Chapter 3
TMJ Disorders
Aim
This chapter gives a simplified approach to understanding and managing temporomandibular joint (TMJ) disorders. It reviews the options for clinical management of TMJ disorders and demonstrates that the majority of TMJ disorders respond to simple therapeutic approaches that should be readily available in a general practice setting.
Outcome
Having read this chapter, the clinician should be able to:
-
identify characteristics of TMJ function that fall within the normal range
-
be familiar with signs and symptoms that indicate a TMJ disorder
-
have an understanding of when it is appropriate to manage a TMJ disorder in general practice and when to refer for specialist advice and management.
Anatomy of the Temporomandibular Joint
The TMJ is classified as ginglymoarthrodial in nature, denoting a joint having the form of both a hinge joint and a sliding joint; this refers to the ability of the condyle to rotate and translate. The anatomy of the joint is illustrated in Fig 3-1. This synovial joint requires complex neuromuscular control to ensure appropriate coordination of its three-dimensional movement. The articulating components of the joint are composed of fibrocartilaginous tissues, in contrast to cartilage, which covers the articulating components of the other moveable joints in the body. The mandible can move with great speed and precision; huge forces can be applied between the mandible and the maxilla, given the unique characteristics of the primary muscles of mastication. The potential for self-repair is good: a feature that influences treatment planning and the management of disorders.
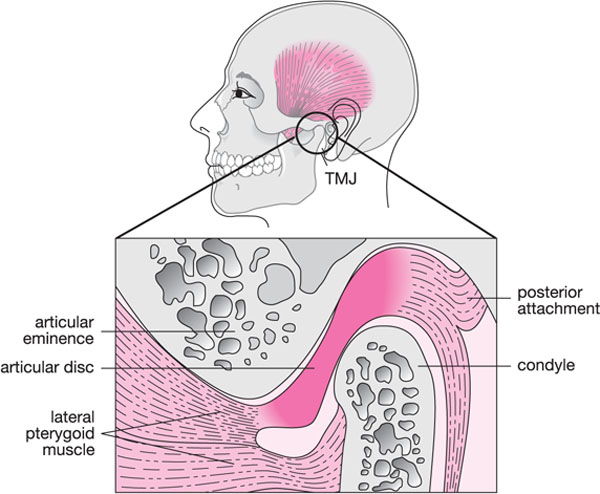
Fig 3-1 Illustration of the anatomy of the temporomandibular joint (TMJ).
The primary bony elements of the TMJ include the glenoid fossa in the base of the skull and the mandibular condyle. In the dried skull, these structures appear to fit loosely against each other. In reality, the fibrocartilaginous tissues covering the articular surfaces fit neatly against each other during normal function, lubricated by synovial fluid and encased by a joint capsule of white collagenous tissue. The intra-articular disc (meniscus), interposed between the condyle and the glenoid fossa, creates an upper and lower joint compartment. The limited attachment of the disc to the underlying condyle, through medial and lateral ligaments, provides a freedom of movement whereby the disc can move anteriorly or posteriorly with the condyle rotating underneath. Disc stability is enhanced by its biconcave shape, with a thickened periphery and relatively thin central contact area. The posterior border of the disc is ideally positioned on the so-called “12 o’clock position” of the articulating surface of the condyle. Physiologically, the position of the disc is determined by a number of factors, including the physical contact with the opposing bony surfaces and the attachment of muscle fibres to the anterior and posterior borders of the disc. Fibres from the superior belly of the lateral pterygoid muscle are inserted into the anterior border of the disc, with the muscle component of the posterior attachment tissues connecting the posterior border of the disc to the posterior wall of the glenoid fossa. A simple perspective on disc position is the disc as part of a pulley system, with the precise location of the disc being determined by the balance of different muscle actions. A more complex view of disc mobility involves both neuromuscular and biomechanical considerations, which are outwith the scope of this book.
The quality and volume of synovial fluid in the upper and lower joint compartments contribute to the lubrication of the articulating surfaces. Disease or disorders of the TMJ may result in changes in synovial fluid characteristics; these, in turn, affect the functionality of the joint. Apart from contributing to smooth joint movements, synovial fluid also has a nutritive function.
Sensory and motor innervation of the TMJ is mediated through the trigeminal nerve. The auriculotemporal nerve, a branch of the mandibular division of the trigeminal nerve, provides most of the sensory innervation to the joint structures. Branches from the posterior deep temporal nerve and the masseteric nerve infiltrate the joint capsule both anteriorly and anteromedially.
Normal and Abnormal Joint Function
Healthy TMJs allow smooth movement of the mandible without pain or discomfort. A full range of movement for an adult is somewhere between 40 and 60 mm of opening, measured interincisally as described in Chapter 2.
As discussed in Chapter 2, it is important to measure the midline and the lateral range of movement and know what is normal. Even experienced practitioners make mistakes by merely observing (“eyeballing”) the range of opening.
Normally, the TMJs should function free of noise, clicking or crepitations. The presence of joint noise with condylar movement does not always indicate the presence of disease or dysfunction. Approximately 80% of young adult females have detectable clicking, with a slightly smaller percentage of males having joint noises.
Joint Function and Noises
Traditional teaching suggests that the posterior band of the disc is located at the 12 o’clock position on the condyle in the closed mouth position. The initial phase of mandibular movement involves condylar rotation with no significant shift in the position of the disc. However, as the condyle moves downwards and forwards along the slope of the articular eminence, the disc position begins to change. Movement of the condyles directly influence the path of movement of the lower incisors. This is represented by the sagittal envelope of movement depicted in Fig 3-2.
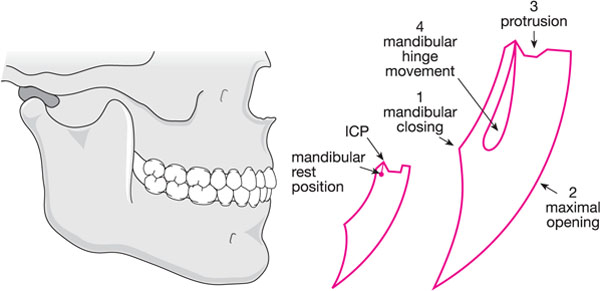
Fig 3-2 The envelope of motion depicting mandibular movement. 1, Mandibular closing; 2, maximal opening; 3, protrusion from the intercuspal position (ICP); 4, hinge movements of the mandible without translation.
The disc and underlying condyle move in unison when the mandible moves towards maximum mouth opening. As the mouth begins to close, the phases are reversed, with the condyle moving back into the fully seated position in the glenoid fossa (Fig 3-3). As the teeth are about to meet in maximum intercuspation, the condyle rotates underneath the intra-articular disc. The final closed position has the disc seated between the condyle and glenoid fossa with the posterior band of the disc in the 12 o’clock position on the condyle.
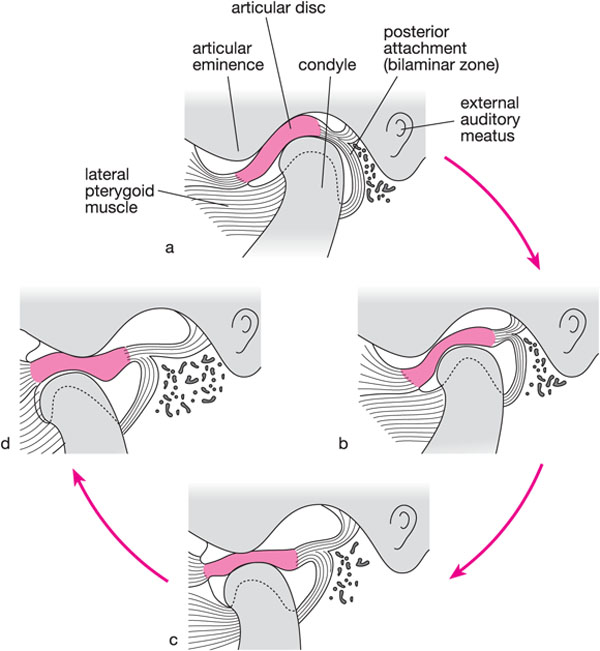
Fig 3-3 Normal mandibular movement. (Courtesy of MK Solberg and GT Clark, Temporomandibular Joint Problems, Chicago: Quintessence, 1980.)
This description of condyle–disc interaction explains much of what we currently know about the mechanics of TMJ movement in a healthy young adult. Unfortunately, the same model does not apply to immature or ageing joints. For example, with ageing the disc is often completely displaced within the joint, while remaining symptom free. It is postulated that the natural shape of the disc is gradually lost over time and the integrity of the supportive disc ligaments is reduced or compromised. Eventually the disc may play a minor role in providing stability for the joint. Yet, at the same time, range of movement is typical and continues to be pain free. Less is known about joint stability and movement during growth and development. The overall conclusion must be that the mechanism of joint movement changes through the course of life. This pattern of change makes it more difficult to interpret the symptoms of certain patients seeking treatment.
TMJ disorders can be broadly divided into two groups:
-
inflammatory conditions: capsulitis and synovitis
-
internal derangements.
The definition of joint derangement varies. In the context of this book, it is used to imply a change in the shape or position of the intra-articular disc, which results in limited movement or pain with function.
Signs and Symptoms of TMJ Disorders
Pain
The most common reason for patients seeking help in respect of TMJ function is jaw pain: a symptom frequently accompanied by restrictions in movement (Table 3-1). Pain is usually described as dull, aching when moderate, and throbbing when severe. Joint pain may radiate anteriorly into the posterior aspect of the mandible or maxilla and is known to trigger headaches.
| Causes | |
|
Trauma |
|
|
Rheumatological disease |
|
|
Neoplastic disease |
|
|
Pain referral |
|
Acute joint pain of sudden onset is frequently associated with recent trauma to the orofacial area. A sudden blow to the face, if sufficiently forceful, may result in immediate joint swelling and pain. An inflammatory response to trauma is easily diagnosed and managed. Acute joint pain is usually described as an intense throbbing discomfort, which may be continuous, and unrelated to mandibular movement. Patients are likely to recover spontaneously, and healing follows a natural course over typically 10 to 14 days.
Management of acute TMJ pain involves:
-
joint rest (soft diet)
-
eliminating parafunctional behaviours
-
thermal applications
-
non-steroidal anti-inflammatory drugs (NSAIDs).
Use of NSAIDs will decrease pain and swelling and expedite the healing process. The repeated application of cold packs may help to decrease tissue swelling. A soft diet and the patient controlling parafunctional habits will limit the need for mandibular movement.
Chronic and recurrent joint pain tends to be associated with rheumatological disease, referred pain and possibly neoplastic disease. Where the cause of such pain is uncertain,/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


