CHAPTER 29
Temporomandibular Joint Imaging
Joshua Stone1 and Christopher J. Haggerty2
1Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
2Private Practice, Lakewood Oral and Maxillofacial Surgery Specialists, Lees Summit; and Department of Oral and Maxillofacial Surgery, University of Missouri–Kansas City, Kansas City, Missouri, USA
Indications
- Evaluation of intra-articular abnormalities (internal derangement)
- Evaluation of lockjaw
- Preoperative evaluation of a dysfunctional joint
- Evaluation of soft tissue changes associated with inflammatory arthritides
Contraindications
- Implantable metal devices (indwelling pacemakers, intracranial vascular clips, etc.) and foreign body fragments are contraindications for magnetic resonance imaging (MRI)
- Documented allergy to contrast. Patients with impaired renal function are also contraindicated to receiving intravascular contrast
- Pregnancy
Relative Contraindications
- Obesity
- Claustrophobia
- Inability to remain motionless
Definitions
- Internal derangement: An abnormal relationship involving the articular disc, condyle, and articular eminence.
- Magnetic resonance imaging (MRI): A non-ionizing radiation modality utilizing magnetic frequencies and radiofrequencies in image generation. MRI provides cross-sectional multiplanar images that illustrate both soft and osseous tissue abnormalities of the joint, surrounding structures, and dynamic assessment of condylar translation and disc movement (with open and closed views).
- T1-weighted MRI images: The anatomy of the temporomandibular joint (TMJ) is clearly defined, and the articular disc is distinctly visible. Fluids are hypointense, whereas fats are hyperintense.
- T2-weighted MRI images: Useful for visualizing degenerative periarticular changes and the presence of joint effusions. Fluids are hyperintense in T2-weighted images.
- Technitium-99m (T99m) bone scan: T99m is a radioactive compound, which is useful in determining active bone metabolism. The compound uptake depends on osseous blood flow and osteogenesis. Common uses include utilization in determining active condylar growth (i.e., condylar hyperplasia) and bone tumors.
- Postgadolinium dynamic enhancement: Contrast agent used to enhance retrodiscal inflammation. Gadolinium can cause nephrogenic systemic fibrosis (i.e., nephrogenic fibrosing dermatopathy) in patients with diminished renal function.
Anatomy
- Articular disc: Composed of dense fibrous connective tissue that is nonvascular and non-innervated. The articular disc can be divided into three distinct regions: a thickened anterior and posterior band, and a central intermediate zone. The three distinct regions of the articular disc contribute to the bowtie morphology as seen in sagittal T1-weighted closed-mouth MRI images. The central intermediate zone is the thinnest area, and the area under function between the condylar head and the articular eminence during translation. The posterior band is the thickest area and attaches to the retrodiscal tissues. The normal position of the posterior band in relation to the condyle is the 12 o’clock position in open and closed views. The normal position of the central intermediate zone in relation to the condyle is the 10 o’clock position in the open and closed views.
- Retrodiscal tissues: The posterior band of the articular disc is continuous with the highly innervated and highly vascular retrodiscal tissues located within the bilaminar zone. Compression of the retrodiscal tissue is a potential source of TMJ discomfort.
- Bilaminar zone: Posteriorly the disc blends with the bilaminar zone, which is composed of the superior and inferior retrodiscal lamina.
- Superior retrodiscal lamina: Composed predominately of elastic fibers, which provide the posterior attachment of the articular disc to the tympanic plate and to the external auditory canal perichondrium. Functions to resist extreme translatory disc movements.
- Inferior retrodiscal lamina: Composed of dense, longitudinally oriented fibers that attach the articular disc to the posterior condyle. Functions in preventing extreme rotation of the disc with rotational movements of the condyle.
Figure 29.1 shows the articular disc in its normal position.
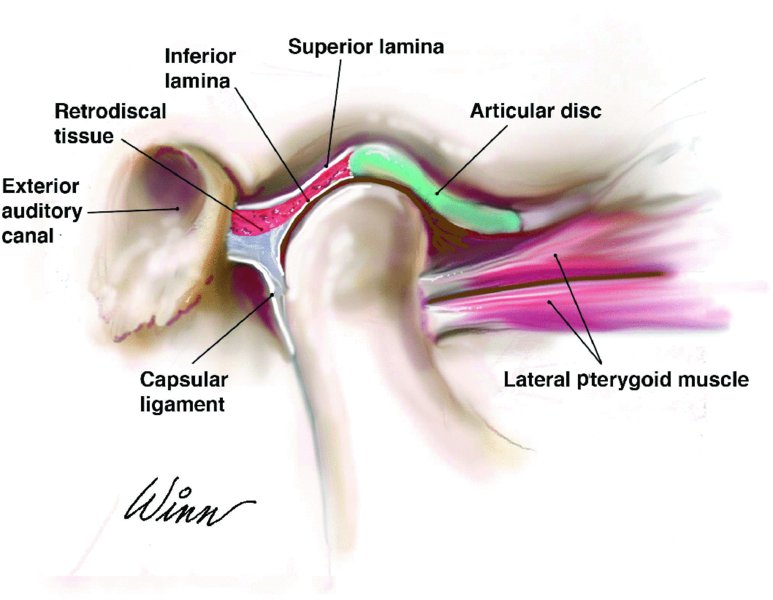
Figure 29.1. Illustration depicting the normal position of the disc and associated structures on sagittal closed-mouth view.
Five Temporomandibular Joint Ligaments
-
Medial and lateral collateral (discal) ligament: Attaches the articular disc to the medial and lateral condylar head (see Figure 29.4 in Case Report 29.1). Separates the joint into superior and inferior compartments. Allows the disc to rotate on the condylar head.
- Capsular ligament: Attaches to the condylar head anteriorly, posteriorly, medially, and laterally to surround the entire joint maintaining the synovial fluid compartment. Originates superiorly from the articular fossa and inserts inferiorly to surround the condylar head. Prevents inferior distracting forces of the condyle.
- Temporomandibular ligament: Originates at the articular tubercle and zygomatic process, and inserts along the lateral pole and lateral aspect of the condyle. Limits inferior distraction and posterior movement of the condyles.
- Sphenomandibular ligament: Originates from the spine of the sphenoid bone and inserts onto the lingula. Provides medial support of the TMJ.
- Stylomandibular ligament: Originates from the styloid process and inserts onto the angle of the mandible. Limits protrusive mov/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


