37 Adhesive-retained, Fiber-reinforced Composite Posts
Numerous options of adhesive build-ups are available today, which dispense with the need for root canal posts and which are preferable because they are less invasive (Creugers et al., 2005). Nevertheless, in clinical situations where there is insufficient coronal hard tissue to support the adhesive build-up, root canal pins/posts still provide the only long-term possibility of retention and stability of the build-up.
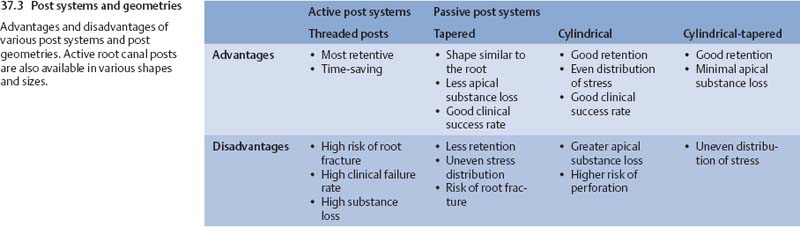
From the vast array of commercially available post systems and shapes, the conical, passive posts have received an increased level of attention because of the similarity between their shape and the root’s shape (Morgano and Brackett, 1999).
It has been shown that in combination with appropriate adhesive systems, the retention of conical posts is significantly improved and passive fitting avoids active loading of the canal walls (Boschian Pest et al., 2006; Dietschi et al., 2006).
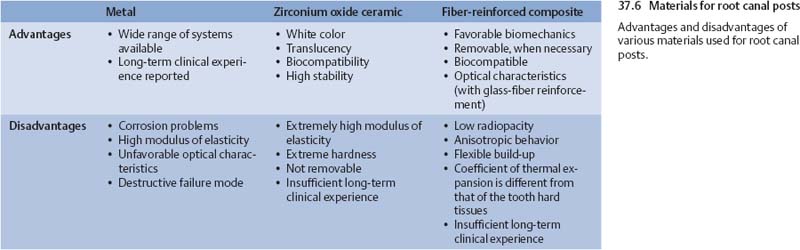
37.1 Range of available materials
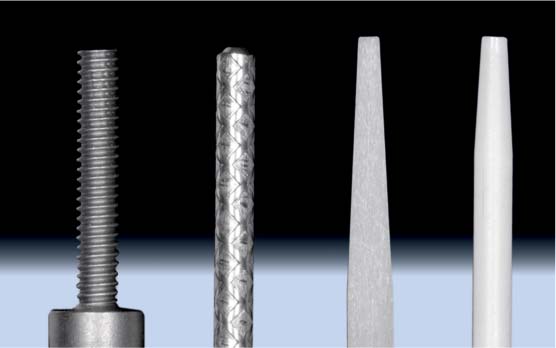
Various systems and materials for root canal posts (from left to right): active, threaded cylindrical titanium post; passive titanium cylindrical post with surface roughening, passive glass-fiber-reinforced tapered post made of composite resin, with a smooth surface; and a cylindrical-tapered post of zirconium oxide ceramic, with a smooth surface.
37.2 Light transmission
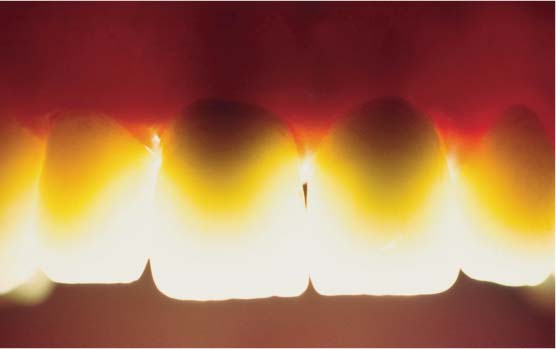
Transmitted light image of full ceramic crowns, some of which were fixed to metal endodontic post buildups (central incisors). The metal posts are seen to cause marked inhibition of light transmission and shadows in the area of the crowns and the surrounding soft tissues.
For root canal posts based on reinforced composite materials, the basic material is an epoxy resin reinforced by carbon or glass fibers. These materials demonstrate mechanical characteristics similar to dentin and can in certain circumstances be relatively easily removed (Lassila, 2004). In vitro investigations have indicated that use of these posts is associated with a less destructive failure mode in comparison to posts made from other materials (Fokkinga, 2004). If these laboratory observations were corroborated by clinical studies, the fact that a fiber-reinforced composite post is relatively easy to remove would allow uncomplicated retreatment of a tooth after post fracture.
So far, posts made of fiber-reinforced composite material exhibit low radiopacity. In addition, the quality of the post can vary considerably depending on the manufacturer (Grandini, 2005).
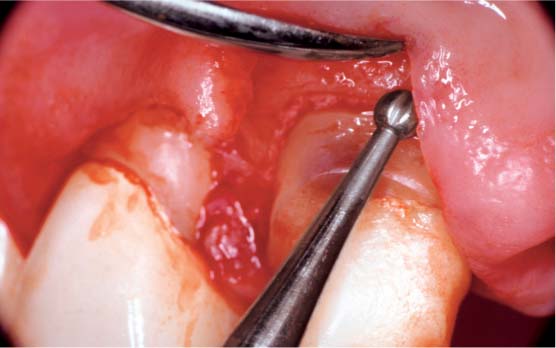
37.4 Removal of a glass fiber post
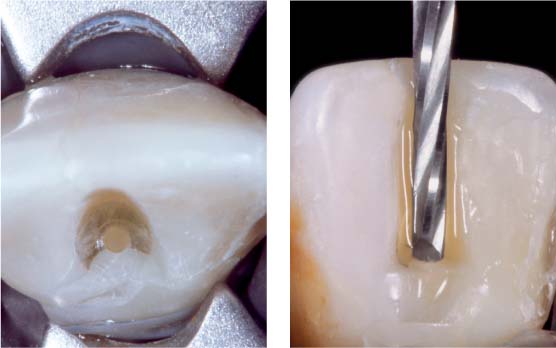
Left: During the removal of a glass fiber post (here: experimental ex vivo situation), it is advantageous to first create a plateau to stabilize the small round bur used to create a point of access in the middle of the fractured post.
Right: For the actual post removal, special carbon-steel burs with a cutting tip are used intermittently at a low speed (800–2000 rpm) with water cooling.
37.5 Radiopacity
Periapical radiograph of maxillary second molar following instrumentation and temporary insertion of glass-fiber-reinforced composite post for length determination. The post is less radiopaque than the remaining gutta percha portion of the root canal filling, which is left in place for apical sealing.
Use of a highly radiopaque adhesive material for final placement of the post can significantly enhance radiographic visibility.
Creating Post Space and Preparation
In general, following the primary treatment (excavation, endodontic therapy), it is prudent to carry out a defect-based preparation of the tooth so that the final restoration can be designed specifically for each tooth. This procedure provides a better estimate of the vertical extent and the thickness of the remaining tooth structure as well as the biological width.
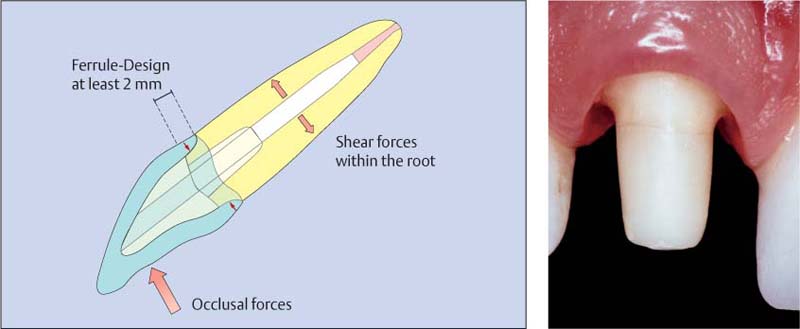
It is generally accepted that the fracture resistance of endodontically treated teeth is significantly affected by the amount of the remaining coronal tooth structure (Creugers et al., 2005; Pereira et al., 2006). The stability of teeth with post-and-core restorations is increased if a dentin collar at least 2-mm wide is prepared apical to the build-up, which is enclosed by the final restoration circumferentially. This preparation, also referred to as the “ferrule” preparation, has a stabilizing effect on the root, and enhances the long-term clinical success of the final restoration (Torbjorner and Fransson, 2004; Pereira et al., 2006).
If the anatomic considerations do not permit this approach, the requirements can be fulfilled by periodontal surgical crown lengthening or orthodontic extrusion, if the root length is sufficient.
Even though endodontically treated teeth have a good clinical long-term prognosis, the possible negative consequences of dental implants should be taken into consideration before such methods involving bone reduction are used in esthetic areas of the mouth (Holm-Pedersen et al., 2007).
37.7 Biologic width
Surgical crown lengthening procedure to create adequate biologic width on a tooth that had been restored using a metal-free post build-up. Without this surgical procedure it would not have been possible to achieve sufficient circumferential marginal adaptation of the subsequent restoration. However, when periodontal procedures that involve removal of bone are undertaken, the clinician must take into consideration the fact that future insertion of a dental implant in this region may be necessary.
37.8 Ferrule effect (as described by Morgano a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses