chapter 30 Fundamentals of General Anesthesia
General anesthesia has been defined as an irregular, reversible depression of the higher centers of the central nervous system (CNS) that makes the patient unconscious and insensible to pain.1 Pallasch2 described general anesthesia as “hypnosis (sleep or loss of consciousness) accompanied by the loss of protective laryngeal reflexes (cough). Ideally, general anesthesia represents the simultaneous presence of analgesia (loss of pain), amnesia (loss of memory) and hypnosis along with reflex inhibition and loss of skeletal muscle tone which allows for safe surgical procedures.” When the CNS is depressed to the extent that consciousness is lost, changes occur in the physiology of the patient that would be life threatening in the absence of a “guardian” trained in the management of the unconscious patient. These changes include partial or complete airway obstruction, hypoxia, hypercapnia, loss of the ability to clear the tracheobronchial tree, respiratory depression, blood gas and pH changes, cardiovascular depression, and depressed or absent protective reflexes.
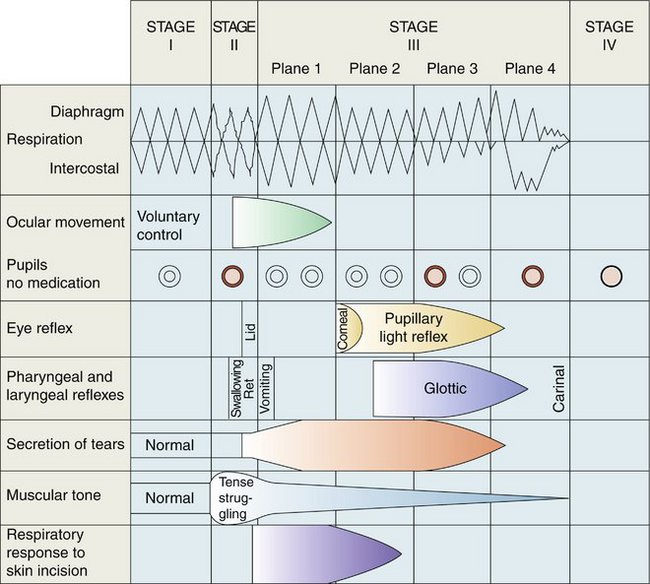
Several types of general anesthesia are recognized. The most frequent use of general anesthesia in dentistry is within the specialty of oral and maxillofacial surgery. The oral and maxillofacial surgeon has been responsible, in large part, for the development of outpatient or ambulatory general anesthesia using intravenous (IV) drugs, originally barbiturates (termed ultralight general anesthesia, where the patient is maintained in Guedel stage II of anesthesia) or conventional general anesthetic agents (with the patient maintained in Guedel stage III of anesthesia) (Table 30-1). As hospital costs rise, ambulatory general anesthesia has gained popularity within the medical profession. The dentist anesthesiologist, a dentist trained in anesthesiology (minimum of 2 years), has made ambulatory general anesthesia available to patients requiring nonoral surgical dental care, such as periodontics, endodontics, implants, and restorative procedures.
| Four stages of anesthesia are described. |
| Guedel based his observations on the following parameters: |
A third type of general anesthesia available to the dental patient is traditional inpatient general anesthesia. Whether the anesthesiologist is a dentist or a physician, the patient is admitted into the hospital and brought to the operating theater, where general anesthesia is induced and the dental procedure completed. The dentist performing the dentistry need not be trained in general anesthesia for this type of anesthesia to be used because the anesthesiologist assumes responsibility for inducing and maintaining the appropriate depth of anesthesia. Each of these types of general anesthesia is described in Chapter 31.
ADVANTAGES
DISADVANTAGES
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses