3 Pre-Operative Assessment and Treatment Options for Post-Extraction Implants
3.1 Factors Influencing the Treatment Outcomes of Implants in Post-Extraction Sites
D. Buser, S. Chen
3.1.1 Introduction
Today, implant placement in post-extraction sites is a common clinical procedure. Patients often present with teeth that are failing due to caries, chronic periodontitis, root fracture, failed endodontic treatment, lack of sufficient coronal tooth structure, and trauma. The clinician must assess the tooth and make recommendations for the timing of the implant placement after the tooth is extracted. The primary objective of implant therapy is to achieve successful treatment outcomes with high predictability and a low risk of complications, both from a functional and an esthetic point of view. Secondary therapeutic objectives are to achieve treatment success with the least possible number of surgical interventions, low morbidity for the patient, and a short treatment period between tooth extraction and prosthetic restoration. Various efforts have been made in the past 10 to 15 years to modify treatment protocols in these areas to make implant therapy more attractive to patients and, hence, to increase patients’ acceptance of this treatment modality. However, these modifications should not compromise the predictability for successful outcomes nor increase the risk of complications.
For the clinician, it is important to understand that various treatment options are available in post-extraction sites, such as immediate, early, or late placement. As outlined in the updated literature review in Chapter 2, each of these treatment options has its specific characteristics, indications and contraindications, advantages and disadvantages, levels of predictability and risks involved, levels of difficulty to perform the procedure, and, last but not least, different levels of scientific evidence.
Treatment outcome in general is influenced by four factors, which have a close relationship with each other, as shown in Fig 1. The key factor is the clinician, who makes all the decisions based on his or her judgment of the clinical situation. The clinician evaluates the patient, selects necessary biomaterials, and decides on the most appropriate treatment approach to provide the anticipated treatment outcome.
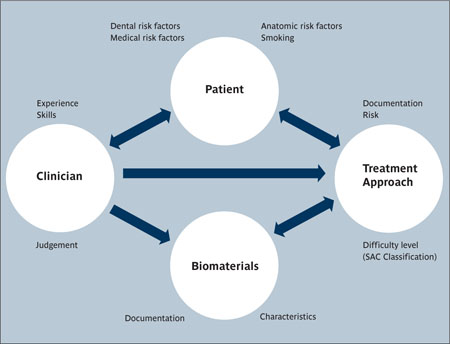
Fig 1 The four factors influencing treatment outcomes with implant therapy and their relationship with each other.
Fig 1 demonstrates the four factors that mainly influence treatment outcomes with implant therapy in general. This diagram can be applied to every clinical situation with specific implications. In the following paragraphs, these four aspects will be discussed for implant therapy in post-extraction cases.
Emphasis will be placed on single-tooth replacement in post-extraction sites in the esthetic zone, since this is a very frequent clinical situation. The clinical handling of implant sites with multiple missing teeth post-extraction in the anterior maxilla, however, will be discussed separately in one of the upcoming ITI Treatment Guides. In addition, post-extraction implant placement in posterior sites will also be presented and discussed in the case-report section.
3.1.2 The Patient
Any type of implant therapy must include a careful preoperative analysis to assess the individual risk profile of a given patient. For post-extraction implant placement in the anterior maxilla, a comprehensive preoperative analysis must be undertaken because implant procedures often involve various fields of dentistry. In general, four risk factor groups can be differentiated:
-
Medical risk factors
-
Smoking
-
Dental risk factors
-
Anatomic risk factors
It should be noted that for a risk factor to be identified, a causal relationship needs to be established with prospective studies. In implant dentistry, this evidence is generally lacking, and the factors discussed represent risk indicators. For the purpose of this clinical discussion, the more general term risk factor is utilized.
The first two groups of risk factors contain systemic risk factors that influence treatment outcomes in general, inside and outside the oral cavity. They have to be examined as part of the patient’s medical history. The latter two groups contain local risk factors that mainly have a local impact on treatment outcomes. All these factors will be briefly discussed in the following paragraphs.
Medical risk factors. This term comprises all diseases or conditions that negatively affect the wound-healing and bone-remodeling capacity of the patient, and the compliance of the patient for the long-term maintenance of osseointegrated implants. A first attempt to classify these risk factors was made by the ITI in the late 1990s at the second ITI Consensus Conference. The medical risk factors were listed under high-risk factors and risk factors (Buser and coworkers, 2000). The following diseases or conditions were included as high-risk factors: (1) serious osseous disorders such as osteogenesis imperfecta or ostemalacia, which are rarely encountered by clinicians; (2) patients with an immunocompromized situation due to viral infection (HIV) or medication (corticosteroids, oncologic chemotherapy etc.); and (3) patients with a drug habit or a psychological or mental disorder that affects compliance. In the group of risk factors, the following disorders or conditions were included: radiotherapy; severe diabetes, especially juvenile (Type 1) diabetes; and bleeding disorders such as hemorrhagic diathesis or drug-induced anticoagulation. This group of risk factors has not changed much over the past ten years, although a recent review paper (Mombelli and Cionca, 2006) concluded that the level of evidence is low. No data was found for the most severe medical conditions, simply because implant therapy has not been performed in such patients. In recent years, a new medical risk factor has been identified in patients taking bisphosphonates on a regular basis (Marx and coworkers, 2005). This medication, often used in cancer patients with osseous metastases or in patients with osteoporosis, inhibits osteoclastic activity and bone resorption. Bisphosphonates can cause osteonecrosis, resulting in large areas of exposed necrotic bone in the oral cavity. At present, it seems that only the intravenous application of bisphosphonates is considered an absolute contraindication for implant therapy (Scully and coworkers, 2006). In patients who take oral bisphosphonates, a recent short-term study indicated no increased risk of developing bone necrosis (Fugazzotto and coworkers, 2007).
Smoking. Smoking has long been known to have a negative impact on the long-term prognosis of dental implants (Bain and Moy, 1993; De Bruyn and Collaert, 1994). A recent systematic review clearly confirmed the relationship between smoking and an increased risk of biologic complications such as peri-implant infection or an increased failure rate (Strietzel and coworkers, 2007). A differentiation is often made between non-smokers and various levels of smoking. In a recent study, heavy smokers (> 20 cigarettes per day) demonstrated the highest failure rate (Sanchez-Perez and coworkers, 2007).
Dental risk factors and anatomic risk factors. These two groups of local factors will be discussed together, since they are part of the Esthetic Risk Assessment (ERA) proposed by Martin and coworkers in Chapter 3 of the ITI Treatment Guide, Vol. 1 (Martin and coworkers, 2006). The authors presented a table of 12 risk factors (Table 1), which can be used in daily practice to evaluate patients.
| Esthetic Risk Factors | Low | Medium | High |
| Medical status | Healthy, cooperative patient with intact immune system | Reduced immune system | |
| Smoking habit | Non-smoker | Light smoker (<10 cig/d) | Heavy smoker (≥ 10 cig/d) |
| Patient’s esthetic expectations | Low | Medium | High |
| Lip line | Low | Medium | High |
| Tissue biotype | Low-scalloped, thick | Medium-scalloped, medium thick | High-scalloped, thin |
| Shape of tooth crowns | Rectangular | Triangular | |
| Infection at implant site | None | Chronic | Acute |
| Bone level at adjacent teeth | ≤ 5 mm to contact point | 5.5 to 6.5 mm to contact point | ≥ 7 mm to contact point |
| Restorative status of neighboring teeth | Virgin | Restored | |
| Width of edentulous span | 1 tooth (≥ 7 mm) | 1 tooth (<7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact soft tissue | Soft-tissue defect | |
| Bone anatomy of alveolar crest | Alveolar crest without bone deficiency | Horizontal bone deficiency | Vertical bone deficiency |
The first two factors – medical status and smoking habit – have already been discussed above. A third general factor is the patient’s expectation of the treatment outcome. The other nine factors represent local factors that will be discussed in relation to implant placement in post-extraction sites of single teeth in the anterior maxilla.
Patient’s expectations. When the patient is first examined, it is important to determine the patient’s expectations concerning treatment outcome. Based on the anatomic situation, these expectations can sometimes be unrealistic. Therefore, an open discussion of anatomic risk factors and their potential impact on the treatment outcome and related risk of complications will help to avoid disappointing outcomes for patients with high esthetic expectations. Such patients should be considered “high risk” in terms of esthetics.
Lip line. The lip line is associated with the amount of tooth and supporting tissues that are visible when the patient chews, speaks, or smiles. Three categories are differentiated: a low, a medium, and a high lip line (Martin and coworkers, 2006). The highest risk is associated with a high lip line (Fig 2), when patients often display their maxillary anterior teeth in their entirety, as well as a significant portion of the alveolar process. In contrast, the esthetic risk is reduced as the lip line is positioned lower, because the lips effectively mask suboptimal outcomes associated with the appearance of the gingival tissues, tooth proportions, and the apical aspects of the restoration.

Fig 2 Patient with a high lip line.
Tissue biotype. Here, a differentiation has been made between thick, medium, and thin tissue biotypes (Martin and coworkers, 2006). Each has its specific characteristics. The least risk is posed by a thick tissue biotype with a thick, broad band of attached mucosa (Fig 3), typically resistant to recession (Kan and coworkers, 2003b; Kois, 2004). The thick mucosa is able to mask the color of the implant and their submucosal metallic components, reducing the risk of not achieving a pleasing esthetic result. This biotype clearly favors the long-term stability of esthetic peri-implant soft tissues.

Fig 3 Patient with a thick tissue biotype and square teeth, which is considered a low esthetic risk.
In contrast, patients with a thin tissue biotype have the highest esthetic risk (Fig 4), although they can display excellent esthetic single-tooth restorations if adjacent teeth are periodontally healthy and have unaltered bone-crest levels. These patients normally form and maintain dental papillae, but have a clearly increased esthetic risk of mucosal recession (Evans and Chen, 2008; Kan and coworkers, 2003b; Kois, 2004). In these patients, a slightly more palatal implant position can favor an optimized esthetic outcome.

Fig 4 Patient with a thin tissue biotype and a high-scalloped gingival line combined with a triangular tooth shape. This represents a high esthetic risk.
Shape of adjacent tooth crown. The shape of the missing and adjacent teeth can profoundly influence the degree of risk associated with implant-supported single crowns in the esthetic zone. Triangular tooth shapes (Fig 4) are often combined with a thin, highly scalloped tissue biotype (Müller and coworkers, 2000). A clearly increased esthetic risk is evident when a triangular tooth shape is associated with reduced vertical bone levels at adjacent roots, causing the loss of interproximal papilla height. These patients will often require an implant superstructure that is square-shaped with long, extended contact zones, potentially compromising the final appearance. When the restoration includes triangular tooth shapes, interproximal spaces (black triangles) must be anticipated. The risk is reduced when rectangular or square teeth are present, often in combination with a thick tissue biotype (Fig 3).
Bone level at adjacent teeth. As clinical studies have shown, the presence or absence of an intact interproximal papilla at an implant-supported crown mainly depends on the bone levels at adjacent teeth (Choquet and coworkers, 2001; Kan and coworkers, 2003b; Ryser and coworkers, 2005). Where local infections have resulted in vertical bone loss at adjacent teeth and the distance between the contact point and bone crest level exceeds 6 or even 7 mm, the risk of a compromised esthetic outcome is clearly increased (Figs 5a-b). The probability of a black triangle arising between a properly contoured restoration and the adjacent tooth increases with greater observable crestal bone loss on adjacent roots. Therefore, clinical situations with reduced vertical bone at adjacent teeth are still challenging and cannot be controlled by the surgeon, since surgical techniques are still not available to predictably regain this lost bone.
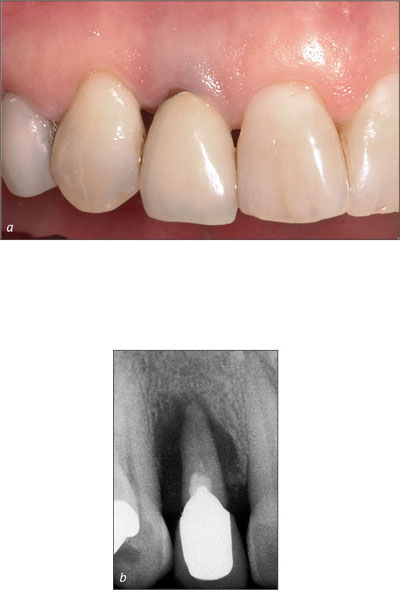
Figs 5a-b A reduced vertical bone height at an adjacent root surface is a significant risk factor and will affect the height of the papilla following implant therapy. In this female patient, the bone defect was caused by a large periapical lesion.
Local infection at implant site. The presence of infection in the entire dentition or just at the future implant site is an important aspect to be examined during preoperative analysis. It has been established for many years that untreated periodontitis should be addressed before initiating implant therapy (Mombelli and Lang, 1992), since periodontally diseased teeth could cause a potential cross-infection to the implant site. Local infections caused by endodontic lesions, post-traumatic lesions (root fractures, root resorption, and/or ankylosis), or foreign bodies (amalgam remnants, infected root remnants), are considered transient risk factors (Figs 6a-b), since they can cause post-surgical complications if implants are inserted in these infected sites. Sites with acute infection including exudate or pus flow are considered high-risk, whereas chronic infections are considered medium-risk.
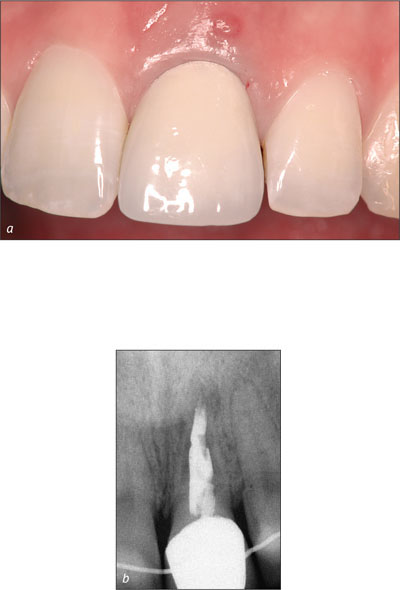
Figs 6a-b Infection with a fistula at tooth 21. The infection is caused by a post-traumatic root resorption. Immediate placement (Type 1) is not recommended.
There is, however, still controversy about whether implants placed in extraction sockets with periapical lesions have an increased rate of early failures. One prospective, randomized clinical study clearly demonstrated an increased failure rate (Lindeboom and coworkers, 2006), whereas a different study did not indicate a difference (Siegenthaler and coworkers, 2007). The more rational approach seems to be to delay implant placement in sites with acute lesions with pus flow or periapical fistulas.
Restorative status of neighboring teeth. When teeth adjacent to a single-tooth gap are virgin from a restorative point of view, no additional risk to the esthetic treatment outcome is anticipated. However, a serious risk is present if adjacent teeth have existing restorations that extend into the gingival sulcus. Such subgingival margins often cause recession following implant placement, leading to exposed restorative margins or altered gingival contours. For these patients, the replacement of the adjacent restoration is often part of the treatment plan, or modifications of the surgical incision are made to reduce the risk.
Width of edentulous space. The chances of an esthetic treatment outcome are better for an implant-supported single-tooth replacement than for clinical situations with multiple missing adjacent teeth (Belser and coworkers, 1996; Belser and coworkers, 1998; Buser and coworkers, 2004). As already pointed out above, the presence or absence of interproximal papillae depends mainly on the bone levels at adjacent root surfaces. In a single-tooth gap, the mesiodistal gap size must be sufficient to ensure a minimal distance of 1.0 to 1.5 mm between the implant shoulder and adjacent roots (Buser and coworkers, 2004). Sites with multiple missing teeth in the anterior maxilla will be discussed in a separate ITI Treatment Guide, since this clinical situation clearly represents a high esthetic risk.
Soft-tissue anatomy. The presence of soft-tissue deficiencies is most often associated with the presence of either horizontal and/or vertical bone deficiencies (Fig 7).

Fig 7 Female patient with a vertical soft-tissue defect at the ankylosed tooth 21, which has to be removed. The tissue deficit is combined with a thin tissue biotype, a delicate combination with high risk.
Experimental and clinical studies have clearly shown that the concept of biologic width applies to dental implants as it does to natural teeth. This means that the peri-implant soft tissues have rather constant dimensions in terms of thickness (Berglundh and Lindhe, 1996; Cochran and coworkers, 1997; Kan and coworkers, 2003b). The key in solving these soft-tissue deficiencies at the implant site is either successful bone-augmentation simultaneously with or prior to implant placement or soft-tissue augmentation simultaneously with or prior to implant placement using connective-tissue grafts. Both techniques are routinely used, sometimes even combined. A critical factor to consider is gingival recession at adjacent teeth. Standard techniques from mucogingival surgery are required to improve the esthetic outcome.
Bone defect at the implant site. This is an important category. Three groups have been classified by Martin and coworkers (2006). A healed site without bone defect is considered low-risk. A healed post-extraction site or a site with a horizontal defect is considered medium-risk, since surgical procedures are available today to successfully augment these defects with high predictability and a low risk of complications. A well-documented surgical procedure to resolve these horizontal deficiencies is the guided bone regeneration (GBR) technique, used either simultaneously with implant placement (Nyman and coworkers, 1990; Simion and coworkers, 1997) or as a staged approach that first rebuilds the alveolar ridge (Buser and coworkers, 1996; von Arx and Buser, 2006). Today, this procedure is referred to as contour augmentation, since this term describes precisely the primary objective of the bone-augmentation procedure. Successful contour augmentation is achieved when (i) bone is successfully regenerated at the implant-bone interface on the facial aspect and (ii) the contour is sufficiently augmented to mimic the root eminence of a natural tooth (Buser and coworkers, 2008).
In post-extraction sites, the socket morphology is of importance, in particular the status of the facial bone wall at extraction. This wall can be missing due to a local infection or trauma (Fig 8a). In this situation, bone augmentation is imperative. If the facial wall is thin (≤ 1 mm), which is a frequent clinical situation (Fig 8b), this bone will resorb within 4 to 8 weeks leading to a horizontal, crater-shaped bone defect and a loss of bone height on the facial aspect.

Figs 8a-c These three radiographs illustrate the various conditions of the facial bone wall prior to extraction: (a) the facial bone wall can be completely missing due to an ongoing local infection such as a peri-apical lesion; (b) the facial bone wall can be very thin (≤ 1 mm), which is most often the case in the anterior maxilla; and (c) the facial bone wall can be rather thick (> 1 mm), which is rarely the case in the anterior maxilla.
This has been documented both in experimental and clinical studies (Araújo and Lindhe, 2005; Nevins and coworkers, 2006; Schropp and coworkers, 2003b). As a consequence, contour augmentation has to be performed simultaneously with implant placement. In the case of a thick facial wall (> 1 mm; Fig 8c), the wall will not be resorbed to the same extent, and minimal loss in bone height will occur. However, the bone wall will undergo some bone-modeling changes leading to a significant flattening of the facial contour after 6 months of bone healing (Botticelli and coworkers, 2004). Summarizing these different clinical scenarios, contour augmentation by GBR seems to be indicated most often when the esthetic outcome needs to be optimized.
Vertical bone deficiencies at the implant site are most demanding in the anterior maxilla from a surgical point of view; they are considered high-risk. Fortunately, these situations are not often encountered in post-extraction sites in the anterior maxilla. When present, these are most often post-traumatic sites with an ankylosed tooth in an apical malposition (Fig 9) or at teeth that have suffered bone loss from advanced chronic periodontitis.

Fig 9 Significant vertical bone and soft tissue defect due to an ankylosed tooth in an apical malposition. Tooth extraction will cause a large tissue defect.
To a certain extent, GBR can be successfully used for vertical-ridge augmentation (Simion and coworkers, 1998; Simion and coworkers, 2007). However, the surgical procedure is very difficult and complex and bears a high risk of complications with soft-tissue dehiscences. This surgical technique thus ought to be reserved for highly experienced clinicians with the necessary skills and a large patient pool offering sufficient patient flow for the clinician to gain experience with such difficult procedures and to establish reliable treatment routine.
In posterior sites, bone height can be clearly reduced either by significant atrophy of the alveolar crest or by extended pneumatization of the maxillary sinus. In the posterior mandible, vertical atrophy of this type is rarely encountered in post-extraction sites. Significant vertical atrophy is most often seen in patients who have been wearing removable partial dentures for years with saddle-type distal extensions. However, in the posterior maxilla, a reduced bone height is frequently seen in post-extraction sites due to a crestal extension of the sinus floor (Figs 10a-b). In such sites, the timing of implant placement is heavily influenced by this anatomical restriction, since a sinus floor elevation has to be performed at an appropriate time point.

Figs 10a-b Reduced bone height in area 16 does not allow immediate (Type 1) or early implant placement (Type 2 or 3), since primary implant stability could not be achieved. In consequence, a healing period of at least 6 months following extraction is recommended to regenerate the alveolar crest that will then provide primary implant stability.
3.1.3 The Biomaterial
For post-extraction implant placement, three groups of biomaterials are required in most instances: the implant itself, barrier membranes, and bone fillers to regenerate peri-implant bone defects.
For all three groups of biomaterials, the scientific documentation plays an important role for the selection if the risk of unexpected complications and negative treatment outcomes is to be kept low. Biomaterials should be well documented – not only in experimental studies but also in clinical studies.
A detailed discussion about different implant types, membranes, or bone fillers cannot be provided here, as this would be beyond the scope of this ITI Treatment Guide. Instead, an overview will be offered on relevant characteristics of these biomaterials and on why they are important for clinical use.
Implant characteristics. Concerning the selection of an appropriate implant, there are a number of well-documented and well-tested implant systems on the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


