Maxillary Arch Fixed Implant Prostheses
Design and Fabrication
Carl E. Misch
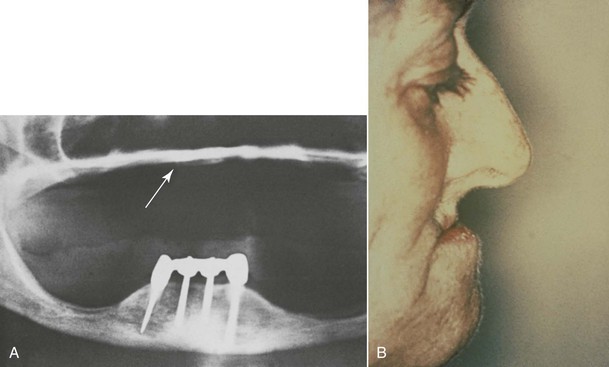
Partially edentulous patients missing multiple maxillary anterior teeth are not unusual. Failed fixed partial dentures often result in additional tooth loss. Car accidents and other sources of trauma may also result in loss of multiple anterior teeth (Figure 30-1). Less often do the effects of periodontal disease affect only anterior teeth. Most partially edentulous patients prefer a fixed prosthesis (FP) to restore their dentition. There are many advantages to restoring multiple anterior missing teeth with a fixed implant restoration independent from the remaining natural teeth.
In addition to partially edentulous patients missing multiple anterior teeth, there are even more patients with completely edentulous maxillae. The average total edentulous rate around the world is 20% of the adult population by age 65 years, although there is wide disparity in the countries with the highest and lowest rates.1 For example, from the 65- to 74-year-old age group, the total edentulous rate in Kenya and Nigeria is 4%, but Netherlands and Iceland have rates of 65.4% and 71.5%, respectively. The edentulous Canadian rate is 47% at age 65 to 69 years and 58% from ages 70 to 98 years (with Quebec at 67% for those older than age 65 years compared with Ontario with a rate of 41%).
A 1999 to 2002 survey found that total edentulism in the United States of both arches was present in almost 20 million people.2 As expected, older persons are more likely to be missing all of their teeth. Total edentulism has been noted in 5% of employed adults ages 40 to 44 years, gradually increasing to 26% at age 65 years and to almost 44% in seniors older than age 75 years.3 Gender was not found to be associated with tooth difference in retention or tooth loss after adjustments were made for age.
The maxillary arch may also be completely edentulous, opposing at least some teeth in the mandible. This condition occurs 35 times more often than the reverse situation. At age 45 years, 11% of the population has maxillary total edentulism opposing at least some teeth, which increases to 15% by 55 years of age and then remains relatively constant.2,3
The percentages of total edentulism of the maxillary arch translate into more than 30 million people or about 17% of the entire U.S. adult population.4 To put these numbers in perspective, 30 million people represent approximately the entire U.S. African American population, the U.S. Hispanic population, the whole population of Canada, or the total population in the United States older than 65 years of age.
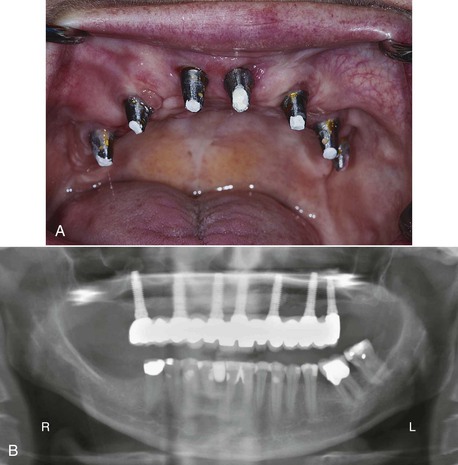
Maxillary dentures usually are tolerated better by completely edentulous patients than their mandibular counterparts. The greater retention, support, and stability compared with a lower restoration are well documented. As such, patients are often able to wear the devices for longer periods of time before complications arise. As such, many treatment plans for complete edentulous patients initially concentrate on the problems associated with the mandibular denture (Figure 30-2). However, when patients enjoy a stable, retentive, and perhaps fixed mandibular prosthesis, often their attention is brought to the maxillary arch. When patients become aware of the anatomical and esthetic consequences of missing teeth, their desires increase for maxillary implant restorations. As a result, future restorations of the edentulous maxilla more often include implant restoration.
Consequences of Anterior Maxillary Edentulism
Several factors affect the condition of the premaxilla and may result in a decrease in implant survival or an increase in prosthetic complications. A completely edentulous anterior bony ridge is often inadequate for endosteal implants. The facial cortical plate is very thin over the maxillary anterior teeth and may be resorbed from periodontal disease or often is fractured during the extraction of teeth (Figure 30-3). In addition, the facial cortical plate resorbs during initial bone remodeling, and the anterior ridge loses 25% of its width within the first year after tooth loss and 40% to 60% over 3 years, mostly at the expense of the labial plate.5,6 As a result, the maxillary denture migrates to a more palatal position in the anterior maxilla.
By the time the patient notices problems of stability and retention caused by lack of premaxilla, the maxillary bone often has resorbed in height and is a division C-h to D (Figure 30-4). When the premaxilla resorbs, the maxillary denture begins to become unstable. The maxillary anterior teeth are positioned in front of the residual bone. As a result, the denture rotates up in the anterior, which means it rotates down in the posterior. The denture loses the valve seal as a consequence. The complete anterior ridge and even the nasal spine may be resorbed in the maxilla, also causing pain and a further increase in maxillary denture movement during function.7,8 Hence, an implant prosthesis should be considered for the maxillary arch before bone is lost in the premaxilla.
The doctor has the responsibility to inform the patient about the continued bone loss of the maxilla. Bone grafting is much more predictable for width gains than increases in height. Division B bone grafting often may use a synthetic bone component for the graft. Division C minus width (C–w) often requires at least some autologous bone, often with the mandible as a donor. With edentulous maxillae requiring height augmentation (division C–h or D), the dentist may have to resort to the iliac crest as a donor site for large volumes of bone.9 As such, the maxillary completely edentulous patient should understand that the surgical rehabilitation is much more complex and extensive because the volume of bone to reconstruct the arch becomes larger. Rather than waiting until the bone is resorbed or the patient complains of problems with the prosthesis, the dental professional should educate the patient about the bone loss process after tooth loss (Box 30-1). The patient should be made aware that the future bone loss can be arrested by a dental implant.
Chapter 25 presents the fixed treatment plan options for edentulous and partially edentulous premaxillae, including the key implant positions and the number and size of the implants. This chapter presents unique conditions of the maxilla that relate to implant number. In addition, this chapter addresses the sequence of treatment to restore the maxillary arch within the esthetic zone.
Advantages of a Maxillary Implant Prosthesis
The use of dental implants to provide support for an implant overdenture (IOD) offers many advantages compared with the use of removable soft tissue–borne restorations. A primary reason to consider dental implants to replace missing teeth is the maintenance of alveolar bone. For example, after the implants are inserted, the bone loss may resorb as little as 0.6 mm vertically over 5 years, and long-term resorption may remain at less than 0.05 mm per year.10
When a maxillary denture is used opposing mandibular teeth or an implant-supported restoration, the maxillary bone loss may be accelerated.11 An endosteal implant can maintain bone width and height as long as the implant remains healthy. As with a tooth, periimplant bone loss may be measured in tenths of a millimeter and may represent a more than 20-fold decrease in lost bone structure compared with the resorption that occurs with RPs.
The features of the inferior third of the face are closely related to the supporting skeleton7 (Figure 30-5). When vertical bone is lost, the dentures only act as “oral wigs” to improve the contours of the face. The dentures become bulkier as the bone resorbs, making it more difficult to control function, stability, and retention. With implant-supported prostheses, the vertical dimension may be restored, similar to natural teeth. In addition, the implant-supported prosthesis allows a cantilever of anterior teeth for ideal soft tissue and lip contour and improved appearance in all facial planes. This happens without the instability that usually occurs when an anterior cantilever is incorporated in a traditional maxillary denture. The facial profile may be enhanced for the long term with implants rather than deteriorating over the years, as can occur with traditional dentures.
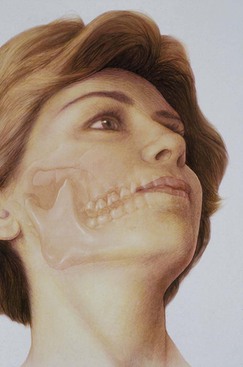
Facial esthetics are affected as a consequence of the maxillary arch with bone loss, with the loss of vermilion border of the lip, increased length of the maxillary lip, and lack of facial bone support. However, patients may not realize these changes are related to the loss of teeth and bone (Figure 30-6).
From a bone volume conservation standpoint in the jaws, completely edentulous patients should be treated with enough implants to completely support a prosthesis whether the patient is partially or completely edentulous. The continued bone loss after tooth loss and associated compromises in esthetics, function, and health make all edentulous patients implant candidates. As a result, complete implant-supported restorations should be the restoration of choice.
The complete denture often moves during mandibular jaw movements during function and speech. The maxillary teeth are often positioned for lower denture stability rather than where natural teeth usually reside. With implants, the maxillary teeth may be positioned to enhance esthetics and phonetics rather than in the neutral zones dictated by traditional denture techniques to improve the stability of a lower prosthesis.
Occlusion is difficult to establish and stabilize with a completely soft tissue–supported prosthesis. Proper occlusal contacts often occur by chance, not by design.12 An implant-supported restoration is stable. The patient can more consistently return to centric relation occlusion rather than adopt variable positions dictated by the prosthesis’ instability.
Proprioception is awareness of a structure in time and place. The receptors in the periodontal membrane of a natural tooth help determine its occlusal position. Although endosteal implants do not have a periodontal membrane, they provide greater occlusal awareness than complete dentures. Implant patients can determine 50-micron differences with rigid implant bridges compared with 100 microns in those with complete dentures (either one or two).13 As a result of improved occlusal awareness, the patient functions in a more consistent range of occlusion.
With an implant-supported prosthesis, the direction of the occlusal loads is controlled by the restoring dentist. Horizontal forces on RPs accelerate bone loss, decrease prosthesis stability, and increase soft tissue abrasions. Therefore, the decrease in horizontal forces that are applied to implant restorations improves the local parameters and helps preserve the underlying soft and hard tissues.
The maximum occlusal force of a traditional denture wearer ranges from 5 to 50 lb. Patients with an implant-supported FP may increase their maximum bite force by 85% within 2 months after the completion of treatment. After 3 years, the mean force may reach more than 300% compared with pretreatment values.14 As a result, an implant prosthesis wearer may demonstrate a force similar to that of a patient with a fixed restoration supported by natural teeth.
Chewing efficiency with an implant-supported prosthesis is greatly improved compared with that of a soft tissue–borne restoration. The masticatory performance of dentures, overdentures, and natural dentition was evaluated by Rissin et al., and the traditional denture showed a 30% decrease in chewing efficiency.15 The tooth-supported overdenture loses only 10% of chewing efficiency compared with natural teeth. An implant-supported prosthesis may function the same as natural teeth.
Retention of an implant-supported prosthesis is a great improvement over soft tissue–borne dentures. Mechanical means of rigid implant retention are far superior to the soft tissue retention provided by dentures or adhesives and cause fewer associated problems.
Patients treated with implant-supported prostheses judge their overall psychological health as improved by 80% compared with their previous state while wearing traditional, removable prosthodontic devices.10 They perceive the implant-supported prosthesis as an integral part of their body.
A FP has less bulk of acrylic compared with a denture or IOD, reducing the bulk of the restoration, especially when the palate is eliminated. A few individuals have taste buds in the palate that are innervated from the eleventh nerve. Although unusual, these patients benefit from the elimination of the palate of their prosthesis. Therefore, eliminating the palate reduces the gagging effect for some patients, improves the taste of food in some individuals, and has an oral sexual advantage to others.
The success rate of implant prostheses varies, depending on a host of factors that change for each patient. However, compared with traditional methods of tooth replacement, a fixed implant prosthesis offers increased longevity, improved function, bone preservation, and better psychological results (Box 30-2).
Fixed Prosthesis versus Overdenture
The maxillary overdenture has several advantages compared with a traditional denture. However, because a maxillary denture has more retention, support, and retention than the mandibular denture, a RP-5 maxillary restoration has less benefit than the RP-5 mandibular restoration. The primary advantage of the RP-5 maxillary IOD is the reduced cost. The reduced fee is not only the reduced implant number (e.g., 4 vs. 7) but usually reduces the need for sinus graft augmentation. Hence, the time for treatment is reduced, as is the surgical fee, and may be less than 50% of the RP-4 or fixed restoration.
A survey by Carlsson et al. in 10 countries indicated a wide range of fixed versus removable options to treat edentulous patients.16 The proportion of IOD selection versus fixed implant dentures was highest in the Netherlands (93%) and lowest in Sweden and Greece (12%). Cost was cited as the number one determining factor in the choice. However, with such a wide range of prosthesis type selection from one country to another, the influence of the doctor presenting the treatment options must be a major factor.
The esthetic advantage of a maxillary overdenture compared with a fixed restoration may be more evident in the maxilla compared with the mandible. The labial position of the maxillary lip for esthetics may require a labial flange, which makes it almost impossible for hygiene access when a fixed restoration is used. As such, when the teeth must be cantilevered off the premaxillary residual ridge more than 7 mm, an overdenture is strongly considered (Figure 30-7).
The IOD may be removed at night to reduce the noxious effects of nocturnal parafunction. These cyclic forces increase the risk of biomechanical problems, not only of the implants but also of the entire implant system, including the prosthesis occlusal material, the screws and cements that retain the prosthesis, the abutment screws, the crestal marginal bone, the complete bone–implant interface, and fracture of any of the prosthetic components or even the implants themselves.
A clinical study by Heydecke et al. evaluated 13 patients who received both a RP-4 overdenture and a FP, both for 2 months each.17 Psychometric evaluation of general satisfaction, comfort, ability to speak, stability, esthetics, ease of oral hygiene, and occlusion was performed for both restorations. The chewing ability with seven types of foods was also determined with both restorations. The general satisfaction rating was significantly higher for the RP-4 overdenture group. The ability to speak and ease of hygiene were better, and the masticatory dynamics were similar in either prosthesis relative to stability, occlusion, and chewing ability. Nine of the 13 patients opted to have the RP-4 overdenture rather than the FP-3 at the conclusion of the study.
On the other hand, Brennan et al. also evaluated patient satisfaction and oral health–related quality of life outcomes of maxillary IODs (RP-5 and RP-4) and fixed complete prostheses.18 Patients with maxillary overdentures reported significantly lower overall satisfaction, with lower scores for both chewing capacity and esthetics. The advantages cited for the overdenture were reduced cost and the ability to perform oral hygiene procedures.
Implant fixed restorations have a psychologic advantage compared with overdenture prostheses. Whereas an overdenture is a prosthesis, a fixed restoration is considered a body part. Patients with an IOD respond, “These are much better than my denture.” When patients have a fixed restoration, they often state, “These are better than my teeth.”
In the author’s experience, patients who desire a fixed restoration are usually those that want the psychologic advantages of fixed teeth or patients who very recently lost their teeth and have not completely accommodated to a removable prosthesis (RP). These patients also most often have anterior bone and do not need the labial support of a denture flange to support the maxillary lip. On the other hand, long-term denture wearers do not perceive the advantages of a fixed restoration enough to compensate for the hygiene benefits. Esthetics may also be the motivating factor for an overdenture when the maxillary lip needs additional support.
A greater crown height space (CHS) is required for an overdenture. Hence, when abundant bone is present and implants are already inserted, a FP will have fewer issues of prosthesis fracture or positioning teeth over a bar.
More prosthetic maintenance is required for an overdenture. Attachments wear and need to be replaced, relines are necessary for RP-5 restorations, and denture teeth wear more rapidly on an IOD than a denture. As a result, a new IOD may need to be fabricated every 7 years.
A side effect of an IOD is food impaction under the prosthesis. The denture is border molded, so the muscles are in their contracted position. Otherwise, because the prosthesis is more rigid than a denture, sore spots develop during function. In the relaxed muscle state, food goes beyond the denture border. When the patient swallows, the food is pushed under the denture. A FP does not extend to peripheral borders and traps less food in comparison.
The advantage of developing a treatment plan for long-term health, rather than short-term gain, is beneficial to the patient. As such, if finances are not an issue, the dentist should design a prosthesis that is completely supported, retained, and stabilized by implants. If cost is a factor, a transitional implant-retained restoration with fewer implants greatly improves the performance of a denture and arrests the bone loss in the premaxilla. Then the dentist may establish a strategy for the next one or two steps to obtain the final complete implant-supported restoration.
Fewer reports have been published for maxillary implant prostheses than for the edentulous mandible.19 The most often reported literature for the edentulous maxilla is similar to the original articles published by Branemark et al.20 In this approach, four to six implants were positioned anterior to the maxillary sinuses, and a cantilever FP was fabricated. Approximately a 10% higher failure rate was observed in the maxilla compared with the mandible.21
Most all reports agree that a greater implant failure and risk of prosthetic complications exists in the maxilla compared with the mandible for full-arch restorations. In addition, maxillary overdentures have a higher failure rate than full-arch fixed restorations. For example, Engquist et al. report a 6% to 7% implant failure for mandibular implant–supported overdentures and a 19% to 35% failure for maxillary IODs.22 Smedberg et al. reported an 86% survival rate for 20 patients with 86 maxillary implants, and results showed a similar disparity of results based on bone volume quality.23 Palmqvist et al. also reported similar results.24 A prospective study by Johns et al. reported on maxillary overdentures over 5 years.25 Sixteen patients were followed throughout the whole study with a cumulative success rate of 78% and 72% for prostheses and implants, respectively. Widborn et al. evaluated 22 patients with 13 planned overdentures compared with FPs that ended up with an overdenture over a mean observation period of 5.7 years.26 The implant survival rate in the planned overdenture group was 77%, and survival rate in the unplanned group was 46%.
Jemt et al. reported an 84% survival rate for 430 maxillary implants on 92 consecutive patients at 1 year.27 In a follow-up study by Jemt of 70 edentulous maxillary patients with 336 implants, there was a 70% survival rate in resorbed bone and 88% in the intermediate group with an 85% implant overall survival rate.28 In a 5-year prospective, multicenter study on 30 maxillae and 103 mandibles, Jemt and Lekholm reported that the survival rates of mandibular implants were 94.5% and 100% for mandibular prostheses.29 In the maxillae, the implant survival rate was 72.4%, and the prosthesis survival rate was 77.9%.
Goodacre et al. performed a literature review from 1981 to 2003.30 The implant prosthesis type with the lowest implant survival was a maxillary overdenture with a 21% failure rate followed by a full-arch maxillary FP with a 10% failure rate. A similar implant survival was reported by Chan et al.31 They combined data from several reports and yielded an average 21% failure rate for implant-supporting maxillary overdentures, the highest failure rate of any prosthesis type. The primary causes of failure were implant overload as a result of decreased bone density, reduced implant size, and reduced implant number.
On the other hand, Sanna et al. reported on splinted implants for maxillary overdentures compared with full dental FPs with no implant failure.32 The author has followed 75 maxillary overdenture (RP-4) patients and 110 full-arch FPs for 10 years with splinted implants and found 97% implant survival and 100% prosthesis survival rates.33 Hence, no difference may be observed between these modalities when enough implants support the prosthesis. The primary differences in these treatment modalities have been implant number, position, and prosthetic guidelines that follow basic biomechanical concepts to reduce failure and decrease risks for maxillary full arch prostheses. In other words, an implant foundation specific for implant position and number.
In conclusion, if an edentulous patient desires a RP, an IOD is often the treatment of choice. If cost is a problem for a patient who desires a fixed restoration, the overdenture may serve as a transitional device until additional implants may be inserted and restored. However, when the patient desires a fixed restoration and the anterior bone is sufficient to support the maxillary lip, a fixed restoration has many advantages (Box 30-3).
Treatment Planning Considerations
An independent, fixed implant-supported restoration has become the treatment of choice for most patients with complete or partial edentulism. A FP presents several advantages over a removable partial denture or an overdenture for a maxillary edentulous patient. However, several criteria should be evaluated, and the treatment sequence should be noted.
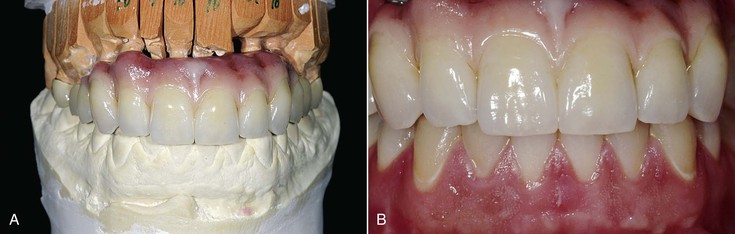
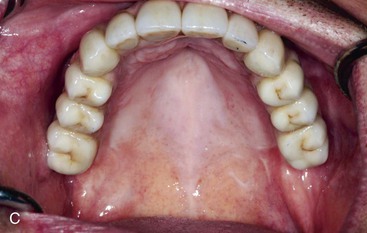
The bone available for implant insertion in esthetic regions should be evaluated because the bone will influence greatly the labial lip support, the soft tissue drape, the implant size, the implant insertion (angulation and depth), and hence the final prosthetic result. Bone loss after maxillary anterior tooth loss is rapid and has considerable consequences. Thereafter, almost all multiple maxillary anterior edentulous sites require at least some bone and soft tissue augmentation before, along with, or at implant uncovery. Even when the bone is restored, the soft tissue drape is usually compromised. The maxillary anterior region with multiple adjacent teeth missing most often is restored with an overdenture or a fixed restoration that replaces teeth and the soft tissue drape (FP-3 prosthesis) (Figure 30-8).
In the majority of patients with available bone, the bone is less dense in the anterior maxilla than in the anterior mandible.34 In the mandible, a dense cortical layer is coupled with coarse trabecular bone strength and permits implants to be supported by a denser bone quality. The maxilla presents thin porous bone on the labial aspect, very thin porous cortical bone in the floor of the nasal region, and a more dense cortical bone on the palatal aspect. The trabecular bone is usually fine and is also less dense than the anterior region of the mandible.
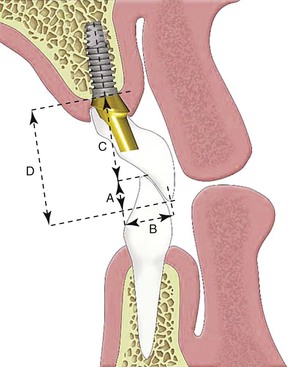
In the premaxilla, esthetics and phonetics dictate that the replacement teeth be placed at or near their original position, often cantilevered off the residual ridge, which usually is resorbed palatally and superiorly (Figure 30-9). The arc of closure is anterior to the residual ridge; as a consequence, the moment force is greatest against the maxillary anterior crowns supported by implants and directed against the thinner facial bone33 (Figure 30-10). All mandibular excursions place lateral forces on the maxillary anterior teeth, with resulting increased stress on the crestal bone, especially on the labial aspect of the implant.
As a consequence, many treatment plan aspects place the edentulous maxilla at a high risk of implant failure:
1. The narrow ridge of a premaxilla has parallel walls of bone, so an osteoplasty to increase width is less effective (Figure 30-11). Therefore, the narrow ridges more often need narrower implants (resulting in increased stress concentrations in the implant and contiguous interfacial tissues, particularly at the crestal region).
2. This region is the most difficult to insert implants parallel to each other and within the contours of the restoration (Figure 30-12). The use of facial cantilevers results in increased moment loads at the implant crest, often leading to localized crestal remodeling and implant or abutment fracture.
3. Oblique centric contacts, resulting in potentially harmful, off-axis load components
4. Lateral forces in excursion, resulting in greater moment loads applied to the implant (Figure 30-13)

5. Reduced bone density, resulting in compromised bone strength and loss of implant support)
To increase implant and prosthesis survival rates, treatment for maxillary FPs with division A bone are planned similarly to that for mandibles with C minus height (C–h) bone and greater factors of forces. In other words, more implants are typically used in the maxillary arch compared with the mandibular situation. For example, four or more implants are inserted from first premolar to first premolar to replace the anterior eight teeth. In addition, subantral augmentation often is performed to place more distal implants and dramatically improve the A-P distance when the anterior and posterior implants are splinted together. This treatment approach has proved successful in yielding success rates in the maxilla similar to those of mandibular restorations.
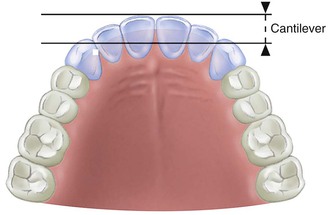
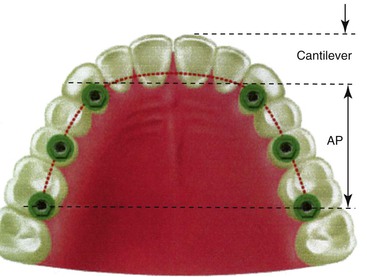
Premaxilla Arch Form: Dentate and Residual Bone
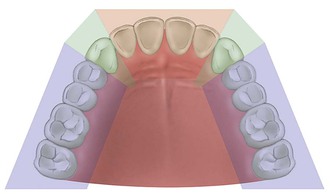
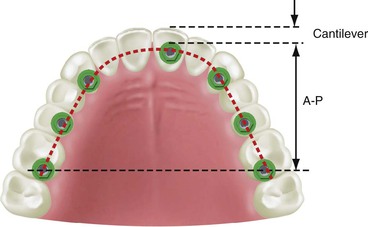
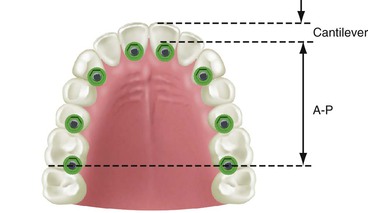
The maxillary arch may be divided into five segments similar to an open pentagon33 (Figure 30-14). The central and lateral incisors represent one segment, each canine a separate segment, and the posterior premolars and molars represent individual segments. Each segment is essentially a straight line, with little resistance to lateral forces. But because they are aligned along the arch, connecting at least three segments creates a tripod and provides an A-P distance (A-P spread) with mechanical properties superior to a straight line and with greater resistance to lateral forces. The A-P spread for anterior (or posterior) cantilevers corresponds to the distance between the center of the most distal implant (in the splint) and the anterior aspect of the most anterior implant.
Three of the five maxillary arch segments described are part of the premaxilla: the canine, the incisors, and the opposite canine. Therefore, to achieve a sound biomechanical system able to sustain lateral forces during mandibular excursions and the angled forces of centric occlusion, at least one implant should be placed in each anterior section and then splinted together. Previous studies have shown that the force distributed over three abutments results in less localized stress to the crestal bone than two abutments.35 Hence, at least three anterior implants usually are required: one in each canine position and at least one in one of the four incisor positions.33,36
Implant Number and Premaxilla Arch Form
In Chapter 12, a discussion of key implant positions for implant prostheses is presented. The rules to determine the key implant positions are no cantilever, no posterior three adjacent pontics, the canine site, and the first molar site. In the premaxilla, the dentate arch form may also affect the implant number (Box 30-4).
The type of arch form of the maxilla influences the treatment plan of the maxillary prostheses. Three typical dentate arch forms for the maxilla are square, ovoid, and tapering. The edentulous maxilla residual ridge of bone also may have three arch forms. Esthetic requirements may require a dentate arch form different from the residual ridge form. The dentate arch form of the patient is determined by the final teeth position in the premaxilla and not the shape resulting from the residual ridge. A residual ridge may appear square because of resorption or trauma. However, the final teeth position may need to be cantilevered to the facial with the final prosthesis. In other words, an ovoid dentate arch form may be needed to restore a residual edentulous square arch form. The number and position of anterior implants are related to the arch form of the final dentition (restoration), not the existing edentulous arch form.
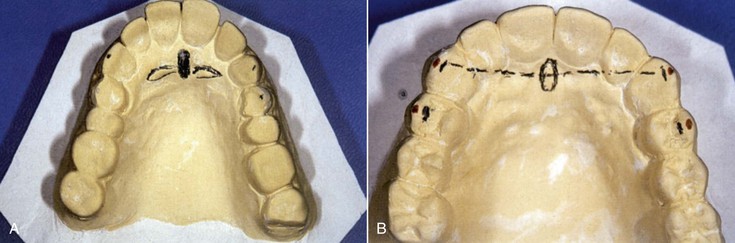
To determine the dentate arch form one line is drawn through the incisive papilla to separate the right and left maxilla into two equal components. A second line is then drawn through the middle of the incisive foramen perpendicular to the first line (Figure 30-15). The second line will pass over the incisal tip position of the maxillary canines, whether the dentate arch is square, ovoid, or tapering37 (Figure 30-16).
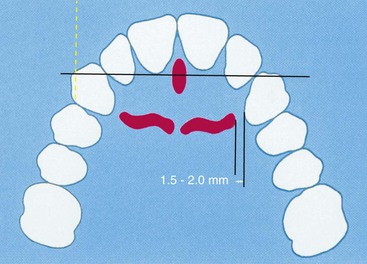
A third line is then drawn parallel to the second line along the facial of the maxillary central incisors33 (Figure 30-17). When the distance between the second and third line is less than 8 mm, a square dentate arch form is present. When the distance between these lines is 8 to 12 mm, an ovoid dentate arch form exists. A distance of more than 12 mm indicates that a tapered dentate arch form is present (Box 30-5).
In a square dentate arch form, lateral and central incisors have minimum cantilever facially compared with the canine position. Mandibular excursions and occlusal forces may be reduced on the canine implants. As a result, implants in the canine position may suffice to replace the anterior six teeth for a full-arch FP because they are splinted to additional posterior implants (Figure 30-18). The four pontics between the canines create reduced forces because (1) the forces are lowest in the incisor region and (2) a square arch in the maxilla has less cantilevered occlusal forces to the canines (Figure 30-19).
If the final teeth position is an ovoid arch form, three implants should be positioned in the premaxilla for a FP33 (Figure 30-20). For the fixed restoration of an ovoid dentate arch form (which is the most common arch form), planning for implants in the canine positions and at least one additional implant, preferably in a central incisor position, is important. The additional implant resists the additional forces created in this arch form, enhances prosthesis retention, and reduces the risk of abutment screw loosening (Figure 30-21).
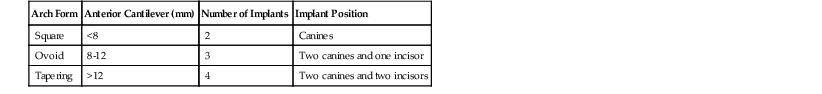
The fixed restoration of a tapering dentate arch form places the greatest forces on anterior implants, especially when pontics replace the incisors (Figure 30-22). The anterior teeth are cantilevered facially from the canine position, with increased forces in centric occlusion and during mandibular excursions. As such, four implants should be considered to replace the six anterior teeth for a FP33 (Figure 30-23 and Table 30-1).
TABLE 30-1
Treatment Plan for Edentulous Premaxilla
| Arch Form | Anterior Cantilever (mm) | Number of Implants | Implant Position |
| Square | <8 | 2 | Canines |
| Ovoid | 8-12 | 3 | Two canines and one incisor |
| Tapering | >12 | 4 | Two canines and two incisors |
The worse-case scenario is a patient requiring a tapered dentate arch form to be restored on a square residual ridge form (Figure 30-24). As a result, in these cases, a bone graft may be required to restore a more compatible residual ridge form. The bilateral canine and central incisor positions are biomechanically the best option for a tapered premaxilla. These positions are preferred when other force factors are greater, such as crown height, parafunction, and masticatory muscular dynamics.
When a dentate tapered arch form is restored on a square residual ridge form, implants are especially indicated in the posterior regions. The most posterior implants are placed in the second molar position (along with a first molar implant) to increase the A-P distance and counter some of the anterior cantilever effect33 (Figure 30-25).
When one canine region cannot be used to place an implant in the edentulous maxilla, an implant in the first premolar and lateral incisor implant on each side of the missing canine are suggested to compensate for this vital position (Figure 30-26). A central incisor implant and canine position in the contralateral section can be splinted to these implants to act as abutments for the fixed restoration.
In the presence of severe force factors, two implants most often are required to sustain the direction of force created during a mandibular excursion, which means a minimum of four implants is suggested to replace the anterior six teeth. In the presence of these severe forces (e.g., severe bruxism), larger-diameter implants should be used, especially in the canine position (which has increased angulation in excursions and higher bite forces). As such, in many instances, the completely edentulous anterior maxilla is restored with three or four implants splinted together to support the FP. In addition, posterior implants are usually required, especially for a full-arch fixed restoration.
Precise implant position in a mesiodistal aspect is not mandatory in a FP-3 prosthesis (Figure 30-27). The pink restoration materials that replace the soft tissue drape hide the implant position and do not affect the mesiodistal width of the overlaying teeth.
Posterior Implant Number
As previously presented, the maxilla may be compared to an open pentagon, with five different sections: the central and laterals, the bilateral canines, and the bilateral premolars and molars. Hence, posterior implants splinted to anterior implants are a particular advantage because four or five different planes of movement are connected together.
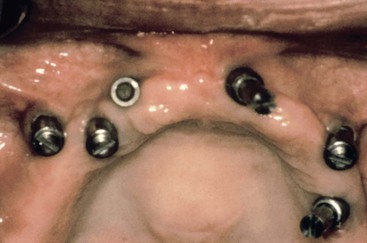
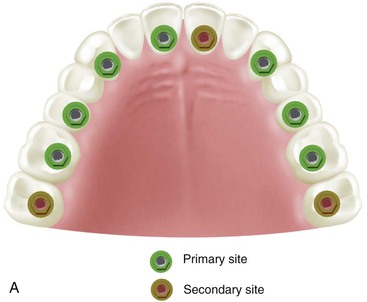
The number of implants most often used in an edentulous maxilla for a FP should be in a range from seven to 10 implants.33 Many reports concur on the fact that maxillary bone tends to be of poorer quality and volume and presents few biomechanical advantages. To compensate for the poor local conditions, a greater number of implants can be planned to create a greater A-P spread, hence the need for sinus grafts or premaxilla reconstruction. When force factors are moderate to severe or bone density is poor, more implants should be inserted and in greater diameter to enhance the surface area. Likewise, the number of implants needed in an edentulous premaxilla is related to arch shape, as previously addressed.
With these concerns in mind, the minimum implant number and suggested locations for a completely edentulous maxillary FP is usually seven: at least one incisor position, bilateral canine positions, bilateral second premolar sites, and bilateral distal half of the maxillary first molar sites (Figure 30-28). These seven implants should be splinted together to function as an arch. These implant positions create sufficient space between each implant to accommodate most any implant diameter. The first molar implant sites in a completely edentulous maxilla almost always require sinus grafting because most edentulous maxillary posterior regions are inadequate in available bone height.
When force factors are moderate to severe, the implant number should increase to eight or 10 implants.33 When eight implants are selected, the additional implant is usually placed in the premaxilla in a central incisor position. When 10 implants are used for patients with higher force factors or poor bone density, additional implants are planned in the distal half of the second molar position to improve the arch form, increase the A-P spread, and eliminate posterior cantilevers. This is an excellent biomechanical design to minimize stress. This foundation design also may counter the effect of a facial cantilever off the residual bone (tapered dentate arch form) for an esthetic tooth position and is also indicated for patients with severe parafunction such as chronic bruxism.
The first and second molar position is also a benefit when the premaxilla has higher force factors/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses