Chapter 30 Posterior Single-Tooth Replacement: Surgical Guidelines
Seventy percent of the dentate U.S. population is missing at least one tooth. Compared with past generations, single-tooth replacement will most likely comprise a larger percentage of prosthetic dentistry in the future. In 1960 the average American older than age 55 had just seven original teeth. Today the average 65 year old has 18 teeth, whereas the baby boomers can expect to have at least 24 teeth left when they reach age 65. Currently the first teeth lost are usually between the ages of 35 and 54 years. Almost 30% of the 50 to 59 year olds examined in a U.S. national survey exhibited either single or multiple posterior edentulous spaces bordered by natural teeth.1 Treatment to replace single teeth in the posterior regions represents nearly 7% of the annual dental care reimbursement from insurance companies, and total estimated treatment costs for all patients missing a posterior tooth approximate $10 billion U.S. each year.2,3
POSTERIOR MISSING TOOTH
The first molars are the first permanent teeth to erupt in the mouth and are often the first to decay. The adult patient typically has had one or more crowns fabricated to restore the integrity of the tooth and replace previous large restorations. Longevity reports of crowns have yielded very disparate results, with the mean life span at failure reported to be 10.3 years. The primary cause of failure of the crown is endodontic therapy, porcelain or tooth fracture, or uncemented restoration, which leads to decay. The posterior tooth is at risk for extraction as a result of these complications.1–9 Replacement of the posterior tooth is frequently necessary, and at least one of the adjacent natural teeth are virgin or minimally restored more than 80% of the time. Therefore, a traditional three-unit fixed partial denture to replace a single tooth would remove the enamel on a completely healthy tooth and begin a cascade of potential complications, which often leads to loss of the tooth.
SINGLE-TOOTH IMPLANTS
From 1993 to the present, single-tooth implants have become the most predictable method of tooth replacement and therefore the treatment of choice. There are more refereed reports in the literature than for any other tooth replacement method. Becker et al. reported a more than 90% success rate in a study over 4 years of 282 molar implants.10,11 Simon et al. followed 70 molar implants over a period ranging from 6 months to 10 years with a 97.1% success rate.12 Levin et al. reported in 2006 on single-molar replacement with implants from 6 to 125 months (>10 years) with a 93.6% success rate.13
A 10-year report by Priest indicated the posterior single tooth was more than 97% successful.3 More important, there were no adjacent teeth lost from endodontic failure or causes, and only one tooth required endodontic therapy after implant insertion. This report clearly identifies the adjacent teeth to be least at risk when the missing tooth is replaced with an implant. In a 2007 study, Misch et al. reported a 99% survival rate (11 initial healing failures and three late failures) for 1377 posterior single-tooth implants for as long as 10 years.14 A review of the literature by Goodacre et al. from 1981 to 2003 found single-tooth replacement with an implant had the highest implant prosthesis survival rate and averaged 97% survival.15 The most common complication reported was abutment screw loosening, which did not cause the prosthesis or implant to fail. In a consensus statement, Salinas et al. reported pooled success for single-tooth restorations exceeded the success rate of traditional fixed partial dentures.16
IMPLANT BODY SELECTION
The implant body for a posterior single-tooth implant should include specific features to reduce complications. The most common problem associated with a single tooth is abutment screw loosening.10,11,15,16 The higher the torque used to tighten the screw, the less the risk of loosening. Crest module and abutment connection designs, which decrease forces to the abutment screw, are also indicated. The implant must have an antirotational feature (e.g., an external or internal hex). The greater its height or depth, the less force transmitted to the abutment screw. However, the diameter of the implant is more significant to reduce the stress. Accuracy of component fit, the abutment screw design, and number of threads on the fixation screw are other critical features.
The implant body should be made of titanium alloy to reduce the risk of long-term fracture, as it is four times more resistant to fracture than grade 1 titanium and twice as strong as grade 3 titanium. Sullivan reported a 14% implant fracture rate for single molars fabricated on standard-diameter Nobel Biocare implants (grade 1 titanium) and concluded that this is not a viable treatment.17 A threaded implant provides greater functional surface area than a cylinder, and a tapered implant provides less surface area than a parallel-walled implant body. When implant bodies are internal hex designs, the dimension of the implant in the posterior regions should be at least 4 mm or more in diameter to increase the outer body wall thickness and reduce the risk of long-term body fracture.
The ideal diameter of a single-tooth implant is dependent upon the mesiodistal dimension of the missing tooth and the buccolingual dimension of the implant site. When the facial bone thickness is inferior to 1.4 mm, bone loss may result and implant failures may occur with greater frequency.18 Horizontal bone loss around the implant causes increased probing depths or increased risk of soft tissue shrinkage. These may affect the bacterial flora or cervical esthetics of the soft tissue drape. This may be why gingival recession around wide-diameter implants has been noted to be greater than with a standard diameter.19,20 The ideal implant size is 1.5 to 2 mm from an adjacent tooth and has at least 0.5 mm of bone on the lateral aspects of the implant body. The ideal implant diameter in the intratooth posterior region should be at least 3 mm less than the mesiodistal dimension of the missing tooth (from cement-enamel junction [CEJ] to CEJ) and 3 mm narrower than the buccolingual dimension of bone. As a general rule, the molar implant should be larger in diameter than a premolar implant.
PREMOLAR IMPLANT REPLACEMENT
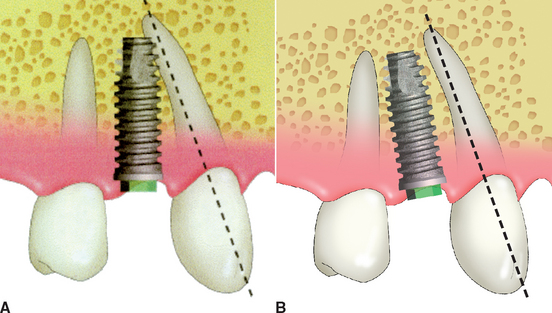
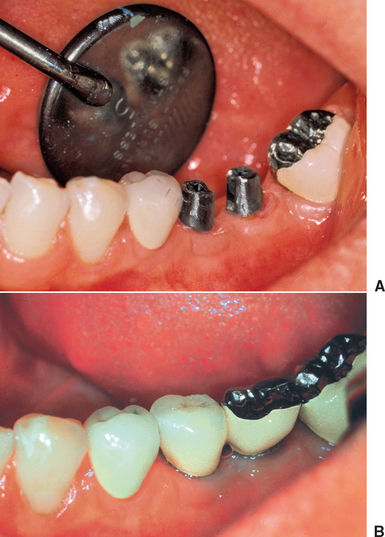
The maxillary canine root is often angled 11 degrees distally and presents a distal curve 32% of the time, which may extend over the shorter root of the maxillary first premolar. The mandibular canine also may have a distal inclination. The implant body is often longer than the natural tooth root of a premolar tooth. The surgeon may inadvertently place the implant parallel to the second premolar and, consequently, into the natural canine root. This may not only result in endodontic therapy of the canine, but also may cause root fracture and loss of the tooth (Figure 30-1, A). Therefore in the first premolar region, care is taken to evaluate the canine angulation. The first premolar implant may need to be placed parallel to the canine root and may need a shorter-than-ideal implant. A tapered implant body at the apical one third also may be of benefit, to further decrease the risk of inadvertently engaging the canine root (Figure 30-1, B).
MOLAR IMPLANT REPLACEMENT
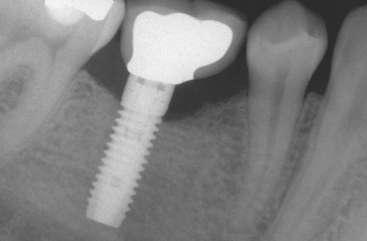
The molar mesiodistal dimension usually ranges from 8 to 12 mm, depending on the original tooth size and the amount of mesial drift of the second molar before implant placement. When one 4-mm-diameter implant is placed to support a crown with a mesiodistal dimension of 12 mm, this may create a 4- to 5-mm cantilever on the marginal ridges. The magnified occlusal forces (especially important in parafunction) may cause abutment screw loosening, an exaggerated emergence profile on the crown, bone loss, and implant body fracture (Figure 30-2).
The most common complication of one regular 4-mm- diameter implant to replace a molar is abutment screw loosening. When the mesiodistal dimension permits, two 3.5- to 4-mm-diameter implants should be considered to restore the region to improve stress reduction and, in turn, reduce the incidence of abutment screw loosening. In a 3-year report of posterior first-molar replacements, Balshi et al.21,22 found implant screw loosening was a common complication when one implant replaced the tooth (48%) and was reduced to 8% when two splinted implants replaced the first molar. Other studies found the one-wide diameter implant had greater screw loosening than two splinted implants.23,24 A 50% decrease in mesiodistal and buccolingual stress was found between a 5-mm and two splinted, standard-diameter implants.24 Therefore, whenever possible, two splinted implants should be used to replace a larger single-molar space.
As mentioned earlier, Sullivan reported a 14% implant fracture rate for single molars on a standard, 4.1-mm implant.17 Rangert et al. reported overload-induced bone resorption appeared to precede implant fracture in a significant number of single-molar implants, which were 4 mm in diameter.25
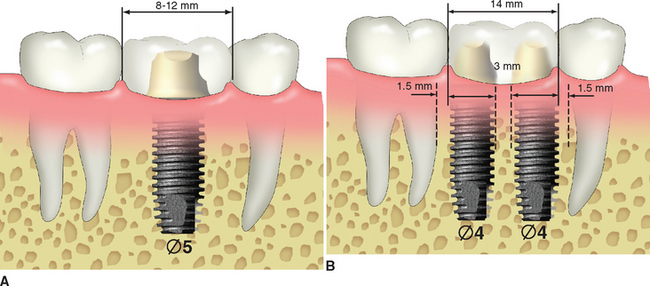
When the mesiodistal dimension of the missing tooth is 8 to 12 mm with a buccolingual width greater than 7 mm, a 5- to 6-mm-diameter implant body is suggested to reduce the stress to the implant system. Langer et al.26 also recommended the use of wide-diameter implants in bone of poor quality or for the immediate replacement of failed implants. The larger- diameter implant does not require as long an implant, which also is a benefit because of the reduced posterior vertical bone height due to anatomical limitations. When possible, a larger diameter implant (or two splinted, traditional-size implants) should be inserted to enhance the mechanical properties of the implant system through increased surface area, stronger resistance to component fracture, increased abutment stability, and enhanced emergence profile for the crown.
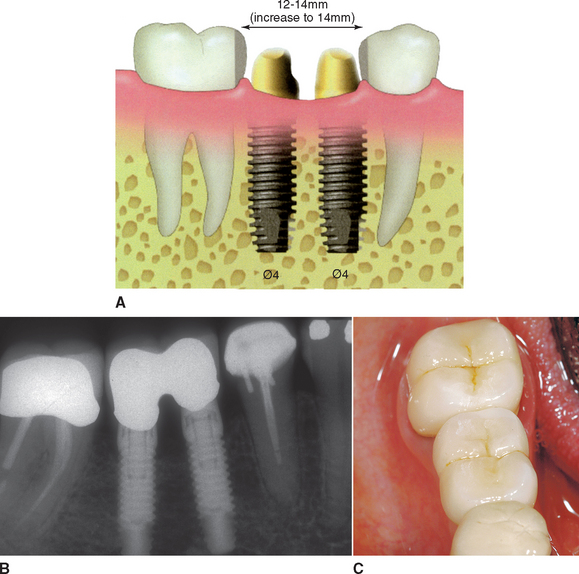
When the posterior space is 14 mm or greater, the largest implant diameter for two adjacent implants may be calculated by subtracting 6 mm (1.5 mm from each tooth and 3 mm between the implants) from the intratooth distance and dividing by 2 (Figure 30-3).
It should be noted the diameter used is the crest module dimension, which is often 0.2 to 0.35 mm greater than the implant body dimension (i.e., 4.1/3.75 mm for Nobel Biocare SteriOss, 3-I, LifeCore). The two implants should be 3 mm apart, because the width of the crestal defect around an implant is usually less than 1.5 mm. The two adjacent implants 3 mm or more apart will not convert the angular defect next to each implant into a horizontal defect, which may increase sulcus depths or cause a loss of papilla height.27 When possible, two regular-size or one regular and one large-diameter implant are suggested when replacing molars. The space is usually restored with two premolar-size crowns, rather than a large molar with a furcation (Figure 30-4).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses