A Maxillary Denture with Modified Occlusal Concepts Opposing an Implant Prosthesis
Carl E. Misch
Eighteen million Americans are completely edentulous, representing 10.5% of the adult population. In addition, 12 million (7% of the adult population) have no maxillary teeth opposing some mandibular natural teeth. Hence, 17% of the U.S. adult population is wearing a maxillary complete denture. Yet the average dentist spends less than 1% to 5% of his or her time treating edentulous patients.
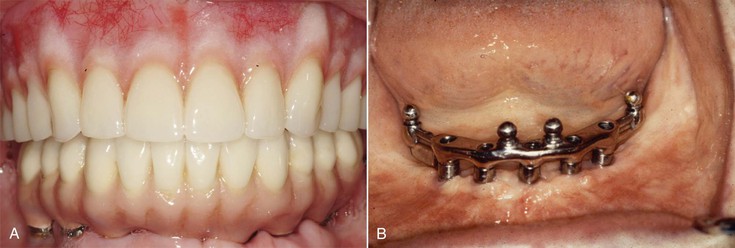
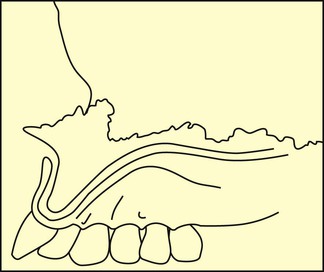
Lack of stability and retention are the most frequent complaints related to complete removable prostheses. However, patients often think that the retention and stability of maxillary dentures are acceptable and that the mandibular denture presents more problems. As a result, a common treatment plan for edentulous patients includes implants to support the mandibular restoration and a traditional soft tissue–supported maxillary denture1–3 (Figure 33-1). A maxillary complete denture may function as a satisfactory replacement for missing teeth for many completely edentulous patients. However, after a mandibular implant-supported restoration is fabricated, the patient becomes more aware of the lack of stability, support, and retention of the removable maxillary prosthesis.4,5
In many ways, the combination of a complete maxillary denture against a lower mandibular implant-supported prosthesis resembles a single complete maxillary denture opposing mandibular natural dentition. The rigid mandibular teeth make the maxillary prosthesis the least stable member of the dentition. In addition, the occlusal plane of the mandibular dentition is often variable and not ideal. This makes it even more difficult to obtain an ideal occlusal scheme to help stabilize the maxillary denture.
One may anticipate postinsertion complications of the removable maxillary restoration opposing a more rigid mandibular overdenture or fixed prosthesis. The patient complains of soft tissue sore spots and maxillary denture instability. The sore spots under the maxillary denture result in part because patients with rigidly fixated implant prostheses are able to generate masticatory forces approaching that of natural teeth, but wearers of complete dentures have been shown to exert less than 25% of this force.6 The occlusal forces are also directed in a more consistent direction and location and even may lead to midline fracture of the denture.7 In addition, more recent reports indicate that a combination syndrome effect of the maxillary arch may be developing with associated alveolar bone resorption and soft tissue inflammation.8,9
Maxillary denture instability also becomes more noticeable to the patient because of the improved occlusal awareness and stability of the mandibular counterpart.7 Mandibular implant overdentures enhance proprioception and improve the consistency of mandibular closure position. A conventional soft tissue–borne complete removable mandibular prosthesis moves up to 10 mm during function, which may accommodate any prematurities or inaccuracies of occlusion.10 The patient is accustomed to the mandibular denture lifting up from the posterior ridge during mandibular excursions. The changes of making the mandibular implant prosthesis more stable predispose to the patient’s awareness of maxillary denture instability (Box 33-1).
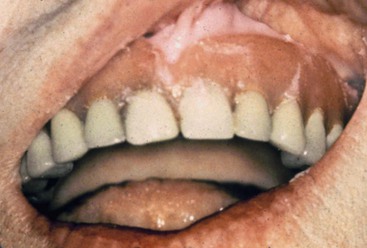
Several modalities are available to improve the prognosis of the restoration on a compromised support area. Varied soft tissue impression techniques, altered occlusal schemes, and a broad range of removable prosthetic concepts show improvement of the final restoration when opposing a stable implant-supported prosthesis. Unfortunately, many patients rely solely on denture adhesive to improve retention of the prosthesis. The inconsistent fit, need for recurrent applications, and poor taste are often consequences (Figure 33-2).
Many textbooks have been written describing the steps and fabrication of a maxillary denture, and complete guidelines are beyond the scope of this chapter. However, specific elements are discussed.
To minimize maxillary denture complications when opposing a mandibular implant restoration, the dentist can implement several concepts. These concepts include preprosthetic surgery to improve the maxillary ridge anatomy and prosthetic approaches specifically tailored to address these problems, raising the posterior occlusal plane (compared with conventional denture concepts), restoring the occlusal vertical dimension (OVD), placing the maxillary and mandibular posterior teeth more medial, and establishing bilateral balanced occlusion in the final restoration11–14 (Box 33-2). The purpose of this chapter is to highlight these areas of special concern when fabricating a maxillary denture opposing an implant-supported restoration.
Maxillary Soft Tissue Evaluation
A successful restoration with a soft tissue–supported removable prosthesis depends on several conditions. However, the anatomy of the edentulous arch foundation is the primary criterion for prosthesis support and stability.
The dentist may evaluate dentures for support, stability, retention, esthetics, masticatory efficiency, speech, extension, and occlusion. Support of a maxillary denture is determined from the resistance of the denture to a vertical force direction applied to the denture. The crest of the residual ridge and the overlying tissue is the region most responsible for support.15,16
The foundation of the maxillary denture is bone, the overlying submucosa, and the mucosa. The blood vessels and nerves are located in the submucosa and bony architecture. Denture support for a maxillary denture primarily corresponds to the regions where fibrous connective tissue is attached firmly to bone, namely, the edentulous ridge.16 The dentist rarely can exploit the concept of placing teeth over the residual crest to improve support in the anterior region because the resorption process has brought the ridge palatal to the ideal denture tooth position.
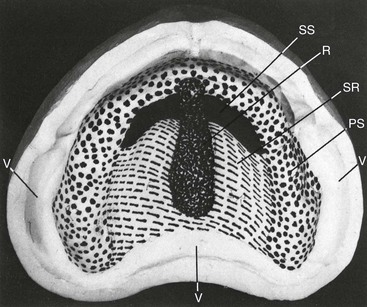
Contrary to popular belief, the palate of the maxilla is not a primary support region for a maxillary denture or implant overdenture.16 Whereas the tissues over the midpalatal suture are usually thin and nonmobile, the surrounding mucosa can be displaced under minimal pressure. The denture base can be relieved selectively in this region to prevent it from acting as a fulcrum, with resultant instability and soreness when vertical forces are transmitted through the maxillary prosthesis. The maxillary denture opposing an implant-supported restoration is subjected to greater forces, and the dentist should consider generous relief of this area to prevent soft tissue trauma. The midpalatal area is a relief zone because the overlying tissues are thin compared with the rest of the maxilla.
The dentist also should provide denture relief to the incisive papilla region to prevent compression of the associated blood vessels and nerves during function. This may eliminate a burning sensation during function from compression of this tissue, especially under the increased bite forces from a mandibular implant prosthesis.
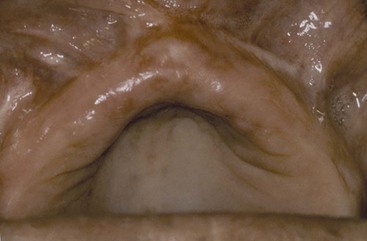
The posterior aspect of the hard palate is an area of secondary retention, not support.15,16 The submucosa is rich in mucous glands and blood vessels, granting greater resiliency under vertical forces. This region is loaded in a lesser amount by the denture compared with the crest of the ridge or premaxilla (Figure 33-3).
Retention is determined as resistance to a vertical incisal or occlusal force direction or pulling force applied to a denture. The valve seal of the periphery of the denture and the close approximation of the intaglio aspect of the denture are the important considerations for retention. Anatomical features that contribute to the performance of the maxillary denture may vary greatly, but the ability to maintain a border seal during function is much greater than with a mandibular denture and often compensates for other limiting retention factors.17,18
The maxillary tuberosities should be firm and located several millimeters superior to the plane of occlusion. Surgical removal of hyperplastic tissue is indicated. The hamular notch is located halfway between the maxillary tuberosity and the hamulus of the medial pterygoid plate. The posterior palatal seal is positioned through this area of loose connective tissue to improve tissue contact and retention. The pterygomandibular raphe attaches from the hamulus to the retromolar pad and should not be impinged on. The posterior limit of the prosthesis is correlated with the soft palate vibrating line, which is more an area than a definite line.15,16
Stability of the denture is the resistance of movement to a lateral force applied to the denture. The vertical component of the residual ridge from the hard palate is primarily responsible for improving stability. The premaxillary segment of the edentulous maxilla is a most important structure to ensure stability of the prosthesis. The denture stability is compromised severely without a vertical component to the premaxilla.17 In addition, the rugae area of the premaxilla is the secondary stress-bearing region.15,16 This region also helps resist the forward movement of the denture during excursive mandibular movements. It is important to make the patient aware of the continued bone loss in the premaxilla under a denture. Unless implants are inserted to stimulate the bone, the bone loss is continuous, and the denture will become less stable.
The type and movement of the supporting tissue are also important parameters to consider in edentulous ridge correction. The soft tissues of the maxillary ridge should be firm to lateral forces to limit denture movement during occlusion. The amount of tissue movement over the bone can affect denture stability directly and cause soft tissue abrasions. If one observes excessive mobility of the anterior or posterior ridges, the dentist should consider soft tissue preprosthetic surgery. If the tissue is mobile, the denture cannot have stability to any lateral force.
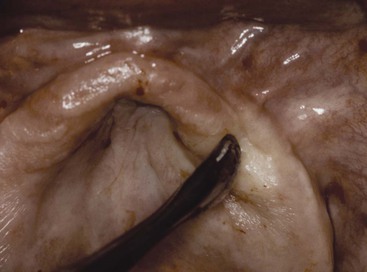
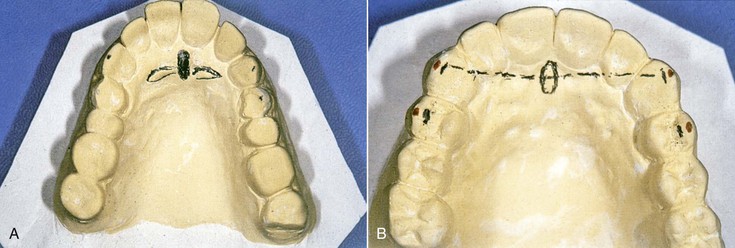
The oral mucosa classically has been described as a movable, unattached, nonkeratinized mucosa or as a nonmobile, attached, keratinized mucosa. These two categories are oversimplified for denture support. Attached keratinized mucosa has been recognized to increase in thickness as a result of bone resorption, primarily in the anterior maxilla. This tissue thickness often exceeds several millimeters and becomes highly mobile. Although classified as attached gingiva, the tissue serves as a poor denture base (Figure 33-4). Likewise, unattached, nonkeratinized tissue may become thick and nonmobile tissue by interposing hydroxyapatite (HA) between the bone and periosteum. This tissue then can serve as an adequate denture-supporting base. Therefore, clinically relevant qualities of tissue for denture support relate to thickness and mobility, not necessarily to the histologic surface condition.
Hard Tissue Evaluation
Surgical techniques that can improve the support of a prosthesis in the maxilla include alveolar ridge augmentation. Autogenous bone grafts for ridge augmentation is a viable alternative in the atrophic maxilla if implants are placed shortly after the graft surgery. If the autogenous graft is used only for improved soft tissue support, as much as 90% of the grafted bone may resorb within 3 to 5 years after augmentation surgery.19 During the rapid resorption process, the soft tissue–supported denture needs repeated relining and rebasing procedures to maintain ridge contact. The resultant soft tissues become highly mobile and unsupported by the resorbing ridge. The patient often complains of recurrent soft tissue abrasions and of mobile, unstable, and poorly retentive prostheses. Hence, implants must be used to maintain the bone formed after a bone graft.
Dense nonresorbable HA used as a ridge augmentation material to enhance the denture support area has proved an adjunct in preprosthetic surgery in which implant placement is not part of the immediate future treatment plan.20 HA ridge augmentation can slow down the rate of ridge resorption. The dense material can bond to the cortical bone and increase the amount of denture support. Clinical experience demonstrates longer periods between relining the maxillary prosthesis after HA augmentations.21,22
The maxilla can be divided into three regions: the left and right posterior segments and the anterior segment. The posterior maxilla rarely requires ridge augmentation for improved ridge shape or contour. The tuberosity region usually maintains ridge form. The posterior palatal seal area of the denture does not depend primarily on the posterior ridge form. The posterior region is usually adequate to give lateral stability in the posterior region regardless of posterior ridge contour.
The bone anatomy of the premaxilla is primarily responsible for the varying degree of stability of maxillary dentures. After the loss of teeth, the bone first resorbs in width, and the incisive papilla eventually becomes the most anterior part of the edentulous ridge. The anterior limit of the papilla is usually 7 to 9 mm behind the incisal edge of the central incisors, and the anterior edentulous ridge is considerably diminished. The maxillary anterior teeth positions are dictated by esthetic and functional requirements. The more anterior and incisal position of the denture teeth from the underlying bone results in less denture stability during function.
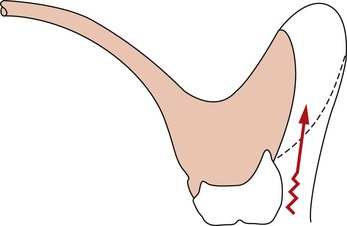
The vertical component of the anterior maxilla is also the primary element that prevents anterior rotation of a complete removable maxillary prosthesis and loss of posterior value seal. Anterior forces commonly are generated against maxillary prostheses during mandibular excursions, especially during the anterior incision of food. During chewing, the bolus of food acts as a fulcrum for denture rotation (Figure 33-5). Therefore, the primary role of the premaxilla under function is to oppose denture dislodgment and improve the stability of the removable prosthesis.
Hydroxyapatite Indications
The maxillary bone division A ridge usually has the height and width of bone to support, retain, and stabilize the prosthesis. On occasion, labial undercuts may compromise retention and increase soft tissue abrasions. As a result, the dentist may fill in labial undercut areas with HA to improve the ridge contour. The division B and C–w anterior ridges or class I and II ridges from the Kent et al. classification are suited ideally for HA ridge augmentation22 (Figure 33-6). The dentist may perform a vestibuloplasty in the same procedure to increase the height of the anterior ridge and further improve stability and retention (Figure 33-7). The patient wears a surgical stent for 10 to 14 days to support the graft and maintain the dimension gained with the vestibuloplasty.
The division D and C–h ridges are least suited for HA augmentation. Although these ridges are in greater need, the poor ridge form provides insufficient structure to resist future migration of the HA in the labial fold and may compromise long-term success.14
Hydroxyapatite ridge augmentation rarely is indicated for the mandibular arch. The mandibular denture moves up to 10 mm during function compared with about 2 mm of movement for the complete maxillary denture.10 Ridge augmentation alone does not provide enough improvement for successful mandibular denture support. In addition, sore spots are more common on the thinner, nonmobile tissues; migration of the augmentation material is of greater occurrence (especially in moderate to severely atrophic ridges) along with paresthesia of the mental nerve.23 Endosteal implants provide much greater support, retention, and stability for the mandibular denture. However, the maxillary edentulous arch and complete denture often can benefit from HA ridge augmentation.
Ridge Shape
In many instances, the incorrect assumption has been made that the larger the alveolar ridge, the better the retention and stability of the denture. The anatomical element most likely to change after HA augmentation is the ridge shape or form. As a result, many alveolar HA ridge augmentations have resulted in greatly increased ridge size but decreased retention and stability. One must appreciate the shape of the ridge in developing the relationships among retention, stability, and support criteria for a maxillary removable prosthesis.
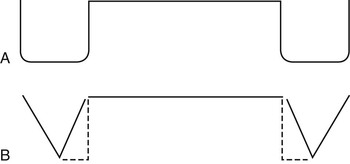
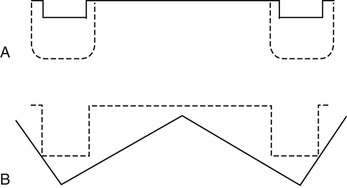
Alveolar ridge shape may be classified related to retention. The ideal ridge form for retention has high, broad parallel walls that also improve lateral stability even if vertical displacement occurs. Therefore, retention and stability are affected by the lateral aspect of the ridge contour (Figure 33-8, A). A flat, atrophic ridge provides poor stability but improved support for a maxillary denture. The least stable ridge shape is the V-shaped ridge at an angle to the opposing force. This ridge shape is also poorest for retention and support (Figure 33-8, B).
The V-shaped ridge is a common ridge form resulting from HA ridge augmentation surgery, which oversizes the ridge at its base with the particulate HA. The ideal ridge is flat at the crest (and under the teeth) for support and has parallel walls on the ridge sides for retention and stability.15,16 Hence, ridge shape affects retention, support, and stability, and ridge form correction should be designed to provide an ideal ridge form (Figure 33-9).
The primary long-term goal of premaxillary HA augmentation is to achieve a square ridge shape that can sustain the increased masticatory forces developed by the opposing arch. Other benefits are a reduction of soft tissue movement, a decrease in the rate of bone resorption, and maintenance of the vertical component of the anterior ridge.
Maxillary Denture Impressions
Four methods may be used to improve the retention of a maxillary denture: (1) a valve seal that completely fills the vestibular border, (2) the extension of the posterior limit of the denture, (3) the accuracy of the intaglio aspect of the prosthesis, and (4) the design of the post dam.
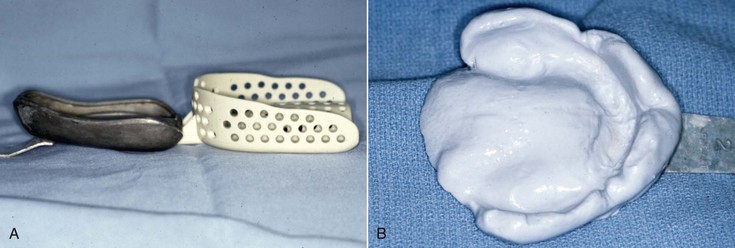
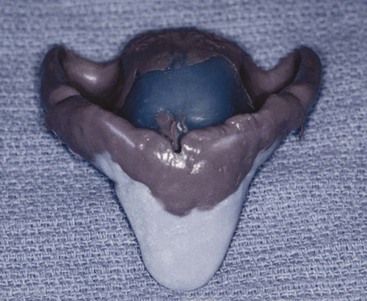
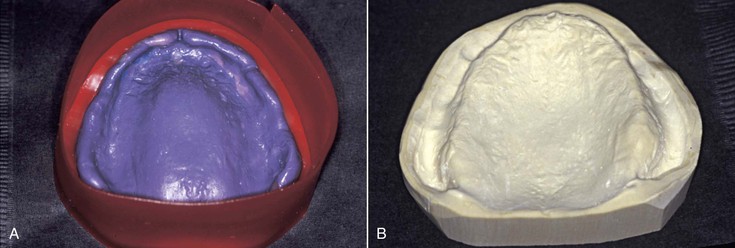
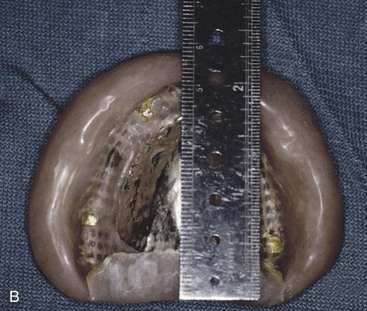
The final impression tray should be 2 to 3 mm short of the peripheral vestibular tissues to provide space for border molding. Existing dentures should not be used as an impression tray because they are usually overextended in the labial vestibule because bone resorption has occurred since their initial delivery. Impression trays designed for teeth are overextended for complete denture impressions. Therefore, they should not be used even for preliminary impression to design the custom tray (Figure 33-10). The dentist may perform border molding procedures on the custom tray using polyether or compound, and each has some advantages (Figure 33-11). The peripheral seal designed from the border molding should completely fill the vestibular space to improve retention and decrease food impaction under the denture (Figure 33-12). Regardless, when the border molding procedure is completed, the maxillary custom tray should have good valve seal retention (before the final impression is made) (Figure 33-13). If not, the dentist should consider extending the posterior palatal seal position in the final impression and the denture. When the denture impression is poured in stone, it should be boxed so the peripheral border is reflected in the cast (Figure 33-14).
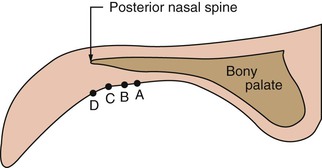
The literature gives many methods to determine the extent of posterior palatal seal, and each one gives a slightly different position (Figure 33-15). One method has the patient hold the nose, close the mouth, and attempt to force air out at the same time. The palatal drape is pushed down from the hard palate and results in a posterior line for the extension of the denture. This technique results in a position farther anterior than the other methods. As such, this technique provides the least retention for the final prosthesis and is therefore limited to patients complaining of a gag reflex when the denture extends posteriorly too far.
Another option to determine the posterior extent of the denture is to extend the palatal seal to the fovea palatinae. This results in an intermediate denture extension (Figure 33-16). In addition, these small openings off the midline are usually difficult to observe and therefore cannot be used routinely in a clinical setting.
A third technique to determine the posterior extent of a denture is to ask the patient to say, “Ah.” The “vibrating line” between the mobile soft tissue and the palate results in the most posterior position (Figure 33-15, position C). As such, this is the technique most often used to determine the posterior limits of the denture.
Some patients do not mind when the posterior limit of the denture extends beyond the vibrating line (Figure 33-15, position D). When valve seals are poor, the posterior extension of the maxillary denture may compensate and improve the overall retention. Hence, when resorption is moderate to advanced and other treatment modalities such as an implant overdenture are not considered, extension of the posterior limit of the denture beyond the vibrating line improves the retention of the prosthesis.
The third method to improve retention of a maxillary denture is related to the intaglio adaption of the denture. To improve the accuracy of fit for the intaglio aspect of the dentures and to protect the underlying bone, the tissue thickness should be at full thickness when the impressions are made. Kydd et al. demonstrated that maxillary soft tissues loaded for 10 minutes may be compressed to 60% of their original thickness and remain at 65% to 85% for extended periods, with 4 hours necessary for complete recovery.24 In an older patient, the recovery of tissue thickness after 10 minutes of compression may be 2 or more hours (Figure 33-17). Therefore, final denture impression and delivery follow certain guidelines.
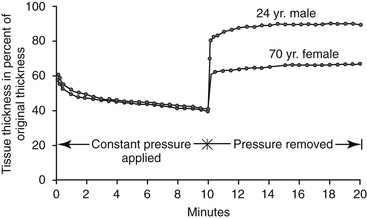
A tissue conditioner can improve the tissue health and help obtain the final tissue thickness while the prosthesis is worn before making the final impression. The denture should be removed at least 4 hours before the final impression. This often means the appointment for the final impression should be in the early morning before the patient eats, and the patient should leave the prosthesis out the night before the appointment. As important, a similar routine is repeated on the day the denture is delivered. Otherwise, the soft tissue may be compressed, and the retention at initial delivery may prove to be less than ideal.
The adaption of the intaglio surface of the denture may also be improved by decreasing the amount of acrylic shrinkage during processing of the denture. The use of an injection-molded processing technique to minimize acrylic shrinkage and improve the fit and retention of the final denture is of benefit. The retention may also be improved by a post dam along the posterior limit of the prosthesis. The post dam is used to compensate for the shrinkage of acrylic during the processing of a denture.
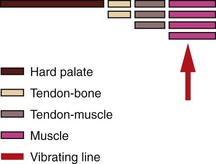
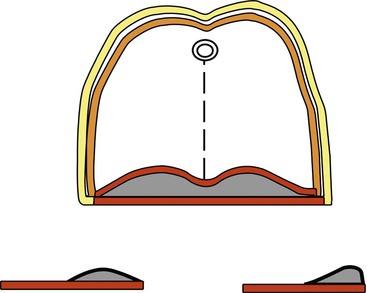
The fourth aspect to improve maxillary denture retention is the post dam design. A common post dam design forms a hill, with the greatest height (depth to tissue) in the middle, and sloping posteriorly and anteriorly.15,16 This contour does not adequately reflect the anatomy of the soft tissue above the vibrating line. When the limit of the denture is established by saying, “Ah,” the anatomy of the soft palate directs the design of the post dam. Directly above the vibrating line is a muscle, which has the most flexibility. The muscle is attached to a tendon (with slightly less movement) that attaches to a hard palate covered by soft tissue that has the least movement (Figure 33-18). Therefore, the depth of the post dam should be greatest in the posterior area and then slant toward the tissue of the hard palate (Figure 33-19). The initial depth varies for each patient and is determined by depressing the area in the mouth with a mirror or blunt object.25
Maxillary Anterior Tooth Position
Several texts on denture fabrication state that the first step in the reconstruction is determining the OVD followed by the position of the lower anterior teeth.15,16,25,26 However, the maxillary anterior horizontal and vertical tooth positions should be evaluated before any other segment of the reconstruction, including the OVD.14 If the maxillary incisor edge is modified in either the horizontal or vertical plane, all other elements of the maxillary and mandibular prosthesis may also need to be changed. No other region of the mouth should be restored until this position is obtained because it negatively influences the proper position of every other segment (e.g., OVD, mandibular anterior tooth position, and posterior planes of occlusion).
The patient’s existing maxillary complete denture often has the maxillary anterior tooth position incorrect. The resorption of the premaxilla causes the denture to shift apically and posteriorly following the bone loss pattern. A base plate and wax rim first evaluates the position of the maxillary anterior teeth. At this point, the evaluation is not for the cosmetic aspects of tooth color or shape, but tooth position is scrutinized. After this is determined, the maxillary occlusal plane, OVD, mandibular incisive edge position, posterior mandibular teeth, and last the maxillary posterior teeth are determined (Box 33-3). Arch relationships are often affected by resorption patterns in edentulous ridges. The anterior and posterior edentulous maxilla resorbs toward the palate after tooth loss.27 The width of the alveolar ridge decreases 40% within a few years, primarily at the expense of the labial plate. This results in a cantilevered force on the denture teeth. The maxilla is affected more often than the mandible because the incisal edge position in the esthetic zones cannot be modified and is dictated by esthetics, speech, lip position, and occlusion.
The anterior location of the occlusal plane is determined by the maxillary incisal edge position. The farther forward the maxillary anterior denture teeth, the more leverage off the anterior bone and the more likely the maxillary anterior teeth will tip up and the posterior palatal seal will fail, with the upper denture dropping from the ridge. Yet many dentists attempt to do plastic surgery with plastic, hoping to eliminate vertical facial lines in the lip by bulking up the labial flange and positioning the teeth forward from the ridge (Figure 33-20).
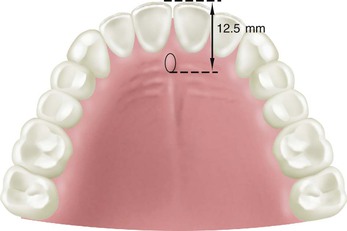
The dentist inserts the base plate and wax rim into the patient’s mouth and first determines the labial contour of the maxillary lip because modification at a later step may alter all other measurements. Most often the facial surfaces of the central incisors are 12.5 mm from the most posterior aspect of the incisive papilla or 7 to 9 mm from its anterior limit28 (Figure 33-21). Hence, the dentist initially positions the wax rim this far forward at the midtooth position. The philtrum of the lip should be a visible depression in the midline under the nose. If the philtrum is flattened, the lip is extended too far, and wax should be removed from the labial of the wax rim. In addition, in 92% of cases, the line drawn from the tip of the canines has been shown to bisect the incisive papilla29 (Figure 33-22).
The labial position of the maxillary anterior teeth is then evaluated with the patient at a relaxed vertical dimension. This is pr/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses