chapter 34 Management of Emergencies
Despite efforts at prevention, complications and adverse drug reactions (ADRs) will arise during and after the administration of drugs for the management of pain or anxiety. In the office that has prepared for these situations, there is a greater likelihood of a successful outcome than in the unprepared or ill-prepared office. Many states, provinces, and specialty groups require that the dental office team be capable of correctly identifying and managing specific ADRs associated with parenteral sedation and general anesthesia.1,2 These emergencies are reviewed in this chapter.
Pallasch3 has proposed the following classification of ADRs:
Overdose reaction (also known as “toxic reaction”) refers to those signs and symptoms manifested as a result of an absolute or relative overadministration of a drug producing elevated blood or plasma levels of that drug in specific organs (termed target organs) of the body. For central nervous system (CNS)–depressant drugs, an overdose occurs when the blood level of the drug becomes overly high in the cerebral circulation.4 Clinical manifestations of an overdose are related directly to the normal pharmacologic actions of the agent. For example, in therapeutic doses, barbiturates produce a mild depression of the CNS, which results in sedation or hypnosis (desirable effects). Barbiturate overdosage produces a more profound depression of the CNS, with respiratory or cardiovascular depression and a possible loss of consciousness.
Allergy is a hypersensitive state acquired through exposure to a particular allergen, reexposure to which brings about a heightened capacity to react.5 Clinically, there are a variety of manifestations through which allergy expresses itself. These include drug fever, angioedema, urticaria, dermatitis, depression of blood-forming organs, photosensitivity, and anaphylaxis. Certain drugs are more likely than others to elicit allergic reactions, and allergic reaction is theoretically possible with any substance.
It is thought today that virtually all instances of idiosyncrasy have an underlying genetic mechanism.6 These genetic aberrations remain undetected until the individual receives a specific drug, such as succinylcholine, which then produces its bizarre (nonpharmacologic) clinical expression.
Two major forms of ADR, overdose and allergy, are reviewed in this chapter; in addition, other emergency situations are discussed. Successful demonstration of the ability to manage these situations is frequently a requirement of the permitting process for parenteral sedation and general anesthesia. These complications are listed in Box 34-1.
Box 34-1
Data from California State Board of Dental Examiners: Conscious sedation evaluation protocol, Sacramento, 2005; and American Association of Oral & Maxillofacial Surgeons: Office anesthesia evaluation manual, ed 6, Rosemont, Ill, 2006, The Association.
Emergency Situations Identified for Parenteral Sedation and General Anesthesia
OVERDOSE
The group of drugs most likely to produce an overdose is the barbiturates. Barbiturates represented the first major breakthrough in the pharmacologic management of anxiety, and because of this, adverse reactions, such as allergy, addiction, and overdose, were tolerated. In the 1960s, with the introduction of the benzodiazepines (drugs that do not possess the same potential for abuse and overdose), barbiturate use declined. Description of their use in dentistry has been dropped from this edition. Previous editions of SEDATION, a Guide to Patient Management contain complete description of their use.7
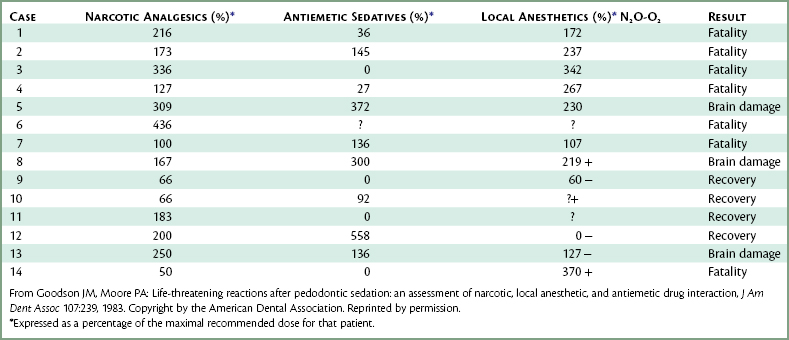
Although the barbiturates present the greatest potential for adverse reaction, the opioid analgesics are involved with the greatest number of clinically significant episodes of overdose and respiratory depression. This is simply because opioids are more widely used than the barbiturates. As discussed elsewhere (see Chapters 7, 10, and 35), the use of opioids is popular in pediatric sedation. Opioids are often administered intravenously in conjunction with antianxiety drugs to aid in sedation and pain control in the adult patient. Goodson and Moore reported on 14 pediatric dentistry cases in which the administration of opioids (and other drugs) led to seven deaths and three instances of brain damage.8 Several opioids were implicated in these reactions: alphaprodine (7), meperidine (6), and pentazocine (1).
Predisposing Factors and Prevention
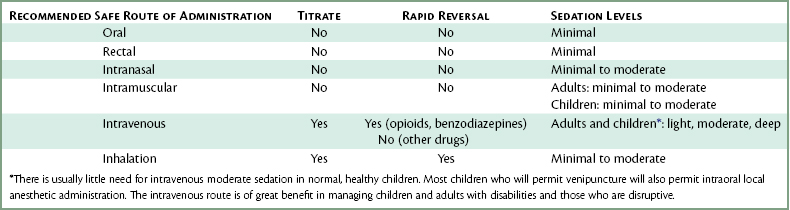
The inhalation and IV routes are the only routes that permit titration. A factor to be remembered regarding inhalation and IV sedation is that absorption of the drugs into the systemic circulation occurs rapidly, so drug responses (both therapeutic as well as adverse) develop suddenly. Titration remains the greatest safety feature these techniques possess and should always be used when possible. Table 34-1 summarizes the recommendations made throughout this book for the various routes of drug administration.
Clinical Manifestations
Sedative-Hypnotics, Including Barbiturates
Opioid Agonists
Overdose reactions to both the sedative-hypnotics and opioid agonists are produced by a progressive depression of the CNS that is manifested by alterations in the level of consciousness and as respiratory depression that ultimately results in respiratory arrest. The loss of consciousness produced by barbiturates or opioid agonists is not always the result of unintentional overdose—these drugs are commonly administered as the primary agents in general anesthesia (see Chapter 31). However, when moderate sedation is the goal, unintended loss of consciousness and respiratory depression/arrest must be considered as complications of drug administration.
Management
Sedative-Hypnotic Drugs
Management of sedative-hypnotic drug overdose is predicated on correcting the clinical manifestations of CNS depression. Stated another way, according to the “new” definitions of sedation from the American Society of Anesthesiologists9 and the American Dental Association,10 the dentist administering sedation must be capable of “rescuing” the patient who inadvertently descends into a level of CNS-depression beyond that which is intended.
Diagnostic clues to the presence of an overdose of a sedative-hypnotic drug include the following8a:

Figure 34-1 The unconscious patient should be placed in the supine position with the legs elevated slightly.
(From Malamed SF: Medical emergencies in the dental office, ed 6, St Louis, 2007, Mosby.)
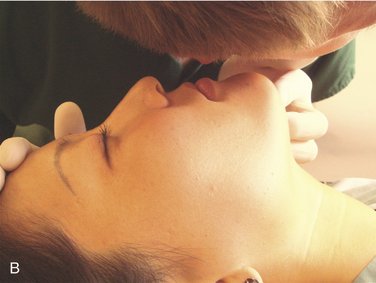
The patient might be more deeply sedated and barely responsive to stimulation, with a partially or totally obstructed airway. In this situation assisted ventilation is essential in addition to airway maintenance. With patency of the airway ensured, the patient should receive oxygen via full-face mask or nasal hood. If spontaneous breathing is present but shallow, assisted positive-pressure ventilation is indicated. This is accomplished by activating the positive-pressure mask just as the patient begins each respiratory movement (just as the chest begins to expand). The positive-pressure mask is activated by depressing the button on top of the mask until the patient’s chest rises and then releasing the button. With the self-inflating bag-valve-mask device, the bellows bag is squeezed at the start of each inhalation. With both devices, an airtight seal of the mask and head-tilt must be maintained at all times. If respiratory arrest occurs (no visible respiratory efforts), controlled artificial ventilation (rescue breathing) must be initiated. The recommended rate for the adult is one breath every 5 seconds (12 per minute) and one breath every 3 seconds for the child aged 1 to 8 years (20 per minute) and the same rate for the infant younger than 1 year old (20 per minute).11 Expansion of the patient’s chest is the only sure sign of successful ventilation. Overinflation should be avoided as this leads to abdominal distention, resulting in inadequate ventilation and an increased risk of regurgitation.
Benzodiazepine overdosage may be reversed by IV or IM administration of flumazenil, a specific benzodiazepine antagonist. Flumazenil is administered intravenously at a dosage of 0.2 mg in 15 seconds, waiting 45 seconds to evaluate recovery. If recovery is not adequate at 1 minute, an additional dose of 0.2 mg may be administered. This is repeated every 5 minutes until recovery occurs or a dose of 1.0 mg has been delivered.12
Opioid Analgesics
Diagnostic clues to the presence of an opioid overdose include the following8:
Following IV administration, naloxone’s actions are noted within 1 to 2 minutes (if not faster) and within 10 minutes following IM administration (in the presence of a near-baseline blood pressure). Naloxone is available in a 1-ml ampule containing 0.4 mg (adult dosage form) or 0.02 mg (pediatric dosage form). The drug is loaded into a plastic disposable syringe, and when the IV route is available, 3 ml of diluent (any IV fluid) is added to the syringe, producing a final concentration of 0.1 mg/ml of naloxone (adult) or 0.005 mg/ml (pediatric). The drug is then administered intravenously to the adult at a rate of 1 ml/min until the ventilatory rate and alertness increase. In children the IV dose is 0.01 mg/kg.13 If naloxone is administered intramuscularly, a dose of 0.4 mg (adult) or 0.01 mg/kg (pediatric) is administered into a suitable muscle mass, such as the middeltoid (adult) or vastus lateralis (child or adult), or sublingually (if the patient is unconscious).
Box 34-3 outlines the steps to follow in management of opioid overdose.
SUMMARY
Whenever more than one CNS-depressant drug is administered to a patient, the dosages of all drugs must be reduced from their usual dosage to prevent exaggerated, undesirable clinical responses. As demonstrated in Table 34-2, in most of the cases reported by Goodson and Moore, this step was not taken, with disastrous results often occurring.8
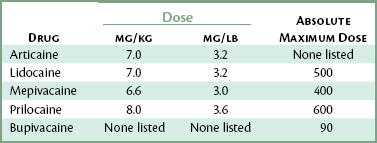
Another factor must be considered, one that most health professionals do not, as a rule, give much thought when using sedative techniques: Local anesthetics themselves are CNS depressants and can produce additive actions when administered in conjunction with drugs commonly used for sedation. The maximal dosage of local anesthetic to be administered to any patient, but especially to a child or lighter-weight adult, should be based on the patient’s body weight in kilograms (or pounds). When no other CNS depressants are being administered, this maximal dose could be reached without adverse effects if the patient is an American Society of Anesthesiologists (ASA) 1 and falls within the normal responding range on the bell-shaped curve. Table 34-3 presents the maximal recommended doses of the most commonly used local anesthetics. When a local anesthetic is administered with other CNS depressants, the local anesthetic dosage should be minimized.
How, then, may overdose reactions best be prevented? Goodson and Moore made the following recommendations concerning the use of sedative techniques involving the administration of opioids8:
The Dentists Insurance Company (TDIC), in a retrospective study of deaths and morbidity in dental practices over a 3-year period, concluded that in most of those incidents related to administration of drugs, there were three common factors.14
ALLERGY
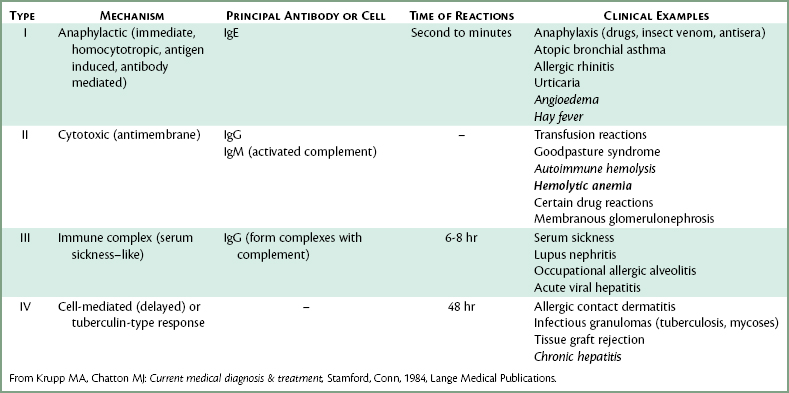
Allergy is a hypersensitive state acquired through exposure to a particular allergen, reexposure to which produces a heightened capacity to react. Allergic reactions cover a broad range of clinical manifestations, from mild, delayed-onset reactions occurring as long as 48 hours after exposure to immediate and life-threatening reactions developing within seconds of exposure. Although all allergic phenomena are important and require thorough evaluation by the dentist, only one form, the type I, or immediate, reaction is discussed here, for it may present the dentist with a life-threatening emergency situation. A classification of allergy types is presented in Table 34-4.
Allergic reactions are mediated through immunologic mechanisms that are similar regardless of the specific antigen responsible for precipitating the response. Therefore an allergic reaction to the venom of a stinging insect may be identical to that seen after aspirin or penicillin administration in a previously sensitized individual. Allergic reactions must be differentiated from the overdose, or toxic, reaction previously discussed, in which the observed signs and symptoms are a direct extension of the normal pharmacologic properties of the drug administered. Overdose reactions are much more commonly encountered than are allergic drug reactions. Of all ADRs, 85% result from the pharmacologic actions of drugs; 15% are immunologic reactions.15 To the layperson, however, any adverse drug response is frequently labeled “allergic.”
Of the many antianxiety drugs used, the barbiturates probably possessed the greatest potential for sensitization of patients. Although not nearly as common as allergy to penicillin or aspirin, barbiturate allergy usually manifests itself in the form of skin lesions, such as hives and urticaria, or less frequently in the form of blood dyscrasias, such as agranulocytosis or thrombocytopenia. Allergy to barbiturates occurs much more frequently in persons with a history of asthma, urticaria, and angioedema.16 A documented history of allergy to any barbiturate represents an absolute contraindication to their administration.
Prevention of Allergic Reactions
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses