3
The treatment planning process
- Understand the three fundamental steps in orthognathic treatment planning.
- Understand the four keys to hard tissue planning.
- Understand the difference between initial, combined treatment planning and final surgical planning.
- Understand the interaction between pre-surgical orthodontic planning and provisional surgical planning.
3.1 Introduction
Treatment planning for the orthognathic patient should be an inter-disciplinary process, carried out between the team members, with the patient present. Following appropriate diagnosis the clinicians will be able to discuss the proposed dental and skeletal movements, taking the patient’s concerns into account.
No individual part of the plan can be made in isolation and a continuous, interactive thought process is required to arrive at the optimal combination of orthodontic and surgical movements.
3.2 Three fundamental planning steps
The planning process typically involves three basic steps:
3.2.1 Envisaging the desired aesthetic changes
This relies on the experience and judgement of the clinicians to a large extent and, even between experienced clinicians, there can be disagreement regarding the facial aesthetic goals. Where this occurs, it is particularly important to ensure that planning remains focused on the patient’s concerns. Guidelines can help in determining the site and magnitude of the discrepancy and have been discussed in Chapter 2.
Photo-cephalometric planning may be required at this stage when maxillo-mandibular disharmony is mild and it is not clear which single jaw correction would produce the best results, or in borderline cases where it is not clear if single or bi-maxillary surgery is required.
3.2.2 Deciding on the required jaw movements
The soft tissue changes, in response to surgical movement of the underlying bones, vary depending on the anatomical level (see Chapter 6). This is not an exact science, since the evidential basis for hard-to-soft tissue movement ratios is limited and there is considerable individual and racial variation.
In addition, soft tissue changes occur not just in profile, but in three dimensions and the clinicians should be mindful of potentially adverse effects. In particular, with Le Fort I osteotomy:
- The alar base has a tendency to flare, even where there is no vertical impaction of the maxilla (Figure 3.1).
- The nasal tip turns upwards with maxillary advancement and impaction.
- Correction of severe maxillary deficiency, accompanied by zygomatic and infra-orbital deficiency, can leave the patient with an unattractive appearance of bi-maxillary protrusion and enophthalmos.
Figure 3.1 Superimposition of mean pre-surgical (white) and post-surgical (red) three-dimensional mesh diagrams of Le Fort I advancement osteotomy patients showing flaring of the alar base.
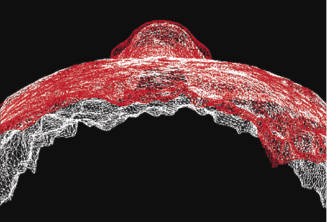
These effects are not entirely predictable and can be controlled by the surgeon to some extent (see Chapter 7), but they will tend to be greater with larger maxillary movements. Care must be taken to formulate a plan that will adequately correct the jaw disharmony, but also limit the unaesthetic side effects. It is important to take into account the shape of the nose and the alar base width, in proportion to the rest of the face, along with the upper facial morphology, particularly where a large maxillary advancement will be required.
3.2.3 Planning orthodontics to allow the required jaw movements
Pre-surgical orthodontics should be aimed at placing the teeth in a position that allows the jaws to be surgically moved by the amount estimated to produce the desired facial aesthetic changes. A key feature of this approach is that the degree of incisor decompensation should be tailored to allow the planned surgical movements, which involves setting a target overjet (class II cases) or reverse overjet (class III cases). This is conceptually different to an approach where the primary aim is to set the incisor inclinations to their cephalometric norms, with the resulting overjet then dictating the size of the surgical correction (see also Chapter 4).
The amount of incisor decompensation that will be required can be aided by profile cephalometric planning at this stage, but its validity may be limited until the final tooth positions are known at the end of pre-surgical orthodontics.
3.3 Four keys to dento-skeletal planning
Whilst the initial step in the planning process is envisaging the final aesthetic outcome, the delivery of treatment usually takes place in the reverse sequence. The teeth are orthodontically positioned first, then the jaws surgically moved to produce the soft tissue changes. The orthodontic tooth movements and the surgical jaw movements are inter-dependent and must be planned together. In most cases the major orthodontic tooth movements will be carried out first but, at the initial planning stage, it can be difficult to predict how accurately the orthodontist will be able to achieve the desired tooth positions. The initial surgical plan can therefore only be approximate and it is not until the patient is seen again following the completion of pre-surgical orthodontics, that the definitive surgical plan can be finalised.
The following four keys should be considered in planning the dento-skeletal movements:
3.3.1 Upper incisor and maxillary position
The first step is deciding where to place the upper incisors in all three planes of space, and their final position will be the net result of both orthodontic and surgical movements.
Antero-posterior positioning
Planning the optimal antero-posterior position for the upper incisors must take into account their position in the horizontal plane as well as their inclination. Antero-posterior orthodontic adjustment of the incisors pre-surgically has two objectives:
These objectives are inter-linked and must be considered simultaneously. There are specific planning considerations that relate to the different malocclusion groups.
Class II skeletal pattern.
In many class II, division 1 cases, the upper incisors will be at an aesthetically acceptable inclination and will require minimal adjustment. If they are proclined and the plan is to retract them to a more average inclination, it must be borne in mind that the upper lip will drop back in response to this, which can accentuate any underlying deficiency of the maxilla. In Class II, division 2 cases the upper central incisors will require proclination and this will result in some increase in lip support.
Where a degree of maxillary deficiency does accompany the mandibular deficiency (bi-maxillary retrusion), a decision must be made as to whether the position of the maxilla also warrants surgical correction to bring the upper incisors into an aesthetically pleasing position. In cases where the maxillary deficiency is mild, leaving the upper incisors slightly proclined may allow adequate advancement of the mandible, whilst avoiding the need for maxillary osteotomy. However, in cases where this may leave the maxilla looking slightly deficient, para-nasal augmentation using bone grafts can be considered as a surgical adjunct.
Where the degree of maxillary retrusion is considered severe enough to require surgical advancement, it is important to ensure that the target overjet is sufficient to allow the maxilla to be advanced by a worthwhile amount (i.e. at least 4mm), whilst still keeping the mandibular advancement to within an achievable surgical limit (i.e. approximately 10mm maximum with a sagittal split osteotomy). An overjet of 8mm is therefore about the maximum that will be compatible with bi-maxillary advancement osteotomy in a class II patient. An adjustment to this calculation will be necessary where the maxilla also needs to be impacted, allowing a degree of mandibular advancement through autorotation. In some cases, with severe mandibular deficiency, other surgical techniques, including inverted ‘L’ osteotomy with bone graft, or distraction osteogenesis, may be considered.
In cases where prominence of the anterior part of the maxilla (pre-maxilla) has resulted in dento-alveolar protrusion, an anterior maxillary osteotomy may be required. This is often carried out in conjunction with extraction of upper first premolars and may be a more predictable and quicker alternative to orthodontic retraction of the teeth.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


