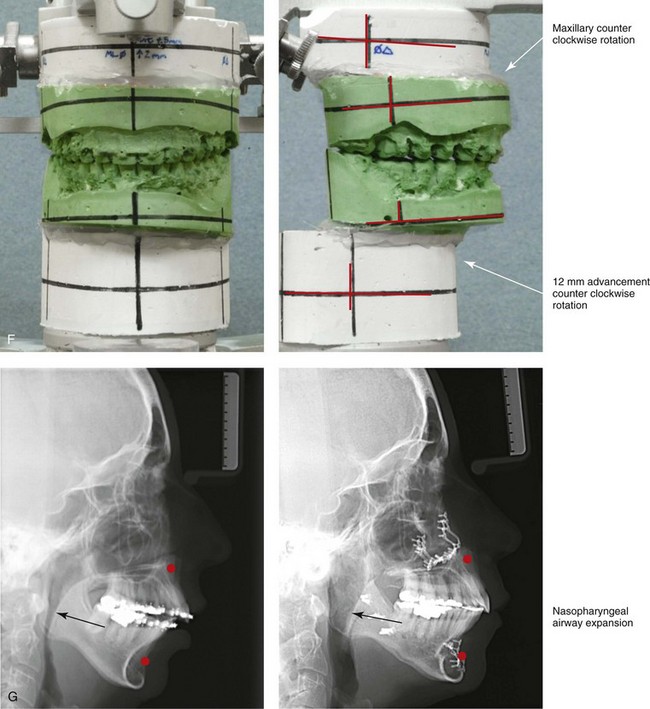
Figure 25-7 A woman in her mid 50s was seen by a prosthodontist for the management of a deteriorating posterior dentition. She was confirmed to have secondary dental trauma as a result of a longstanding malocclusion. She was referred to an orthodontist and then for surgical assessment. Her head and neck evaluation confirmed a short face growth pattern with a Class II excess overjet deep-bite constricted maxillary arch malocclusion. There was a lifelong history of obstructed nasal breathing and the suggestion of obstructive sleep apnea, which was confirmed with an attended polysomnogram. Facial aesthetic concerns included the downturned corners of the mouth, the deep perioral creases, the early jowl formation, the weak profile, the obtuse neck–chin angle, and the loose skin of the neck. The patient agreed to a comprehensive surgical and dental rehabilitative approach. Periodontal evaluation, initial restorations, and orthodontic decompensation preceded surgery. The patient’s surgical procedures included maxillary Le Fort I osteotomy (horizontal advancement, counterclockwise rotation, and vertical adjustment); bilateral sagittal split osteotomies of the mandible (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement); an anterior approach to the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication); and septoplasty, inferior turbinate reduction, and nasal recontouring. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before treatment, with orthodontics in progress, and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment. Note the improved posterior airway space.



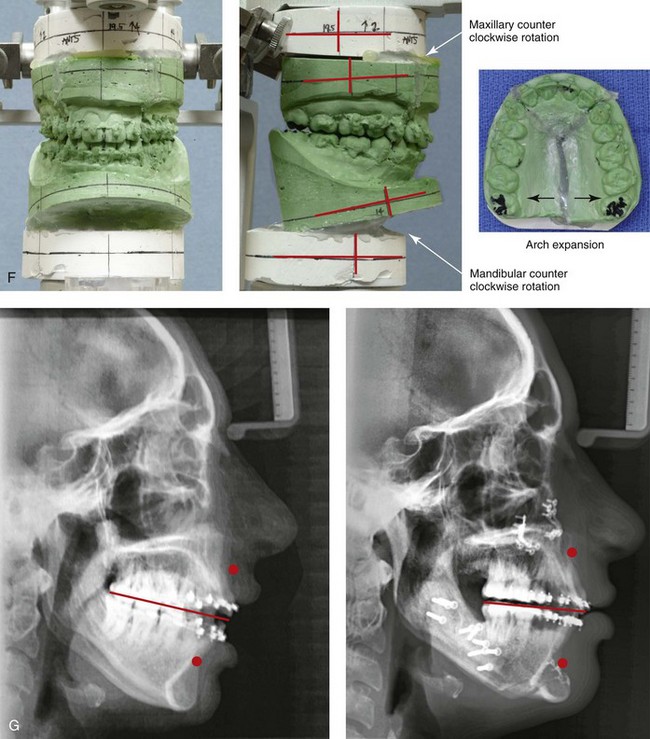
Figure 25-8 A woman in her mid 30s was referred by an orthodontist for surgical evaluation. She had a lifelong history of obstructed nasal breathing and a long face growth pattern. Throughout her middle childhood and teenage years, she had undergone attempted growth modification followed by orthodontic camouflage that included four bicuspid extractions in an effort to neutralize the occlusion. This resulted in periodontal deterioration and dental relapse with residual malocclusion. She now agreed to a comprehensive surgical and dental rehabilitative approach. Periodontal treatment was followed by orthodontic decompensation. The patient’s surgery included maxillary Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, arch expansion, and the correction of the curve of Spee); bilateral sagittal split ramus osteotomies in segments (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal recontouring. A, Frontal views in repose before and after reconstruction/dental rehabilitation. B, Frontal views with smile before and after reconstruction/dental rehabilitation. C, Oblique facial views before and after reconstruction/dental rehabilitation. D, Profile views before and after reconstruction/dental rehabilitation. E, Occlusal views before retreatment, with orthodontics in progress, and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.


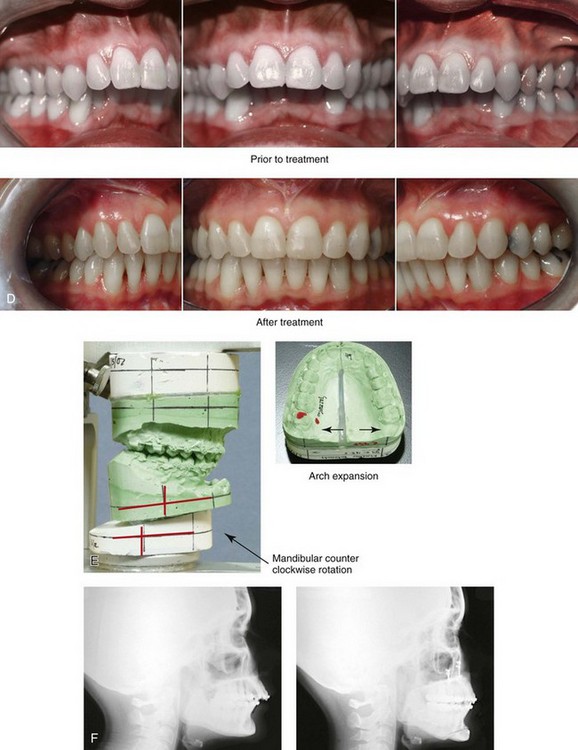
Figure 25-9 A woman in her mid 40s requested the correction of her malocclusion and an improved smile. She was referred by a restorative dentist to an orthodontist and then for surgical evaluation. The developmental jaw deformity was characterized by mandibular deficiency in combination with maxillary arch width constriction. A lifelong history of obstructed nasal breathing with a desire for an improved airway was also confirmed. A combined orthodontic and surgical approach was chosen. After orthodontic decompensation, the patient’s surgery included maxillary Le Fort I osteotomy in segments (transverse expansion); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after reconstruction. B, Facial views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Occlusal views before treatment and after reconstruction. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction.

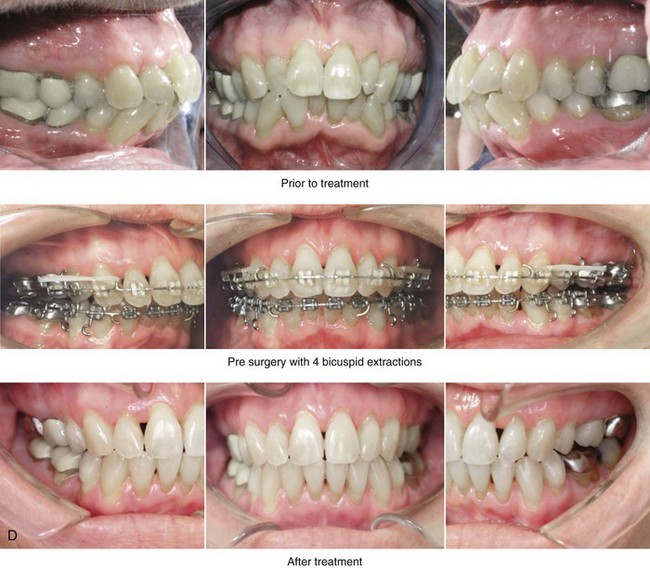
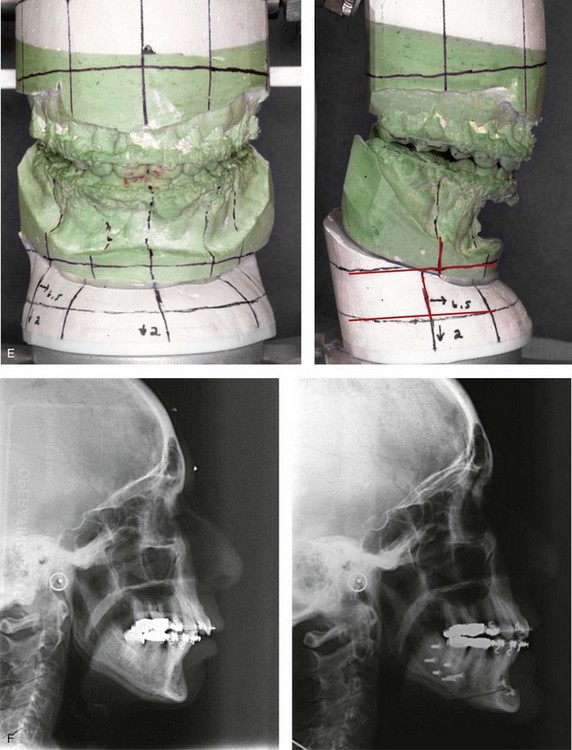
Figure 25-10 A 70-year-old woman arrived for surgical evaluation. She desired a stronger chin, less “loose” neck skin, and an improved smile. She initially requested a face lift and a chin implant. She was found to have a retrusive mandible and dental deterioration made worse by dental crowding and a deep-bite negative overjet malocclusion. She underwent orthodontics that included four bicuspid extractions and then surgery that included sagittal split ramus osteotomies (horizontal advancement) and osseous genioplasty (horizontal advancement). A, Frontal views with smile before and after treatment. B, Oblique facial views before and after treatment. C, Profile views before and after treatment. D, Occlusal views before treatment, with orthodontics in progress (including four bicuspid extractions), and after treatment. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after surgery.

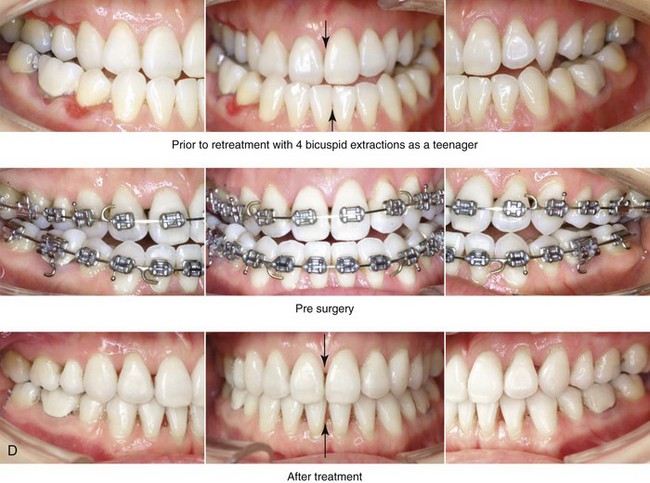
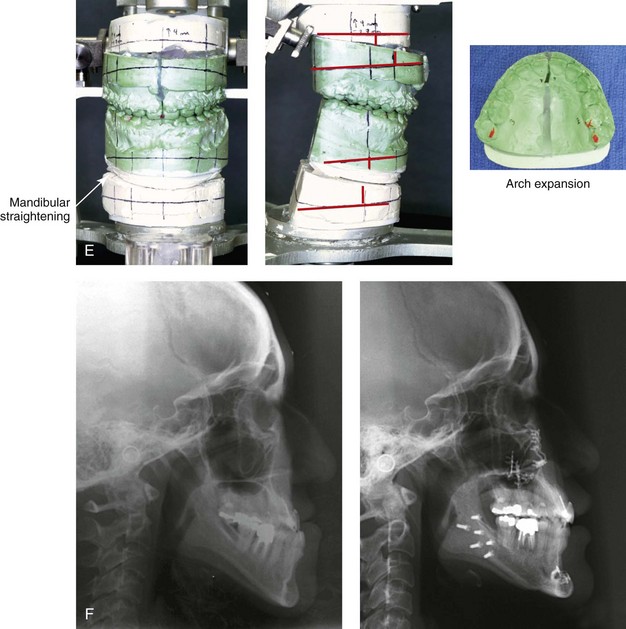
Figure 25-11 An Asian woman in her mid 30s had a developmental jaw deformity that was characterized by maxillary deficiency and relative mandibular excess. In the childhood years, she had been treated with growth modification followed by four bicuspid extractions and orthodontic camouflage mechanics. Periodontal deterioration resulted, and malocclusion remained. She also had a lifelong history of obstructed nasal breathing. She now agreed to a comprehensive surgical and dental rehabilitative approach. Periodontal treatment was followed by orthodontic decompensation. The patient’s surgery included maxillary Le Fort I osteotomy in segments (horizontal advancement, vertical intrusion, counterclockwise rotation and transverse widening); bilateral sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views with smile before and after treatment. B, Oblique facial views before and after treatment. C, Profile views before and after treatment. D, Occlusal views before retreatment, with orthodontics in progress, and after reconstruction/dental rehabilitation. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after treatment.
Special Medical Considerations
For the adult who is more than 40 years old and who is considering orthognathic surgery, additional medical risk factors may include cardiovascular disease; the effects of obesity; smoking history and pulmonary function; the potential for deep vein thrombosis or pulmonary embolus; the effects of bisphosphonate medication on wound healing; and occult malignancy. As with teenagers and young adults, taking a thorough history, performing a review of the medical records, and completing a physical examination are essential. To clarify areas of concern in these patients, there should be emphasis placed on the need for a thorough clearance examination by a primary care physician; evaluations by other medical specialists; (e.g., cardiologist, pulmonologist); the completion of an electrocardiogram, chest radiography, and laboratory tests (e.g., chemistries, hematology, thyroid tests, coagulation tests); and other special studies (e.g., stress test, echocardiogram, sleep study, pulmonary function tests). Obtaining a hemoglobin A1C level and a serum or urine cotinine level are useful checks to address long-term diabetes effects and smoking compliance, respectively. The adult with a dentofacial deformity and an elevated body mass index is at risk for obstructive sleep apnea (OSA) and therefore more vulnerable to intraoperative and postoperative complications (see Chapter 26).
Functional Assessment of Head and Neck Structures
The orthognathic surgeon should evaluate the baseline head and neck functions of their patients, which include speech, swallowing, chewing, breathing, hearing, vision, cognition, and psychosocial competence (see Chapters 7 and 8). The documentation of cervical spine and temporomandibular joint (TMJ) baseline function and of any limitations in neck or mandibular range of motion is also essential (see Chapter 9). Each of these aspects may be negatively affected by the presenting maxillofacial malformations and influenced favorably or unfavorably by the treatment being contemplated. Baseline chronic obstructive nasal breathing as a result of septal deviation, enlarged inferior turbinates, or a tight nasal aperture should not be ignored (see Chapter 10).103,104,106,107 In the adult, weight gain with adipose hypertrophy within the upper airway in combination with hypotonia of the pharyngeal muscles in the presence of an uncorrected dentofacial deformity is likely to result in OSA. A formal attended polysomnogram, a complete upper airway evaluation, and a consultation with a sleep specialist are frequently indicated (see Chapter 26).
Temporomandibular Disorders: Effects of Orthodontics and Orthognathic Surgery
It is estimated that an average of 32% of the population report at least one symptom of temporomandibular disorder (TMD) and that an average of 55% demonstrate at least one clinical sign of such a condition.117 TMDs include various symptoms and signs of the TMJs, the masticatory muscles, and the related structures. The symptoms and signs may include a spectrum of referred head and neck discomforts; joint noise (e.g., popping, clicking, crepitus); reduced or altered mandibular movements as a result of muscle spasm or disc displacement with or without reduction; condylar head erosion; and pain on direct palpation of either TMJ or of the masticatory muscles.
The effects of orthodontics and orthognathic surgery on TMJ function for each specific adult patient cannot be fully predicted. Many clinical studies report improvement in TMJ symptoms and signs in a majority of individuals after successful orthodontics and orthognathic surgery, although some patients will deteriorate after the procedures. The favorable TMJ effects of orthognathic surgery often observed in patients with preoperative TMD may be the result of the improved occlusion, the restoration of normal facial height and jaw projection, or the reduced emotional stress. Adults with longstanding TMD should be cautioned that their pretreatment findings may not respond to occlusal correction and jaw-straightening surgery. Baseline TMD problems in the patient with a dentofacial may primarily be masticatory muscle disorders (i.e., myofascial conditions) or, less commonly, the result of joint pathology (i.e., internal derangement). These two problems may coexist, and the distinction in some individuals may be difficult. It is unlikely that the correction of an existing dentofacial deformity will correct either internal joint problems or other non-muscular sources of pain. Myofascial pain develops when muscles are fatigued, because they then tend to go into spasm. Myofascial pain generally occurs after clenching or grinding the teeth for many hours each day, presumably as a response to stress. It is also true that some types of occlusal discrepancies predispose the individual who clenches or grinds his or her teeth to TMD. A compelling argument against malocclusion as the primary cause of TMD is the observation that TMD is not more prevalent among individuals with malocclusion as compared with those with a more normal occlusion. Interestingly, for those individuals with myofascial pain, the orthodontic mechanics required as part of the orthognathic correction are often helpful. This is because orthodontic treatment makes the teeth sensitive, which tends to limit grinding and clenching. Therefore, when the parafunctional (i.e. clenching, grinding) activity stops, the myofascial pain is often diminished. The changing occlusal relationships during the orthodontic phase of treatment may also contribute to a break in the cycle that contributed to the initial muscle fatigue and pain. The cycle of clenching and grinding is also broken during the healing phase that takes place just after orthognathic surgery. Unfortunately, it is also recognized that, at some point after successful orthodontics and orthognathic surgery, the individual with a long history of myofascial TMD symptoms may return to the clenching and grinding parafunctional habits. The use of an intra-occlusal splint in this situation will often be the best way to break the cycle and keep symptoms at bay. For all of these reasons, the individual’s rationale for the correction of the jaw deformity and the associated malocclusion should not be solely based on a desire for the permanent relief of TMJ symptoms and signs (see Chapters 7 and 9).
Special Wound Healing Risk Factors
Special wound healing risk factors may include previous radiation therapy, diabetes mellitus, smoking or other forms of nicotine use, and past or current bisphosphonate treatment for osteoporosis. Diabetes mellitus, high blood pressure, hyperlipidemia, and OSA are frequent comorbidities of obesity that may complicate wound healing. A significant incidence of postoperative infections among diabetic patients undergoing maxillary or mandibular osteotomies has been reported, despite adequately controlled glucose levels. The inhalation of nicotine via cigarette smoke affects pulmonary function as well as tissue oxygenation and the healing of the surgical wounds. Smoking (nicotine ingestion) has been shown to delay the chondrogenic phase of bone (osteotomy) healing, thereby negatively affecting the circulation of elevated flaps and their healing after wound closure. It is known that bisphosphonate treatment for osteoporosis affects osteoclastic activity and may negatively affect bone healing (see Chapter 16).
Comprehensive Dental Rehabilitation
Recognizing when a patient who is seeking orthognathic surgery has additional dental needs beyond standard orthodontics is essential to the achievement of a favorable outcome (see Figs. 25-1 through 25-11). The need for periodontal evaluation and treatment as well as the need for complex dental restorative work should be considered for every adult patient before the initiation of a coordinated orthodontic and jaw surgical approach. This is especially true for the adult who has suffered dental and periodontal sequelae from a longstanding uncorrected dentofacial deformity and who may have undergone camouflage treatment in an attempt to neutralize the occlusion (e.g., orthodontics, occlusal equilibration, r/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


