Cleft–Orthognathic Surgery
The Unilateral Cleft Lip and Palate Deformity
• Facial Growth Implications of Cleft Palate Repair in the Infant with Unilateral Cleft Lip and Palate
• Timing of Orthognathic Surgery
• Residual Deformities in the Adolescent with Unilateral Cleft Lip and Palate
• Orthodontic Considerations in the Patient with Unilateral Cleft Lip and Palate with a Jaw Deformity
• Immediate Presurgical Re-Assessment
• Orthognathic Approach for Unilateral Cleft Lip and Palate Deformities
• Clinical Management after Initial Surgical Healing
• Orthognathic Surgery for Unilateral Cleft Lip and Palate: Review of Study
• Skeletal Stability after Modified Le Fort I for Unilateral Cleft Lip and Palate: Review of Study
In 1880, the pioneer orthodontist Normal W. Kingsley stated the following in his remarks about surgical operations as a means of correcting cleft palate: “Although the practice [of cleft palate repair] has been tested in thousands of cases by the most eminent surgeons of their time, it has resulted in such uniformity of failure [i.e., severe jaw deformities], that it should have been utterly abandoned years ago.”85
In 1920, another preeminent orthodontist of his day, Calvin Case, voiced a similar sentiment: “[L]et us hope that the proportion of [cleft palate] surgical failures will be greatly lessened in the future and that well-informed, honest surgeons … accept only the most favorable cases with a determination to follow them through with proper interest.”16
In 1965, Vilray Kazanjian, who was a leading maxillofacial surgeon of the first half of the twentieth century, reminded us that “the relative value of surgery to repair a cleft palate has been intelligently questioned for over 150 years.”83
Facial Growth Implications of Cleft Palate Repair in the Infant with Unilateral Cleft Lip and Palate
Effects of Cleft Palate Repair in Infancy
The management of individuals with unilateral cleft lip and palate (UCLP) presents specific clinical challenges for the maxillofacial surgeon, the orthodontist, and the restorative dental team. Orthognathic surgery is a procedure that should be considered as part of the treatment algorithm for patients with UCLP. Ross completed a multicenter, long-term facial growth study to assess the need for orthognathic surgery among individuals born with complete UCLP who had undergone primary lip and palate repair during childhood. He concluded that, even by the most conservative standards and in conjunction with maximum compensating orthodontic camouflage maneuvers, at least 25% of adolescents with UCLP required orthognathic surgery to achieve even the limited objective of a neutralized occlusion.148 His research indicated that only 25% of adolescents with UCLP had near-normal maxillary growth and that another 50% were in a borderline category with some degree of maxillary hypoplasia. Ross stated that individuals who were born with a cleft lip and palate have an intrinsic deficiency in the midfacial skeleton that is made worse by operations. More recently, Mulliken and colleagues reviewed the prevalence of Le Fort I osteotomies among patients with cleft lip and palate who were treated at Boston Children’s Hospital.55 They found that 48% of UCLP patients who underwent repair in infancy later required orthognathic surgery. The study also showed that the need for orthognathic surgery is dependent on the severity of the cleft type as well as the number and extent of previous operative procedures. Similarly, The Hospital for Sick Children in Toronto, Ontario, Canada, found that 48.3% of their patients (i.e. treated since infancy) with complete UCLP required orthognathic surgery. When they looked at all patients with UCLP who were referred to their center, they found that 59.4% needed jaw surgery.27 A retrospective cohort study of five prominent cleft palate centers in North America compared the maxillomandibular relationships of individuals with non-syndromal complete UCLP (n = 169).63 The one center that incorporated primary alveolar bone grafting showed especially poor maxillary growth, with 66% of its patients requiring orthognathic surgery. Interestingly, at the one center in which a single surgeon performed all of the surgeries with the use of a more delayed approach to cleft palate repair and whose patients underwent no revisions until they were 14 years old showed the lowest need for orthognathic surgery at less than 25%.
Saperstein and colleagues described the facial growth of children with complete clefting of the primary palate (i.e., the lip through the incisal foramen) but with an intact secondary palate (i.e., the incisal foramen through the uvula).151 This was a retrospective, cross-sectional analysis of non-syndromal patients with unilateral complete clefting of the primary palate as compared with those with unilateral complete clefting of both the primary and secondary palates. Angular and linear measurements of the midfacial region were made on lateral cephalograms. The study groups included those with unilateral complete clefting of the primary palate (n = 25) and those with unilateral complete clefting of the primary and secondary palate (n = 18). The study documented that individuals with a cleft of only the primary palate who underwent lip repair during infancy typically had a normal or even slightly forward maxillary position as compared with age-matched controls. This was in contrast with children with a cleft of both the primary and secondary palates who underwent lip repair followed by palate repair before they were 1 year old; this group showed a high incidence of maxillary deficiency. The study clarified that the cleft palate repair carried out before 1 year of age—and not the cleft lip repair itself—was responsible for the high incidence of midface hypoplasia.
Effects of Achieving Bone Fusion Across the Cleft Alveolus during Infancy
Reconstruction of the alveolar process in patients with UCLP is an essential part of cleft care. Accomplishing this goal provides support for the alar base of the nose; the teeth in the cleft region; and the periodontium that surrounds those teeth (Figs. 32-1 and 32-2). There are three basic methods that have been described for the closure of the cleft alveolus: 1) primary bone grafting; 2) secondary bone grafting; and 3) gingival periosteoplasty (GPP).56 The method of primary bone grafting is now generally recognized to result in severe midface growth disturbance and has therefore been universally abandoned throughout the world.63,148 The use of secondary (mixed dentition) bone grafting is generally recognized as an effective method to avoid the problem of additional midface growth disturbance and to successfully achieve support for the alar base; to provide bone for the eruption of the canine through the grafted cleft site; and to establish effective periodontal support (Figs. 32-3 through 32-6).1
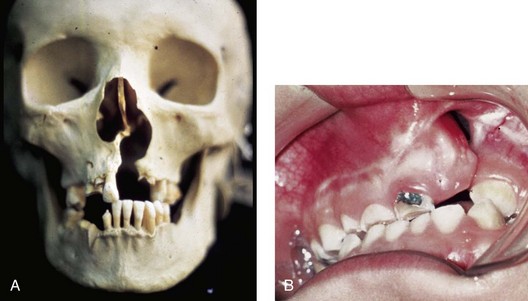
Figure 32-1 A, The maxillofacial skeleton of an adult with unrepaired unilateral cleft lip and palate (UCLP) is shown. Typical UCLP deformities of the hard palate, the alveolus, the nasal septum, the floor of the nose, the nasal spine, and the pyriform rims are demonstrated. B, An occlusal view of a child born with UCLP who presented during the mixed dentition with a residual alveolar/palatal skeletal defect and a labial and palatal oronasal fistula is also shown.
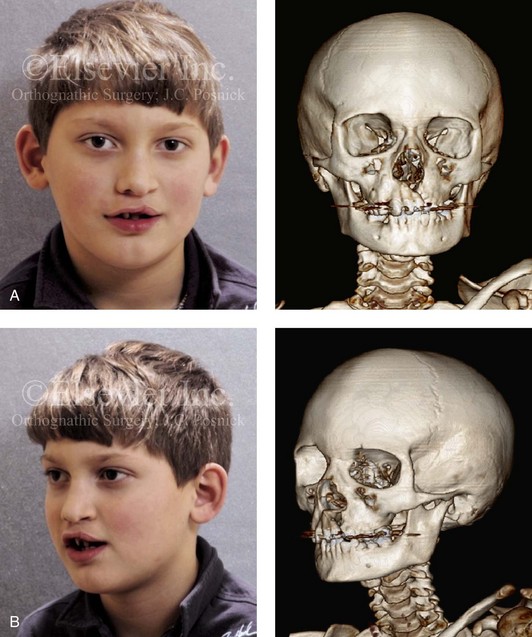
Figure 32-2 A 6-year-old boy who was born with a UCLP is shown after soft tissue lip and palate repair in infancy. A, Frontal and B, oblique facial and computed tomography scan views during the mixed dentition demonstrate residual cleft skeletal defects and deformities that were present before grafting and fistula closure.
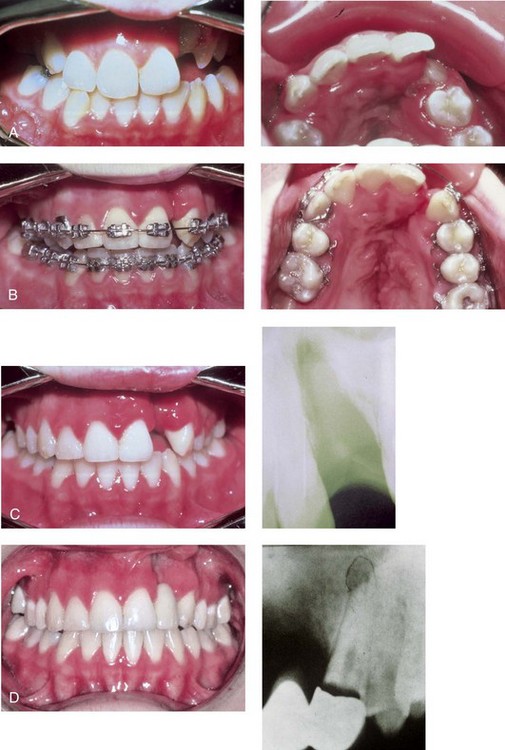
Figure 32-3 An example of the suboptimal management of a unilateral alveolar/palatal cleft. A child who was born with UCLP underwent soft tissue lip and palate repair during infancy. She underwent orthodontic treatment and achieved a satisfactory overjet and overbite. The alveolar/palatal cleft skeletal defects and the residual labial and palatal oronasal fistula were ignored. The maxillary lateral incisor tooth was inadequate and required extraction. The canine erupted adjacent to the cleft, and the dental gap was orthodontically retained. Dental rehabilitation was accomplished with a three-unit bridge to manage the cleft–dental gap. Limited periodontal (bone) support of the cleft-adjacent teeth (the canine and the central incisor) resulted in a periodontic–endodontic problem with a loss of the canine and poor support of the central incisor. These problems would not have occurred had effective bone grafting and fistula closure been carried out during the mixed dentition. A, Occlusal and palatal views during the mixed dentition before the full eruption of the canine through the non-grafted alveolar cleft. B, Occlusal and palatal views are also shown during orthodontic alignment (extraction of right bicuspid was carried out). C, Occlusal view at the completion of orthodontic alignment. A periapical radiograph indicates limited bony support of the cleft-adjacent teeth. D, An occlusal view is next shown after the placement of a three-unit bridge across the cleft–dental gap. A periapical radiograph confirms that, after several years, a periodontal–endodontic problem resulted in irreversible injury to the cleft-adjacent canine.
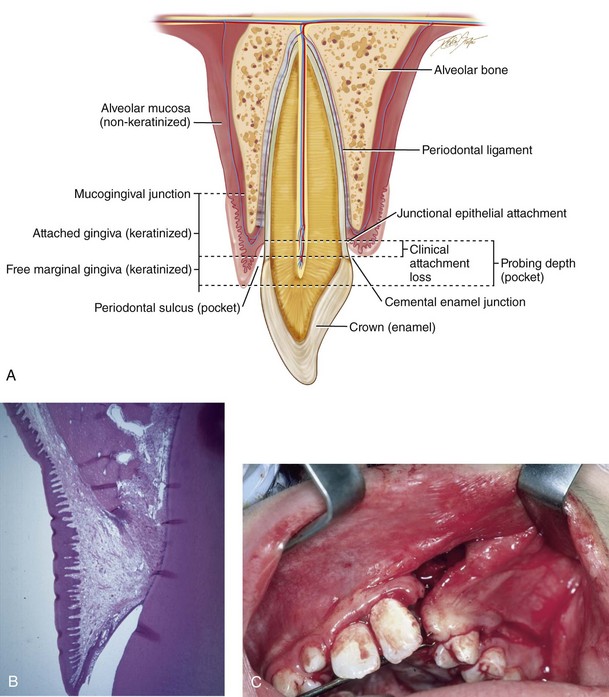
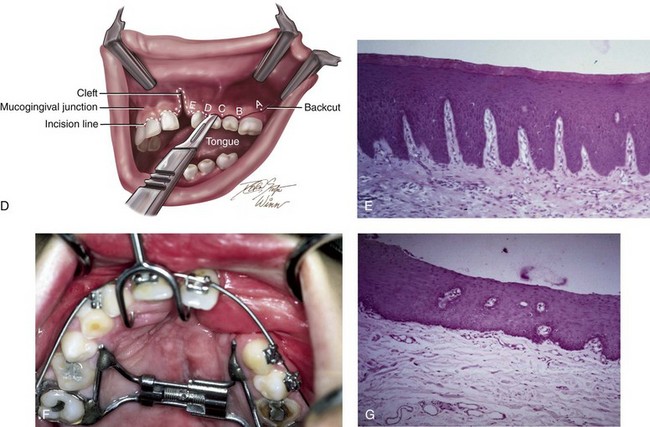
Figure 32-4 The importance of maintaining keratinized tissue adjacent to the cervical margin of each tooth for long-term periodontal health cannot be overemphasized (see Chapter 6). A, Illustration of a cross-section of dentoalveolar anatomy that indicates the location of the gingiva (keratinized mucosa) adjacent to the tooth surface. B, Low-power histomicrograph cross-section of the dentoalveolar anatomy that indicates the microscopic character of the keratinized mucosa adjacent to the tooth surface. Just deep to the keratinized epithelium rete pegs, organized fibrous tissue can be seen. C, Intraoperative view of an elevated mucogingival flap advanced anteriorly for the closure of the labial aspect of the cleft oronasal fistula. The flap brings the gingiva into the region where the canine will erupt. D, Illustration of incision placement for the elevation of the mucogingival flap. The flap splits the attached gingiva posteriorly adjacent to the first molar so that the advancing flap brings keratinized tissue into the cleft site without denuding the attached gingiva from the posterior teeth. E, Low-power histomicrograph that demonstrates keratinized epithelium, organized fibrous tissue, and rete pegs. F, Palatal view of a patient with UCLP during the mixed dentition. This patient underwent the closure of an oronasal fistula using a buccal “finger” flap by another surgeon. This is not the preferred way to rearrange the intraoral tissue for fistula closure; the labial vestibule is destroyed, and non-keratinized buccal mucosa is brought into the region where the canine will erupt. G, Low-power histomicrograph of non-keratinized buccal mucosa. Note the thin layer of non-keratinized epithelium with the underlying loose areolar connective tissue. Part D modified from an original illustration by Bill Winn.
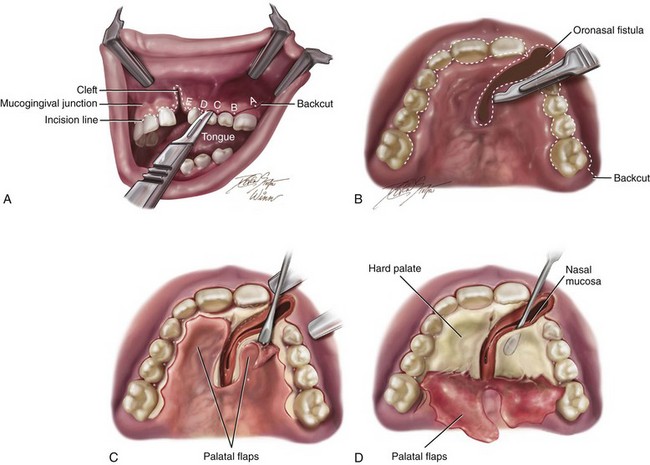
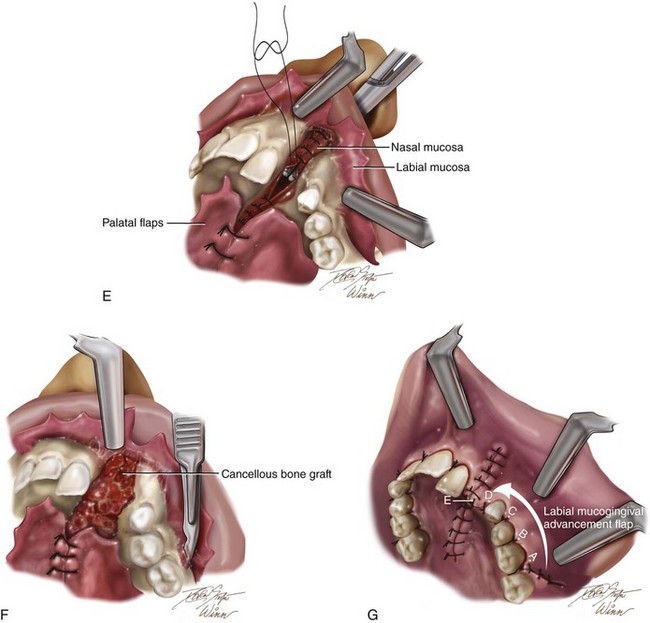
Figure 32-5 Illustrations of basic technique for bone grafting and the management of residual oronasal fistula during the mixed dentition of a child with a UCLP. If required, orthodontic expansion to correct the arch width precedes mixed-dentition bone grafting. A, A view of the left labial mucogingival incision in progress. B, Attention is turned to the sharp palate for the separation of the oral and nasal mucosa at the site of the fistula and then the elevation of the flaps. C, Subperiosteal elevation of the palatal flaps. D, With the palatal flaps elevated, the nasal mucosa is separated from the floor of the nose on each side. Left and right labial flaps have already been elevated. The nasal mucosa is further separated from the bony surface along the distal aspect of the central incision for later closure. Part A modified from an original illustration by Bill Winn. E, Suturing of the nasal flaps for watertight closure is in progress. A hemostat is placed through the left nostril to demonstrate the partially sutured nasal floor. The palatal flaps have been sutured together for fistula closure. F, After the nasal flaps are sutured, iliac cancellous bone graft is packed into the palatal, alveolar, and floor-of-the-nose skeletal defects. G, Left and right labial and palatal flaps are advanced for watertight closure. By advancing the left labial mucogingival flap, the keratinized tissue has been placed over the alveolar ridge, where the canine will eventually erupt. This is accomplished by splitting the attached gingiva at the last molar.
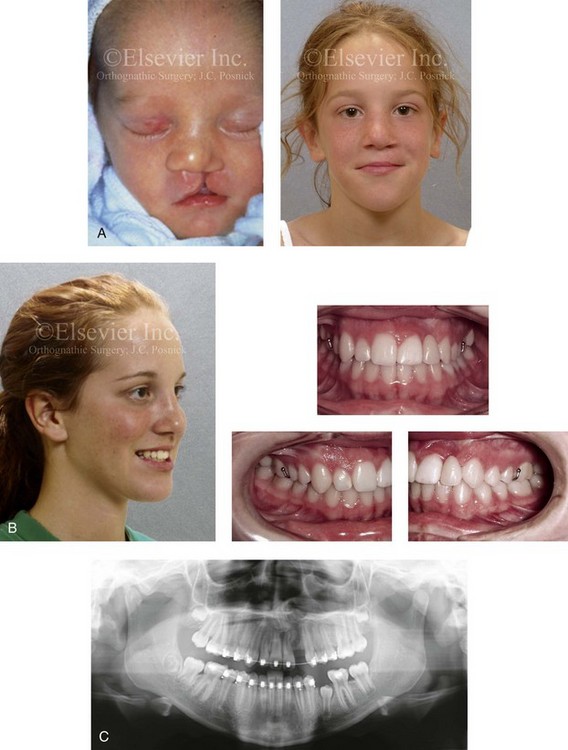
Figure 32-6 A 16-year-old girl was born with van der Woude syndrome, including UCLP and lower lip pits. She has been managed by this surgeon since her birth. She underwent lip and palate repair during her early childhood, which was followed by successful bone grafting and fistula closure during the mixed dentition. She had normal maxillary growth and underwent standard orthodontic treatment with the maintenance of the cleft–dental gap. She underwent an open rhinoplasty that included the use of a septal cartilage (caudal strut) graft when she was 15 years old. There is sufficient bone volume and attached gingiva for a dental implant, which is planned for when she is 18 years old. A, Facial views at the time of birth and during the mixed dentition, just before alveolar/palatal bone grafting. B, Facial and occlusal views taken when the patient was a teenager after rhinoplasty and before dental implant placement. A removable retainer that includes the missing lateral incisor is in place. C, Panorex image taken when the patient was a teenager during orthodontic treatment indicates successful bone grafting of the alveolar cleft.
The technique of GPP was first described by Skoog in 1965 as a method to achieve fusion across the cleft alveolus at the time of lip repair. The goal was to “remove” the cleft during infancy with the hope that no harm would result.156 Millard included the use of the Latham device to position the alveolar ridges close to one another before going forward with the GPP procedure at the time of lip repair.105,106 Grayson and Cutting later proposed the use of a nasoalveolar molding device before the GPP and primary lip repair to accomplish the same alveolar ridge fusion. Several studies confirm that the GPP procedure has a high osteogenic potential that results in the deposition of bone to achieve successful fusion of the alveolar ridge. Unfortunately, clinical studies do not confirm sufficient bone fill to consistently allow for the eruption of the canine through the ridge and to provide ideal periodontal support. Since the late 1970s, clinical studies have been carried out to assess the long-term effects of GPP on midfacial growth in cleft patients.
In 1999, Millard and colleagues used serial dental casts to evaluate the effects of GPP on maxillomandibular relationships.106 They found a greater frequency of anterior crossbite in the GPP group than in the non-GPP group. They also confirmed that the GPP group had a shorter anteroposterior length of the maxilla as compared with the non-GPP group at 6 years of age. Similar findings of poor midface growth have been documented by Berkowitz and colleagues,9 Matic and Powers,99 and others.70,169 In 2005, Renkielska and colleagues evaluated the impact of GPP on occlusal relationships with the use of the Goslon Yardstick occlusal grading system.143 They found that patients treated with GPP had a poor occlusal relationship and a Goslon Yardstick score of 4 and 5, thus indicating need for orthognathic surgery. They reaffirmed that the inclusion of the alveolar process in the primary lip repair increased severe occlusal maldevelopment.
More recently, Hsieh and colleagues completed a retrospective clinical study to evaluate the effects of GPP on facial growth in patients with UCLP.74 Sixty-two consecutive patients with non-syndromal complete UCLP with records from when they were 5 years old were included in the study. All of the patients had received nasoalveolar molding treatment before primary lip repair. Those individuals who underwent GPP at the time of lip repair (n = 26) were placed in one group. Those that did not undergo GPP at the time of lip repair (n = 36) were placed in another group. Cephalometry was used to evaluate facial growth at 5 years of age in the two treatment groups. GPP was found to have significant negative effects on the maxillary position (i.e., diminished horizontal projection), the intermaxillary position (i.e., negative overjet), the maxillary length, and the maxillary alveolar length at the age of 5 years. The authors concluded that, in patients with UCLP, the sagittal growth of the maxilla was significantly adversely affected by the GPP procedure. As a result of their study, the Chang Gung Cleft Center no longer uses the GPP technique.
Coordinated Team Approach
Care of the patient with UCLP is best delivered by an integrated group of specialists who evaluate and provide comprehensive definitive care. It is no longer acceptable for individual practitioners (e.g., surgeons, orthodontists, restorative dentists, speech pathologists, otolaryngologists) to carry out extended treatment without considering all aspects of the patient’s care and without discussing options with members of the team.82,90
A frequent road block to successful reconstruction and dental rehabilitation of the midface-deficient adolescent with UCLP—especially in those who present with other residual clefting problems (see the section about residual deformities later in this chapter)—is disagreement between clinicians about the indications, the most effective techniques, and the timing of intervention.8,104,123 The surgeon, the orthodontist, the dental and medical team, and the patient and his or her family must first agree about the dental, occlusal, speech, upper airway, and aesthetic objectives; only then can effective treatment go forward.
The advantage of coordinated care was confirmed by the Eurocleft Study, which found a lack of association between high-intensity disjointed treatment and favorable results. In other words, the greater the number of operations and the greater the number of years of orthodontic appliances worn (i.e., heavy burden of care), the worse the outcome.25,108
Treatment Protocol
The orthodontist provides interceptive treatment during the mixed dentition in association with bone grafting and carries out definitive orthodontic treatment in conjunction with orthognathic surgery, when indicated. From the mixed dentition phase, the cleft orthodontist should recognize the patient with UCLP who may require orthognathic surgery.* The institution of extensive camouflage (dental compensatory) treatment is likely to jeopardize periodontal health and lead to late dental relapse. Proceeding with a compromised (camouflage) orthodontic approach should only be entered into with full disclosure to the family and other treating clinicians.
Before orthognathic surgery, a speech pathologist evaluates the patient to characterize VP function and to identify articulation errors that result from the cleft palate jaw deformity and the dental malocclusion (see Chapter 8). A baseline evaluation is important, because VP function may deteriorate after maxillary advancement. A nasoendoscopic guided speech assessment is useful to provide maximum objective data.180 VP closure that is adequate before surgery may become borderline afterward, and VP closure that is borderline may become inadequate. Studies document that only a small percentage of patients require a primary pharyngeal flap or flap revision after maxillary advancement.19,20,57,60,79,86,91,95,102,125,170,180 Articulatory distortions that result from malocclusion are also identified and cause-and-effect relationships are determined. The successful orthodontic and surgical correction of crossbites, open bite, cleft–dental gaps, negative overjet, and residual oronasal fistulas represents the most effective way to correct the identified articulation distortions (see Chapter 8). Unfortunately, the use of “oral–motor therapy” is still often applied to manage both jaw-deformity–related articulation errors and VP insufficiency; however, this type of treatment has not been proven beneficial for dynamic speech.
A thorough evaluation of the upper airway is conducted to assess for areas of obstruction (see Chapter 10). Studies suggest an increased prevalence of sleep-disordered breathing and obstructive sleep apnea in patients with cleft palate, especially in the presence of Robin sequence. A formal sleep study (i.e., an attended polysomnogram) is performed if there is a suggestion of obstructive sleep apnea (see Chapter 26). If indicated, simultaneous intranasal procedures (e.g., septoplasty; reduction of the inferior turbinates; recontouring of the nasal apertures, the floor of the nose, and the anterior nasal spine) should be carried out at the time of orthognathic surgery (see Chapters 10 and 15).150
Timing of Orthognathic Surgery
Definitive correction of the jaw deformity is best carried out when the skeleton is mature and before the patient finishes high school.82,90 Maxillofacial growth is generally complete between the ages of 14 and 16 years in girls and 16 and 18 years in boys. However, skeletal growth is variable and may be further gauged by an analysis of sequential lateral cephalometric radiographs taken at 6-month intervals (see Chapter 17). The patient’s and the family’s preferences for the timing of the operation on the basis of psychosocial and functional needs are also taken into account.
As early as 1986, investigators showed that, if maxillary advancement is performed during the mixed dentition in a patient with a cleft palate, then another orthognathic procedure will be necessary for definitive correction after skeletal maturity is reached.181–184 All research to date indicates that a Le Fort I osteotomy carried out during the mixed dentition in a patient with clefting—whether with standard or distraction osteogenesis (DO) techniques—results in no further horizontal maxillary growth (see the controversies section later in this chapter).21,41,40,75
Residual Deformities in the Adolescent with Unilateral Cleft Lip and Palate
Correction of the residual skeletal, soft-tissue, and dental deformities in the adolescent patient with UCLP challenges the ingenuity and skill of the orthognathic surgeon and the cleft team. The central deformity is maxillary hypoplasia (Figs. 32-7, 32-8, and 32-9), and it is frequently combined with residual oronasal fistula, bone defects, intranasal obstruction, soft-tissue scarring, and, occasionally, VP dysfunction (Figs. 32-10 through 32-21).84,167 In addition, the maxillary lateral incisor at the cleft site is usually congenitally absent or deficient, thereby resulting in a cleft–dental gap. Secondary deformities of the nose, the mandible, and the chin region are also common.
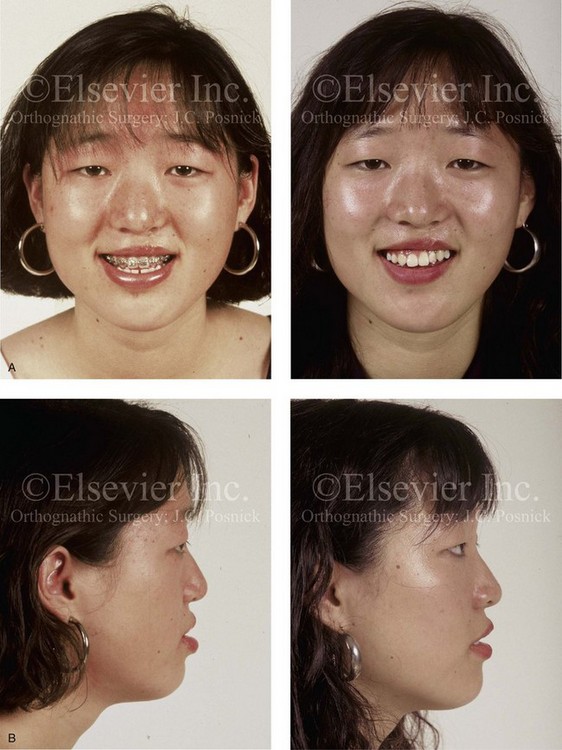
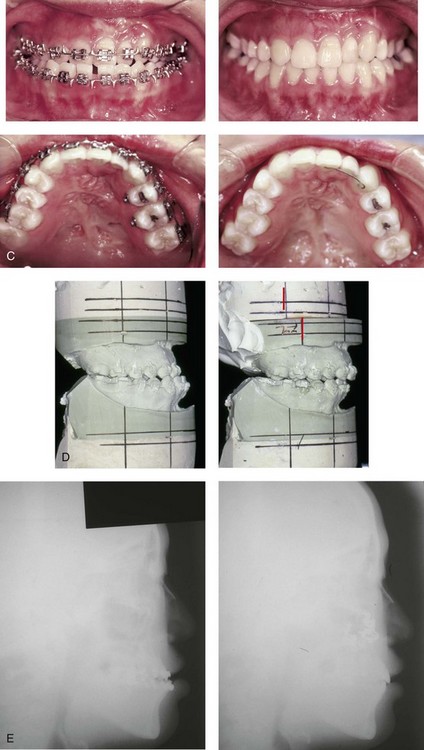
Figure 32-7 A 19-year-old woman was born with UCLP on the left side and underwent lip and palate repair followed by effective bone grafting and fistula closure during the mixed dentition. She has a useful lateral incisor at the cleft site but is missing the lateral incisor on the non-clefted side. A bicuspid has also been removed on the cleft side. As a teenager, she was referred to this surgeon and underwent a combined orthodontic and orthognathic surgical approach. The procedure included a standard Le Fort I osteotomy (horizontal advancement, vertical lengthening) and interpositional grafting. A, Frontal views with smile before and after reconstruction. B, Profile views before and after reconstruction. C, Occlusal and palatal views before and after reconstruction. D, Articulated dental casts that indicate analytic model planning. E, Lateral cephalometric radiographs before and after reconstruction. Note that, by limiting surgery to the maxilla, the cant (which also involved the mandible) cannot be corrected.

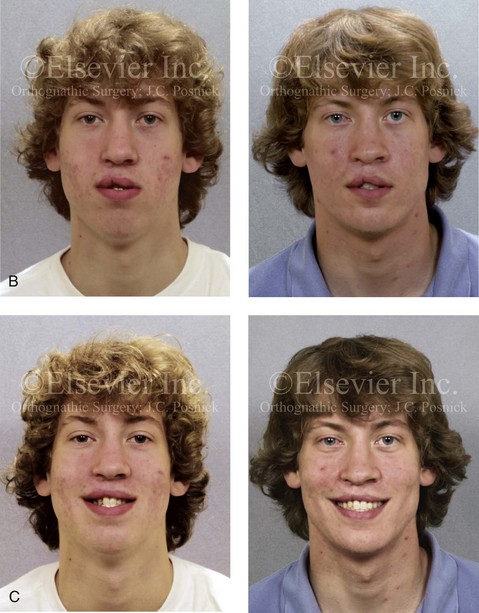

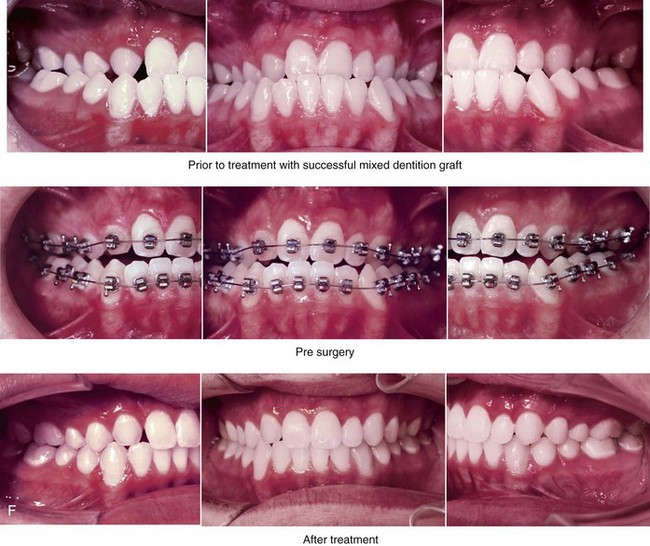
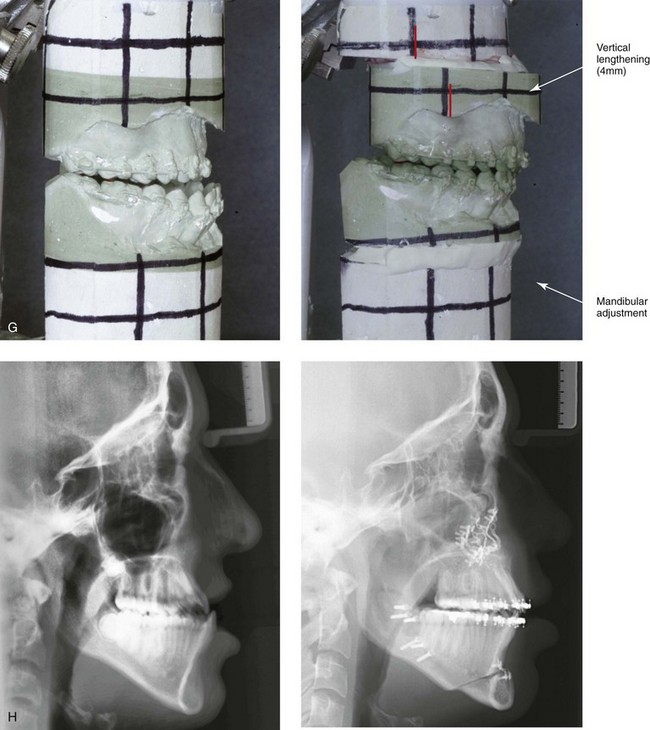
Figure 32-8 A 20-year-old man was born with UCLP on the right side. Primary lip and palate repair were carried out at another institution. He was referred to this surgeon and underwent successful bone grafting and fistula closure during the mixed dentition. He underwent orthodontic closure of the cleft–dental gap and limited alignment by the time he was 14 years old. Final orthodontic decompensation was later carried out in combination with orthognathic surgery when he was 19 years old. The patient’s procedures included maxillary Le Fort I osteotomy (horizontal advancement, vertical shortening, midline correction, cant correction, and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (counterclockwise rotation and asymmetry correction); osseous genioplasty (horizontal advancement); and septoplasty, inferior turbinate reduction, and recontouring of the floor of the nose. A, The patient is shown during the mixed dentition after successful bone grafting and fistula closure. B, Frontal views in repose before and after reconstruction. C, Frontal views with smile before and after reconstruction. D, Oblique facial views before and after reconstruction. E, Profile views before and after reconstruction. F, Occlusal views before definitive orthodontics, with decompensation in progress before surgery, and after reconstruction. G, Articulated dental casts that indicate analytic model planning. H, Lateral cephalometric radiographs before and after reconstruction.

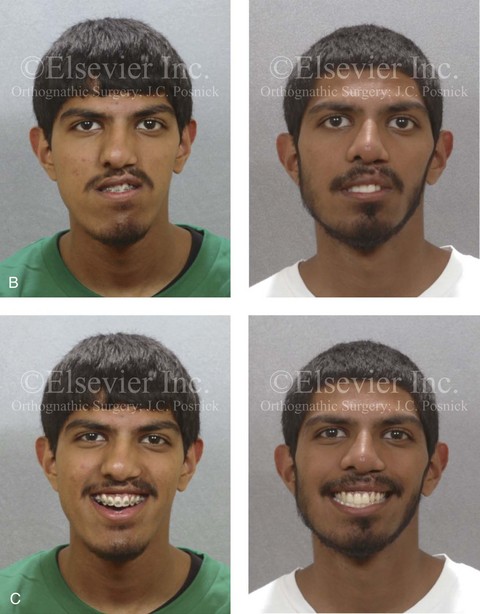
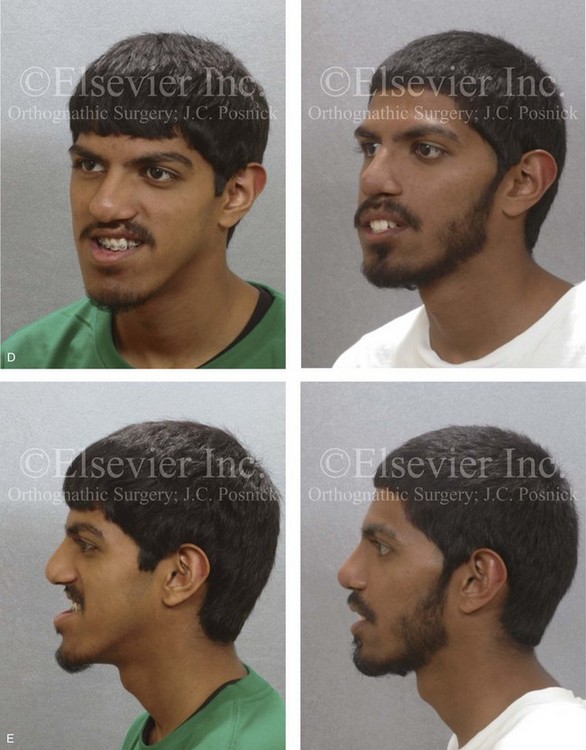
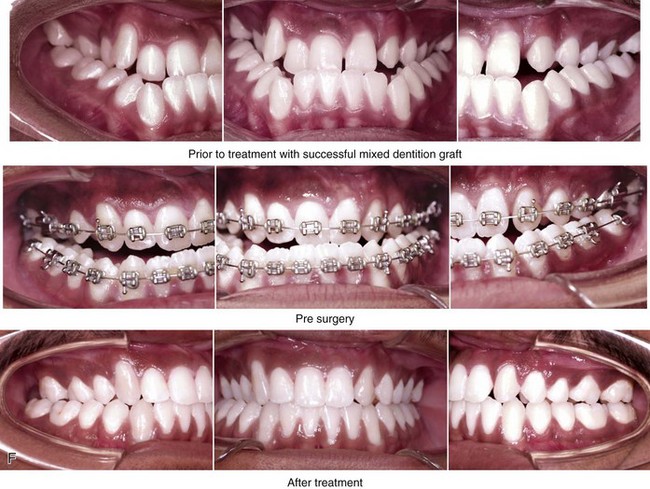
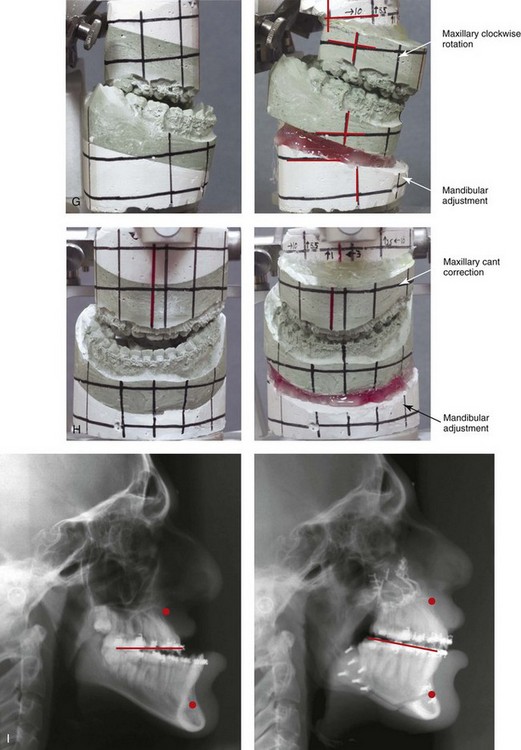
Figure 32-9 A high school senior was born with a complete UCLP on the left side. He underwent lip and palate repair at another institution. He was then referred to this surgeon and underwent successful bone grafting and fistula closure during the mixed dentition. He developed a jaw deformity that was characterized by maxillary deficiency and secondary deformities of the mandible and the intranasal cavity. He underwent a combined orthodontic and surgical approach. Orthodontic decompensation included cleft–dental gap closure (absent lateral incisor). He then underwent jaw reconstruction. The patient’s procedures included maxillary Le Fort I osteotomy (horizontal advancement, vertical shortening, midline correction, cant correction, and clockwise rotation) with interpositional grafting; sagittal split ramus osteotomies (clockwise rotation and asymmetry correction); osseous genioplasty (vertical shortening); and septoplasty, inferior turbinate reduction, and recontouring of the floor of the nose. Six months after successful orthognathic surgery, the patient underwent cleft rhinoplasty including rib cartilage (caudal strut) grafting. A, The patient is shown during the mixed dentition before bone grafting and fistula closure. B, Frontal views in repose before and after reconstruction. C, Frontal views with smile before and after reconstruction. D, Oblique facial views before and after reconstruction. E, Profile views before and after reconstruction. F, Occlusal views before definitive orthodontics, with orthodontic dental decompensation in progress, and after reconstruction. G & H, Articulated dental casts that indicate analytic model planning. Note that, with the clockwise rotation of the mandible, the pogonion moves posterior while the incisors do not. I, Lateral cephalometric radiographs before and after reconstruction.
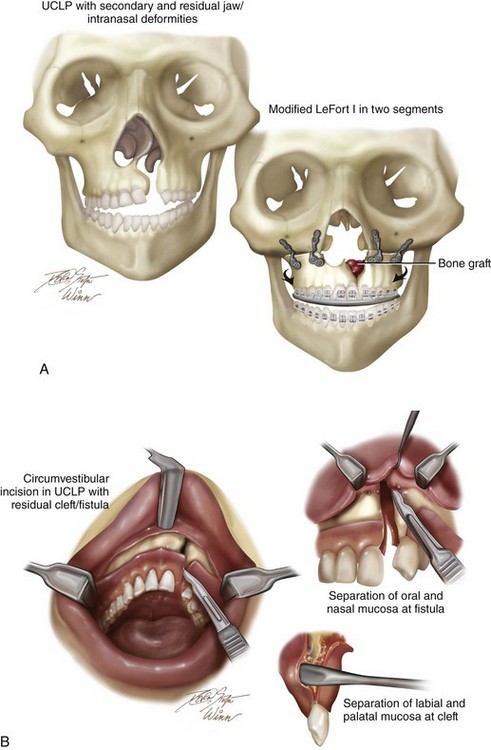
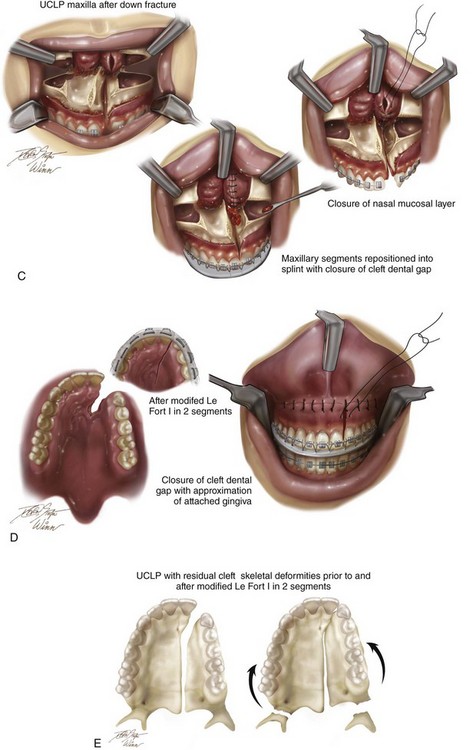
Figure 32-10 Illustrations of modified Le Fort I osteotomy in two segments as carried out in a patient with UCLP who did not undergo successful grafting during the mixed dentition and who presents as an adult with a jaw deformity. A, Frontal view of maxillofacial skeleton before and after Le Fort I osteotomy in two segments. The inferior turbinates have been reduced, and a submucous resection of the deviated septum has been performed. The nasal floor and the nasal spine have been recontoured with a rotary drill. Cancellous iliac bone graft has also been placed along the cleft nasal floor. Corticocancellous iliac graft will also be placed in gaps along the anterior maxilla on each side. B, Circumvestibular and perifistular incisions for exposure to complete osteotomies for down-fracture and later fistula closure. C, Down-fractured Le Fort I osteotomy in two segments after the submucosal resection of the septum, the reduction of the inferior turbinates through the nasal mucosa opening, and then watertight nasal-side closure. D, Wound closure of both the labial and palatal aspects after differential segmental repositioning. E, Palatal view of bony segments before and after repositioning. Parts A-E modified from an original illustration by Bill Winn.



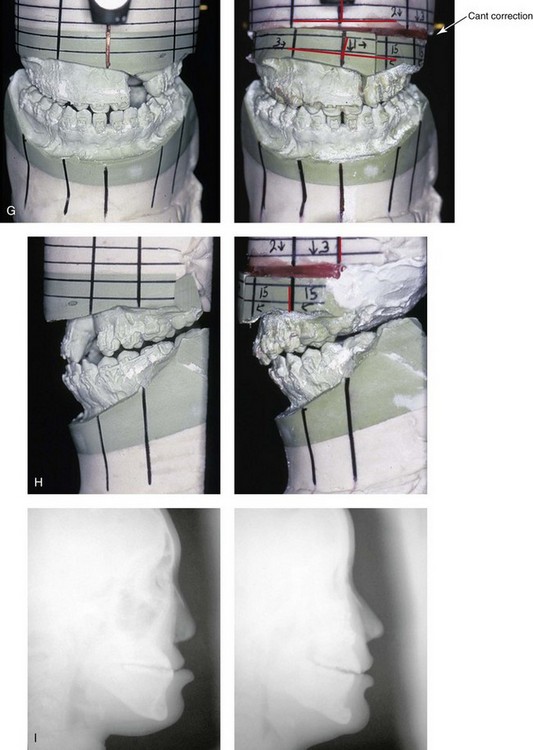
Figure 32-11 A 17-year-old girl who was born with UCLP. She underwent lip and palate repair during childhood, but she did not undergo effective bone grafting during the mixed dentition. A useful lateral incisor is not present at the cleft site. She was referred to this surgeon and underwent a comprehensive orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) with interpositional grafting as well as closure of the oronasal fistula, the cleft–dental gap, and the alveolar defect; an osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, nasal floor recontouring. A, Frontal views with smile before and after reconstruction. B, Oblique views before and after reconstruction. C, Profile views before and after reconstruction. D, Worm’s-eye views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Palatal views with orthodontics in progress and after reconstruction. Note: The maxillary dentition is reconstructed with only eleven teeth. This provides a low maintenance dentition for the patient going forward. G and H, Views of articulated dental casts that indicate analytic model planning. I, Lateral cephalometric radiographs before and after reconstruction. A, E (top Center), E (bottom center), F, From Posnick JC, Tompson B: Modification of the maxillary Le Fort I osteotomy in cleft–orthognathic surgery: the unilateral cleft lip and palate deformity, J Oral Maxillofac Surg 50:666-675, 1992.
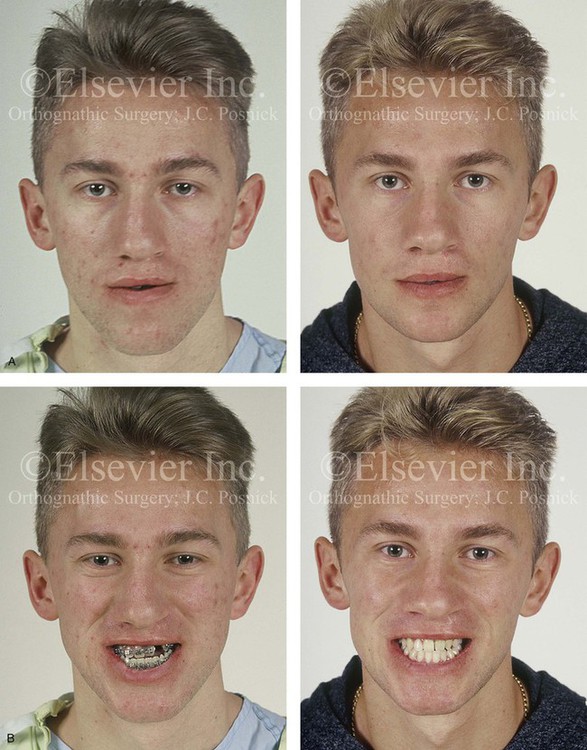

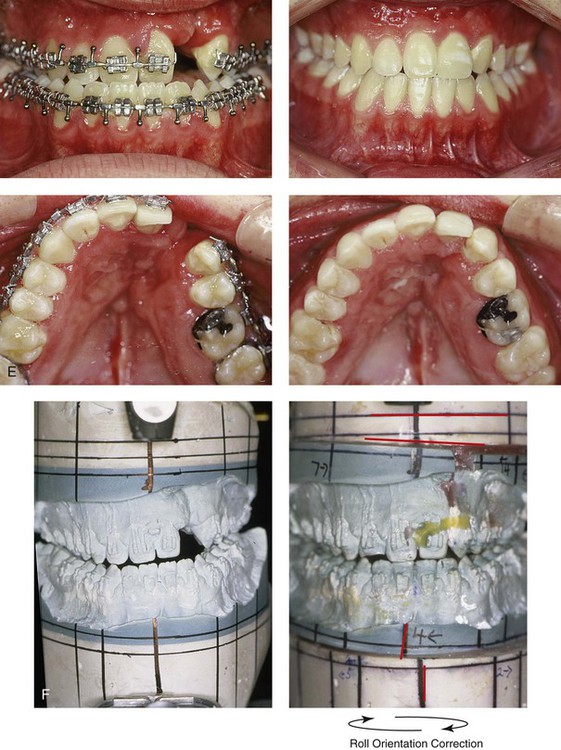
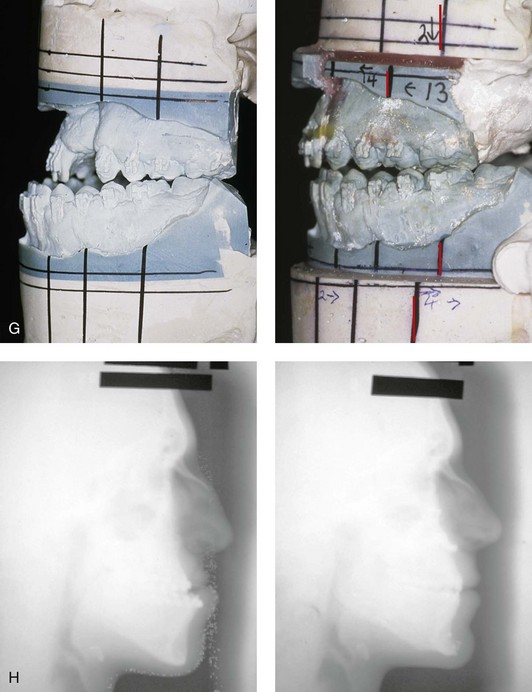
Figure 32-12 A 19-year-old man who was born with UCLP. He underwent lip and palate repair during childhood, but he did not undergo effective bone grafting during the mixed dentition. A useful lateral incisor is not present at the cleft site. He was referred to this surgeon and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) with interpositional grafting, the correction of occlusal canting, and the closure of the oronasal fistula, the alveolar defect, and the cleft–dental gap; bilateral sagittal ramus osteotomies (correction of asymmetry); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal and palatal views with orthodontics in progress and after reconstruction. F and G, Articulated dental casts that indicate analytic model planning. H, Lateral cephalometric radiographs before and after reconstruction. B, D, E, From Posnick JC, Tompson B: Modification of the maxillary Le Fort I osteotomy in cleft–orthognathic surgery: the unilateral cleft lip and palate deformity, J Oral Maxillofac Surg 50:666-675, 1992.
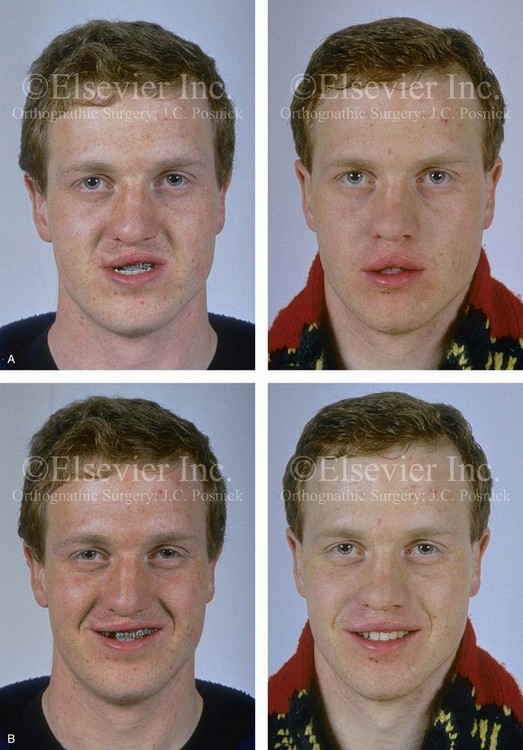
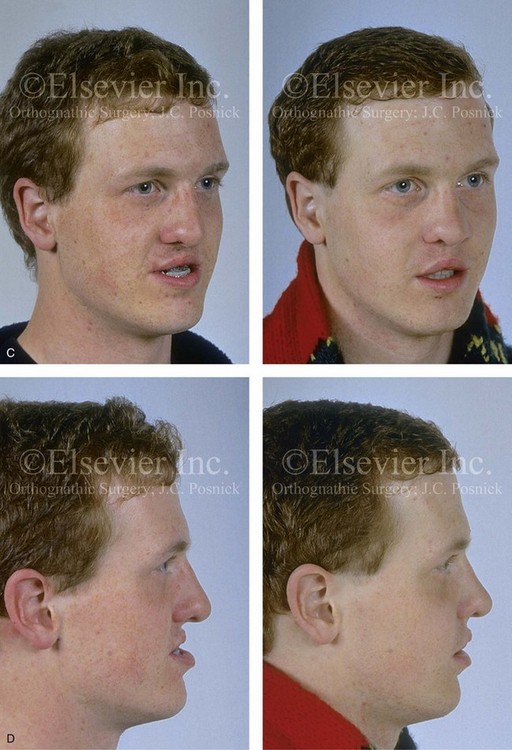
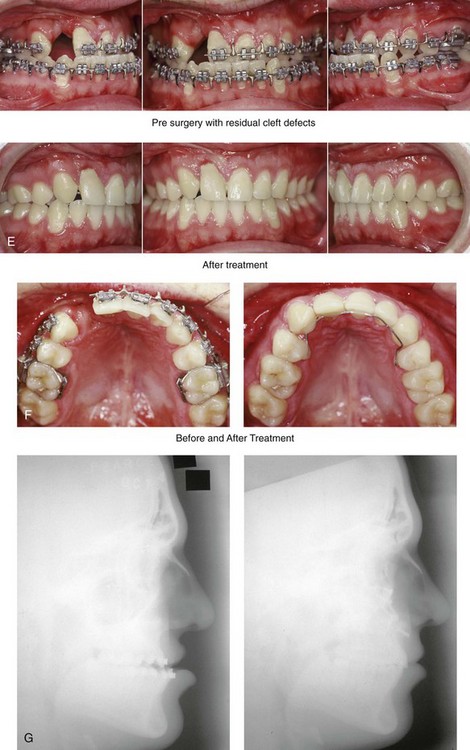
Figure 32-13 A 17-year-old boy who was born with UCLP. He underwent lip and palate repair during childhood, but he did not undergo effective bone grafting during the mixed dentition. The lateral incisor is not present at the cleft site. He was referred to this surgeon as a teenager and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) with interpositional grafting and closure of the oronasal fistula, the alveolar defect, and the cleft–dental gap; and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Palatal views with orthodontics in progress and after reconstruction. G, Lateral cephalometric radiographs before and after reconstruction. B, D, E, F, From Posnick JC, Dagys AP: Skeletal stability and relapse patterns after Le Fort I maxillary osteotomy fixed with miniplates: the unilateral cleft lip and palate deformity, Plast Reconstr Surg 94:924-932, 1994.
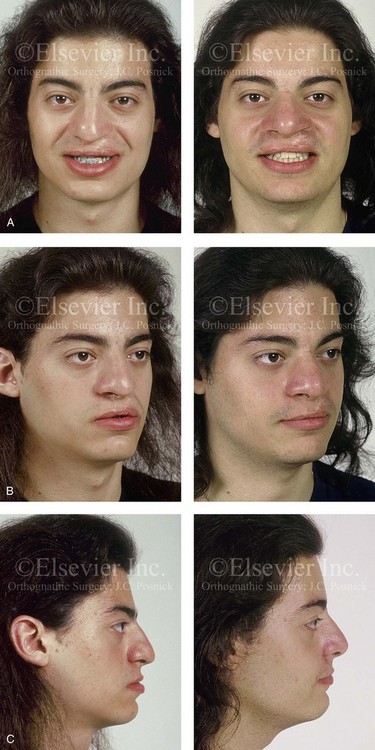

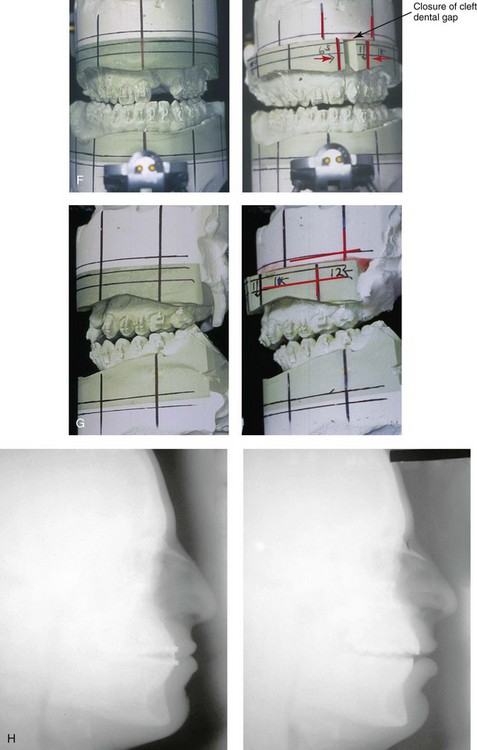
Figure 32-14 A 20-year-old man who was born with UCLP on the left side. He underwent lip and palate repair during childhood, but he did not undergo effective bone grafting during the mixed dentition. A useful lateral incisor is not present at the cleft site. He has a retained primary molar and an absent lateral incisor on the non-cleft side. He was referred to this surgeon as a young adult and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) with interpositional grafting and closure of the oronasal fistula, the alveolar defect, and the cleft–dental gap; and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views with smile before and after reconstruction. B, Oblique views before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views with orthodontics in progress and after reconstruction. E, Palatal views with orthodontics in progress and after reconstruction. F and G, Articulated dental casts that indicate analytic model planning. H, Lateral cephalometric radiographs before and after reconstruction. A, C, D, F, From Posnick JC, Dagys AP: Skeletal stability and relapse patterns after Le Fort I maxillary osteotomy fixed with miniplates: the unilateral cleft lip and palate deformity, Plast Reconstr Surg 94:924-932, 1994.


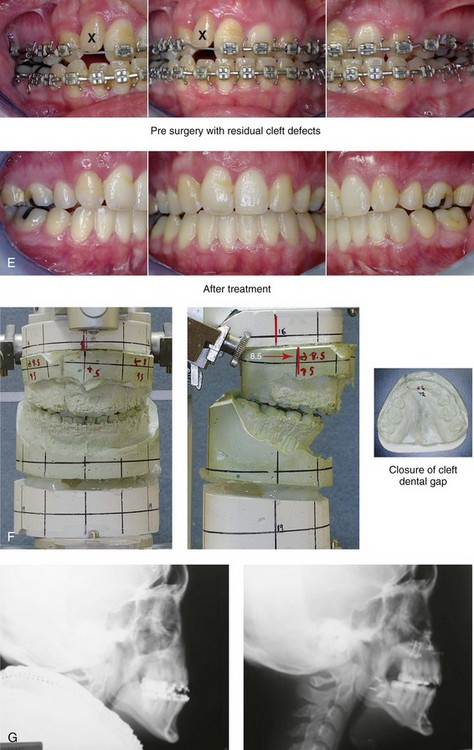
Figure 32-15 A 24-year-old schoolteacher who was born with UCLP. She underwent 4 bicuspid extractions as part of earlier orthodontic treatment. The retained lateral incisor at the cleft does not have an adequate root and required extraction. She was referred to this surgeon as an adult and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) and closure of the oronasal fistula, the alveolar cleft, and the cleft–dental gap; bilateral sagittal split ramus osteotomies; osseous genioplasty; and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction and dental rehabilitation. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction.
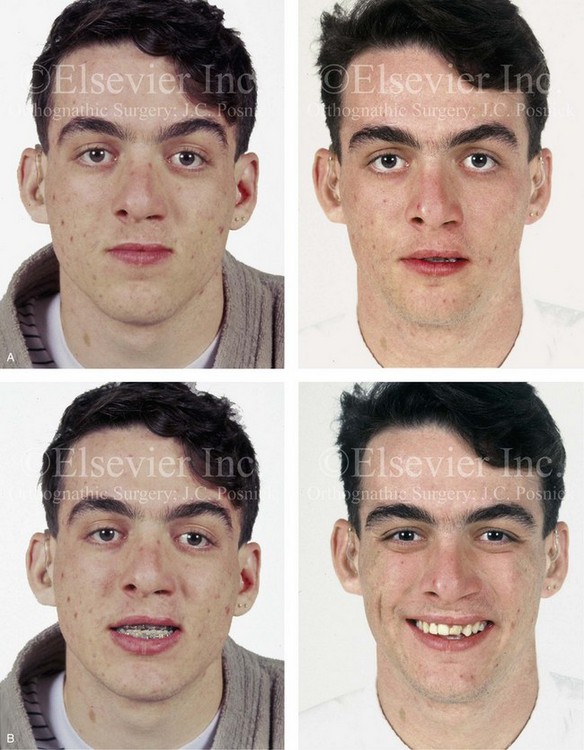


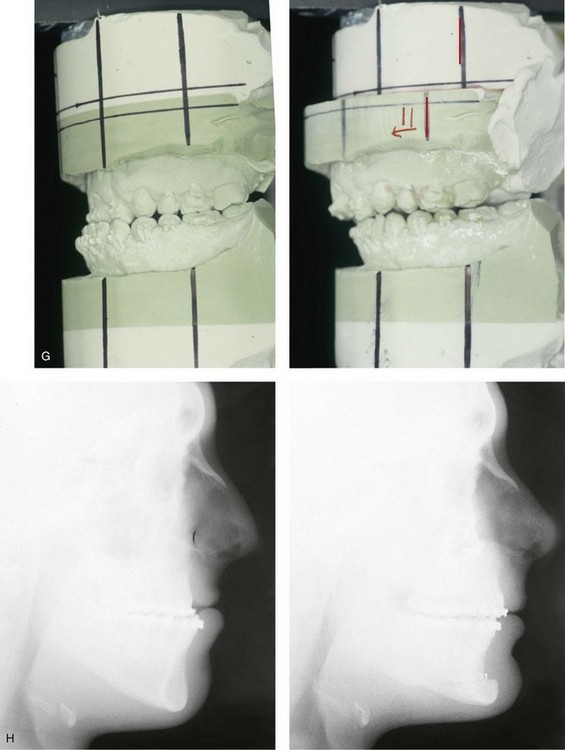
Figure 32-16 A 17-year-old boy who was born with UCLP. He was referred to this surgeon during the late mixed dentition and underwent effective bone grafting. He was congenitally missing his lateral incisor at the cleft site. There is transposition of the canine and the first bicuspids on each side of the upper jaw. He underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a standard Le Fort I osteotomy (horizontal advancement) with interpositional grafting; osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Palatal views with orthodontics in progress and after reconstruction. G, Articulated dental casts that indicate analytic model planning. H, Lateral cephalometric radiographs before and after reconstruction. Note that cosmetic recontouring and modification of the maxillary dental crowns would be beneficial.

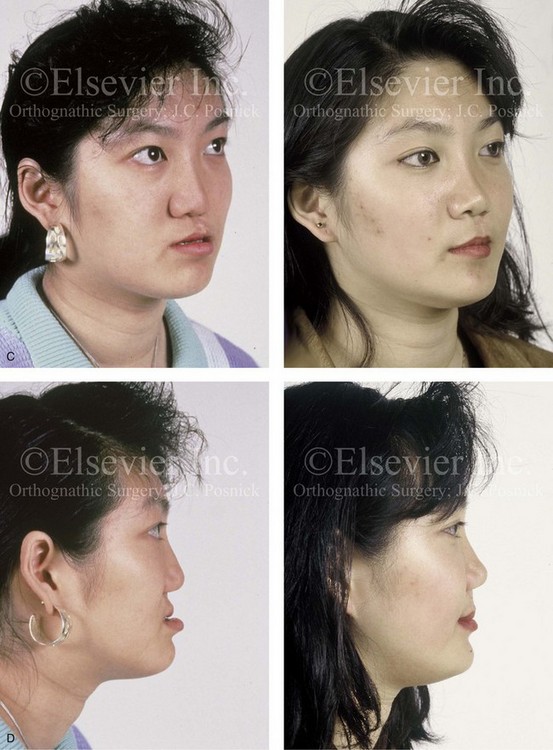

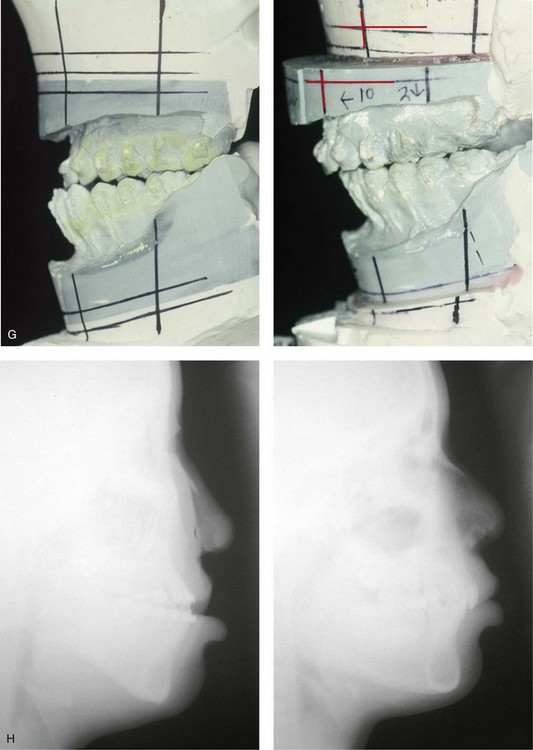
Figure 32-17 A 16-year-old girl who was born with UCLP. She was referred to this surgeon and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) and the closure of the oronasal fistula, the alveolar defect, and the cleft–dental gap; and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A and B, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C and D, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontics in progress and after reconstruction. F, Palatal views with orthodontics in progress and after reconstruction. G, Articulated dental casts that indicate analytic model planning. H, Lateral cephalometric radiographs before and after reconstruction. From Posnick JC: Orthognathic surgery in the cleft patient. In Russell RC, ed: Instructional courses, Plastic Surgery Educational Foundation, vol 4, St. Louis, Mo, 1991, Mosby–Year Book, p 129.


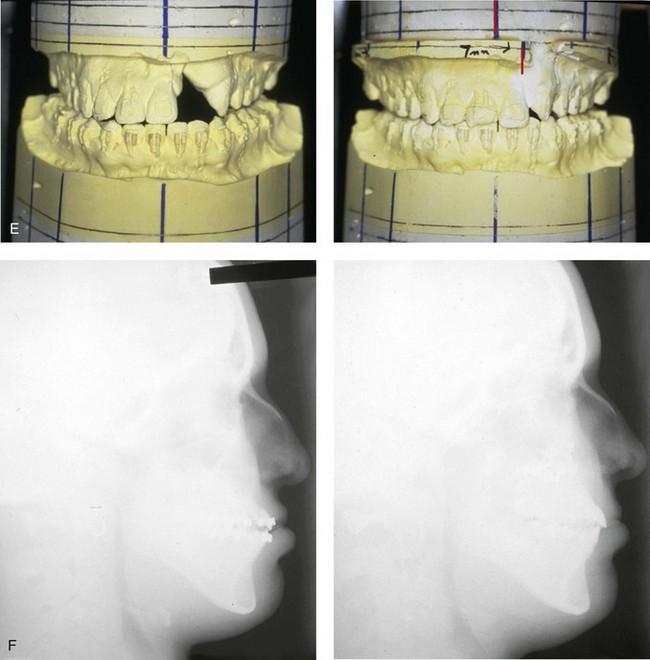
Figure 32-18 A 24-year-old woman who was born with UCLP. She did not undergo bone grafts in the mixed dentition. She is missing the lateral incisor on the cleft side. She was referred to this surgeon as an adult and underwent a combined orthodontic and orthognathic surgical approach. The patient’s procedures included a modified Le Fort I osteotomy in two segments (differential repositioning of the segments) and closure of oronasal fistula, the alveolar cleft, and the cleft–dental gap; bilateral sagittal split ramus osteotomies; osseous genioplasty; and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views with smile before and after reconstruction. B, Profile views before and after reconstruction. C, Occlusal views with orthodontics in progress and after reconstruction and dental rehabilitation. D, Palatal views before and after reconstruction. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction. Note that the palatal fistula was successfully closed. Cosmetic modification of the maxillary anterior teeth was recommended.

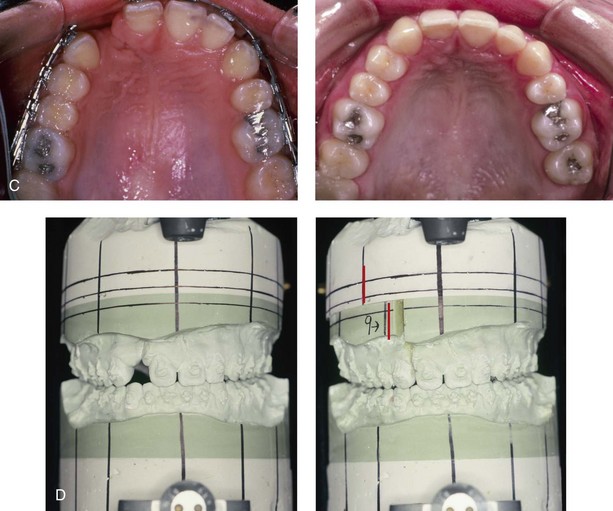
Figure 32-19 A 17-year-old girl who was born with UCLP. She did not undergo successful bone grafting in the mixed dentition. She is missing the lateral incisor on the cleft side. The first bicuspid was extracted on the non-cleft side. She was referred to this surgeon as a teenager and underwent a combined orthodontic and orthognathic surgical approach. The maxilla had good horizontal projection and vertical height. Of the options available to manage the residual upper dentoalveolar needs, a right posterior segmental osteotomy was completed to close the oronasal fistula, the alveolar defect, and the cleft–dental gap. A, Frontal views with smile before and after reconstruction. B, Occlusal views with orthodontics in progress and after reconstruction. C, Palatal views with orthodontics in progress and after reconstruction. D, Articulated dental casts that indicate analytic model planning.
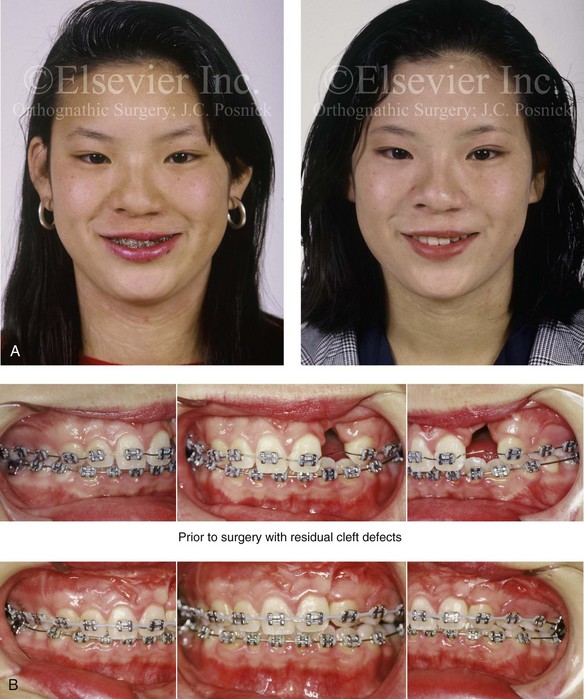

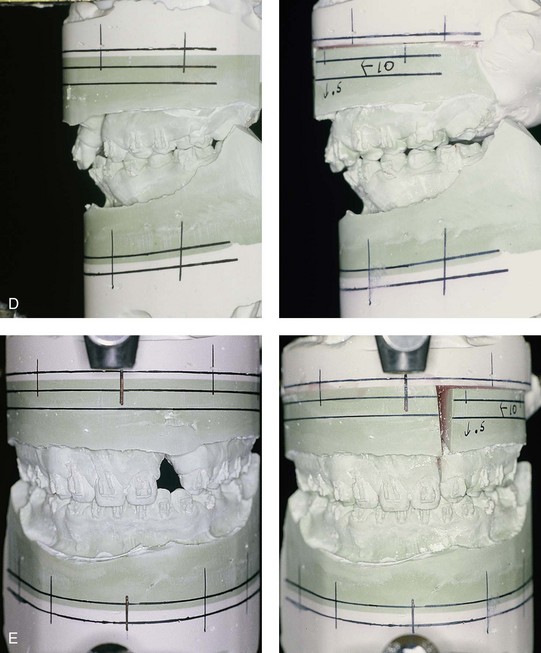
Figure 32-20 A 17-year-old girl who was born with UCLP. She underwent lip and palate repair during childhood, but she did not undergo effective bone grafting during the mixed dentition. The lateral incisor is not present at the cleft site. She was referred to this surgeon and underwent a combined orthodontic and orthognathic surgical approach. The maxilla had good horizontal projection and vertical height. Of the options available to manage the residual upper dentoalveolar needs, a right posterior segmental osteotomy was completed to close the oronasal fistula, the alveolar defect, and the cleft–dental gap. A, Frontal views with smile before and after reconstruction. B, Occlusal views with orthodontics in progress and after reconstruction. C, Palatal views with orthodontics in progress and after reconstruction. D and E, Articulated dental casts that indicate analytic model planning.
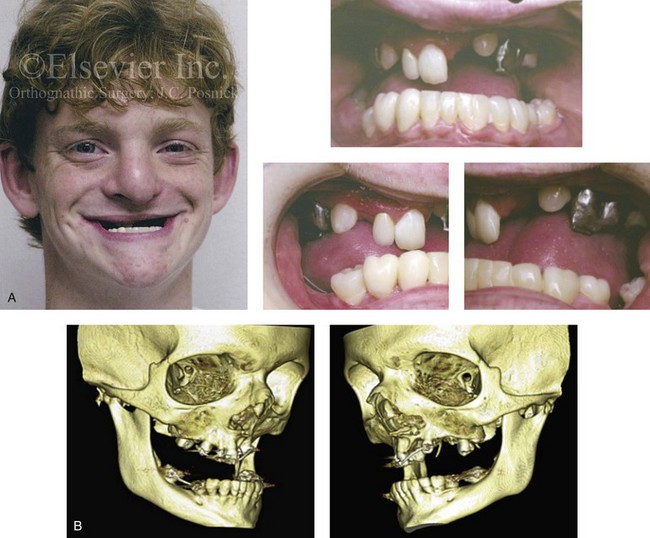
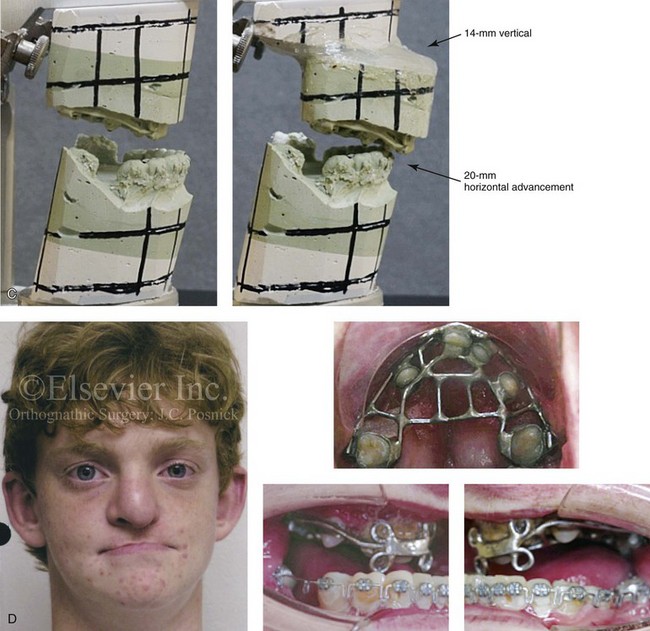
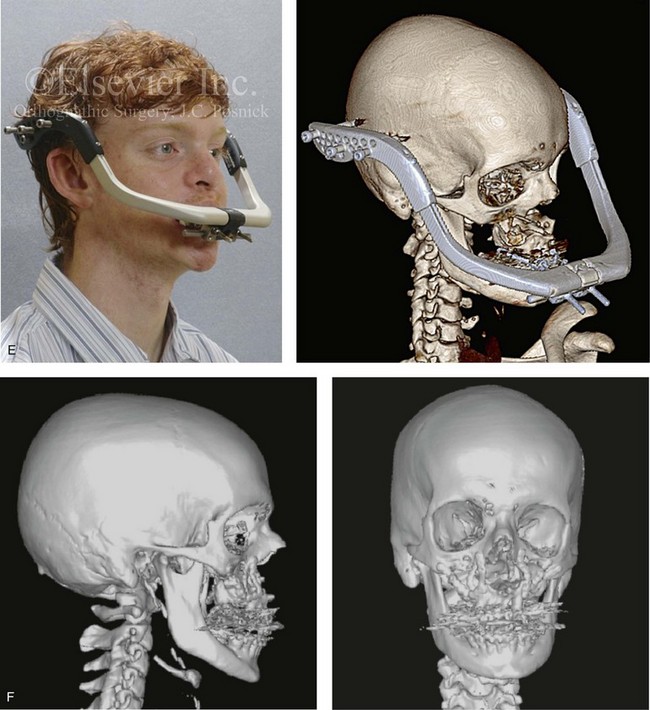
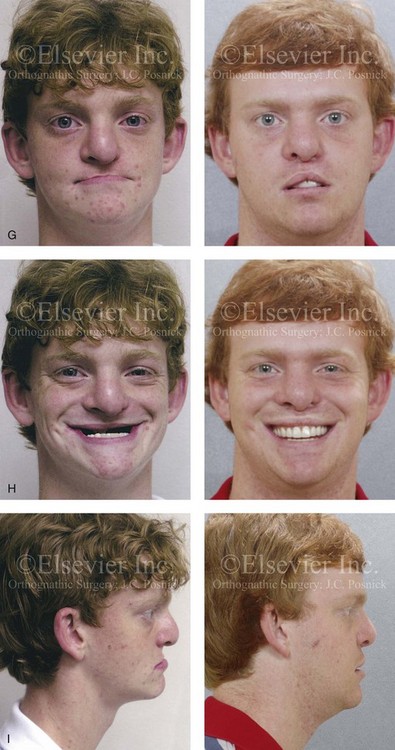
Figure 32-21 A teenage boy who was born with ectodermal dysplasia and complete UCLP on the left side. He underwent lip and palate closure during infancy. There are multiple congenital missing teeth in each arch. He was referred to this surgeon for evaluation when he was 14 years old. He retains only six long-term useful teeth in the maxilla (first and second molars) and displaced left and right canines. The maxilla is vertically and horizontally deficient. The mandible has satisfactory symmetry and horizontal projection. The patient underwent evaluations by specialists, including an orthodontist, a prosthodontist, a periodontist, a surgeon, a speech pathologist, an otolaryngologist, and a geneticist. Reconstruction and dental rehabilitation were felt to require the surgical repositioning of the maxilla followed by an overdenture. In the mandible, crown and bridge rehabilitation would be carried out. The prosthodontist requested 18 mm of horizontal advancement and 14 mm of vertical lengthening of the maxilla. A two-stage approach to maxillary reconstruction was undertaken.
Stage I surgery included the following: 1) nasotracheal intubation; 2) Le Fort I osteotomy with down fracture and disimpaction; 3) septoplasty and inferior turbinate reduction; 4) application of a MED I external distraction device; and 5) securing of the MED I device to a prefabricated in-place chrome cobalt appliance fixed to the maxillary dentition. Successful outpatient distraction of the maxilla to the preferred position was accomplished over a 10-day time frame.
Stage II surgery involved the patient’s return to the operating room for the following: 1) awake fiber-optic nasotracheal intubation; 2) removal of the MED I device; 3) harvesting of the anterior iliac corticocancellous graft; 4) re/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


