Mandibular and Maxillary Implant Overdenture Design and Fabrication
Carl E. Misch
The average total edentulous rate around the world is 20% of the adult population by age 65 years, although there is wide disparity from the countries with the highest and lowest rates.1 For example, from the 65- to 74-year age group, the total edentulous rate in Kenya and Nigeria was 4%, but the Netherlands and Iceland have rates of 65.4% and 71.5%, respectively. The edentulous rate in Canada was 47% at 65 to age 69 years and 58% from ages 70 to 98 years (with Quebec at 67% for those older than age 65 years compared with Ontario with a 41% rate).
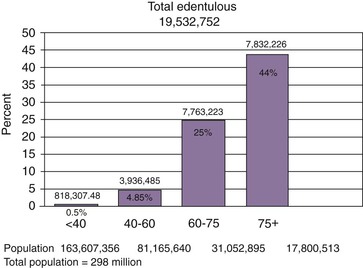
A 1999 to 2002 survey found that total edentulism in the United States of both arches was present in almost 20 million people.2 As expected, older persons are more likely to be missing all of their teeth. Total edentulism has been noted in 5% of employed adults ages 40 to 44 years, gradually increasing to 26% at age 65 years and almost 44% in seniors older than age 75 years3 (Figure 29-1). Gender was not found to be associated with tooth retention or tooth loss after adjustments were made for age.
The maxillary arch may be completely edentulous, opposing at least some teeth in the mandible. This condition occurs 35 times more often than the reverse situation. At age 45 years, 11% of the population has maxillary total edentulism opposing at least some teeth, which increases to 15% by 55 years of age and then remains relatively constant.2,3 Therefore, an additional 12 million individuals in the United States have total edentulism in the maxillary arch, representing 7% of the adult population overall.
The percentages of one or two arch total edentulism translate into more than 30 million people or about 17% of the entire U.S. adult population.4 To put these numbers in perspective, 30 million people represent approximately the entire U.S. African American population, the U. S. Hispanic population, the whole population of Canada, or the total population in the United States older than 65 years of age.
Although the edentulism rate is decreasing every decade, the elderly population is rising so rapidly that the adult population in need of one or two complete dentures will actually increase from 33.6 million adults in 1991 to 37.9 million adults in 2020. The total numbers of edentulous arches were estimated at 56.5 million in 2000, 59.3 million in 2010, and 61 million in 2020.5 Complete edentulism, therefore, remains a significant concern, and affected patients often require implant dentistry to solve several related problems. If four implants were used to help support each complete edentulous arch, a total of 226 million implants would be required. Yet only 10 million implants in the United States were inserted in 2010 for all patient treatment.
The vast majority of completely edentulous patients are treated with complete dentures. Despite these numbers, almost 70% of dentists spend less than 1% to 5% of their treatment time on edentulous patients, leaving a great unfulfilled need for implant dentistry. However, the dental profession and the public are more aware of the problems associated with a complete mandibular denture than any other dental prosthesis.
The placement of implants enhances the support, retention, and stability of an overdenture. As a result, edentulous patients are very willing to accept a treatment plan for a mandibular implant overdenture (IOD). There is greater flexibility in implant position or prosthesis fabrication with a mandibular IOD. As a result, it is also an ideal treatment modality to begin an early learning curve in implant surgery and prosthetics. Therefore, one of the most beneficial treatments rendered to patients is also one of the best introductions for a dentist into the discipline of implant dentistry.
An increased awareness from the profession and patients has now rendered the mandibular IOD the treatment of choice for edentulous patients regardless of most clinical situations, bone densities, and patients’ desires to restore an ever-growing number of patients.6–43 As a consequence, mandibular overdentures have become the minimum standard of care for most completely edentulous mandibles.38
Anatomical Consequences of Edentulism
There are many negative consequences for completely edentulous patients. They include continued bone loss of the jaws; soft tissue consequences that support the prostheses; facial esthetic consequences of bone loss; decreased masticatory performance, resulting in diet-related health issues; and psychological aspects of a total tooth loss (Box 29-1). Some of these issues are addressed in Chapter 1. Other related issues to overdentures are reviewed in this chapter.
Bone Loss
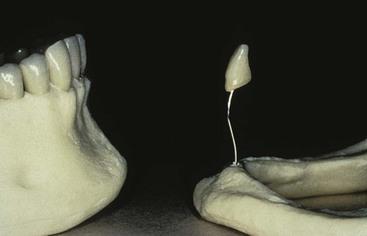
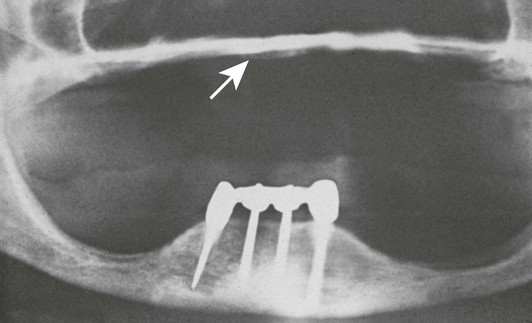
Wolff’s law (1892) states that bone remodels in relationship to the forces applied.44 Every time the function of bone is modified, a definite change occurs in the internal architecture and external configuration.45 In dentistry, the consequences of complete edentulism and remaining bone volume were noted by J. Misch in 1922, where he described the skeletal structure of a 90-year-old woman without teeth for several decades46 (Figure 29-2).
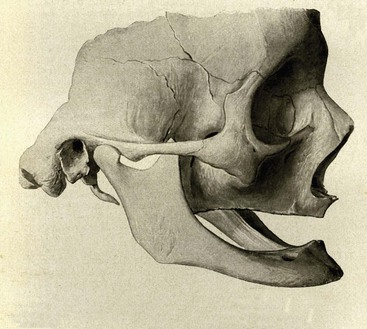
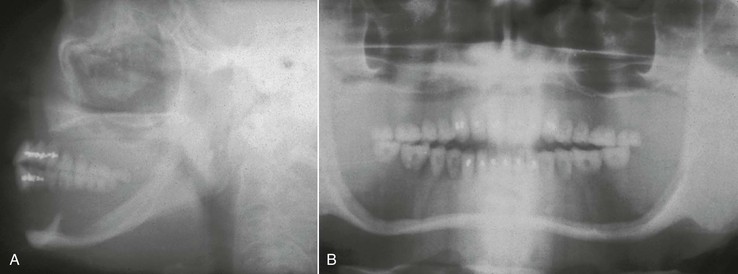
Bone needs stimulation to maintain its form and density. Roberts et al. report that a 4% strain to the skeletal system maintains bone and helps balance the resorption and formation phenomena.47 Teeth transmit compressive and tensile forces to the surrounding bone. These forces have been measured as a piezoelectric effect in the imperfect crystals of durahydroxyapatite that comprise the inorganic portion of bone.48 When a tooth is lost, the lack of stimulation to the residual bone causes a decrease in trabeculae and bone density in the area, with loss in the external width and then height of the bone volume.49 There is a 25% decrease in width of bone during the first year after tooth loss and an overall 4-mm decrease in height during the first year after extractions for an immediate denture.50 In a longitudinal 25-year study of edentulous patients, lateral cephalograms demonstrated continued bone loss during this time span, with a fourfold greater loss observed in the mandible.51 In 1963, Atwood introduced five different stages of bone loss in an anterior mandible after tooth loss52 (Figure 29-3).

Although the bone loss issue has been noted for a hundred years, the dental profession has most often overlooked the insidious bone loss that occurs after tooth extraction. The patient is often not educated about the anatomical changes and the potential consequences of continued bone loss. The bone loss accelerates when the patient wears a poorly fitting soft tissue–borne prosthesis. Patients do not understand that bone is being lost over time and at a greater rate beneath poorly fitting dentures. Patients do not return for regular visits for evaluation of their condition; instead, they return after several years when denture teeth are worn down or can no longer be tolerated. In fact, the average denture wearer sees a dentist every 14.8 years after having a complete denture. Hence, the traditional method of tooth replacement (dentures) often negatively affects bone loss in a manner not sufficiently considered by the dentist and the patient. The doctor should inform the patient that a denture replaces more bone and soft tissue than teeth, and every 5 years a reline or new denture is suggested to replace the additional bone loss by the atrophy that will occur (Figure 29-4).
Preventive dentistry has traditionally emphasized methods to decrease tooth loss or the surrounding bone supporting a tooth. This bone loss around a tooth is often monitored by the millimeter, yet no therapy had been promoted and accepted by the profession to avoid the bone changes resulting from tooth loss. The bone changes after total tooth loss may be measured by the centimeter. Today the profession must consider the loss of both teeth and bone. The loss of teeth causes remodeling and resorption of the surrounding residual bone and eventually leads to atrophic edentulous ridges.
Almost every girl and woman past the age of 14 years is aware of osteoporosis after menopause. Diet and exercise are encouraged their whole lives to decrease this risk. Yet osteoporosis primarily affects bone density, not bone volume. The only place in the body bone volume is lost to an extreme is in the jaws after tooth loss. Yet nobody in the public and very few in the profession ever address this issue. It is malpractice if a dentist does not monitor the bone loss around teeth by the millimeter with a probe. Yet the centimeter bone losses of the edentulous regions are often ignored.53
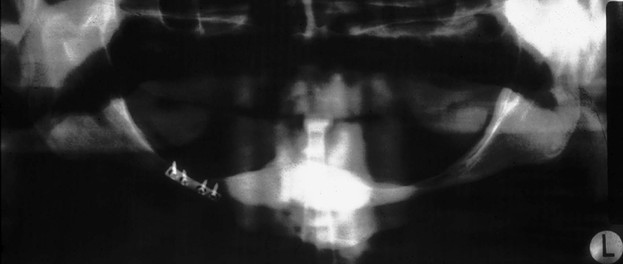
Consequences of edentulous ridges with bone loss are associated with anatomical problems that often impair the predictable results of traditional dental therapy. Several of these anatomical problems are listed in Box 29-2. Loss of bone in the maxilla or mandible is not limited to alveolar bone; portions of the basal bone may also be resorbed (Figure 29-5), especially in the posterior aspect of the mandible, where severe resorption may result in more than 80% bone loss.54 The contents of the mental foramen or mandibular canal eventually become dehiscent and serve as part of the support area of the prosthesis.55 As a result, acute pain and transient to permanent paresthesia of the areas supplied by the mandibular nerve are possible. The body of the mandible also is at increased risk of fracture even under very low impact forces (Figure 29-6). The mandibular fracture causes the jaw to shift to one side and makes stabilization and an esthetic result most difficult to obtain during treatment of the fracture.
The average denture patient does not see a dentist regularly. In fact, more than 10 years usually separates dental appointments of edentulous patients. As a consequence, the patient is unaware of the insidious loss of bone in the edentulous jaw. The bone loss that occurs during the first year after tooth loss is 10 times greater than in following years. In the case of multiple extractions, this often means a 4-mm vertical bone loss within the first 6 months. This bone loss continues over the next 25 years, with the mandible experiencing a fourfold greater vertical bone loss than the maxilla.56,57 During the long hiatus between dental visits after dentures are used to replace the dentition, the amount of resorption from initial denture delivery to the next professional interaction already has caused the destruction of the original alveolar process.
The anterior residual alveolar process also continues to resorb during this time frame, and the superior genial tubercles (which are 20 mm below the crest of bone when teeth are present) eventually become the most superior aspect of the anterior edentulous ridge. The more often a patient wears a denture, the greater the bone loss, yet 80% of denture patients wear their dentures day and night.
Soft Tissue Consequences
The loss of bone first causes decreased bone width. The remaining narrow residual ridge often causes discomfort when the thin overlying tissues are loaded under a soft tissue–borne removable prosthesis (RP). As bone loses width, then height, then width and height again, the attached gingiva gradually decreases. A very thin attached tissue usually lies over the advanced atrophic mandible or is entirely absent. The increasing zones of mobile, unkeratinized gingiva are prone to abrasions caused by the overlaying prosthesis. In addition, unfavorable high muscle attachments and hypermobile tissue often complicate the situation.
As the bony ridge resorbs in height, the muscle attachments become level with the crest of the edentulous ridge (Figure 29-7). The continued atrophy of the posterior mandible eventually causes prominent mylohyoid and internal oblique ridges covered by thin, movable, unattached mucosa. There is little to prevent the prosthesis from moving forward against the lower lip during function or speech. This condition is further compromised by the vertical movement of the distal aspect of the prosthesis during contraction of the mylohyoid and buccinator muscles and the anterior incline of the atrophic mandible compared with that of the maxilla.58 Yet these compromised tissues are the support and stability system of the denture (Box 29-3).
Masticatory Function
The difference in maximum occlusal forces recorded in a person with natural teeth and one who is completely edentulous is dramatic. In the first molar region of a dentate person, the average force has been measured at 150 to 250 psi.59 A patient who grinds or clenches the teeth may exert a force that approaches 1000 psi. The maximum occlusal force in the edentulous patient is reduced to less than 50 psi. The longer patients are edentulous, the less force they are able to generate. Patients wearing complete dentures for more than 15 years may have a maximum occlusal force of less than 6 psi.60
As a result of decreased occlusal force and the instability of the denture, masticatory efficiency also decreases with tooth loss. Ninety percent of the food chewed with natural teeth fits through a no. 12 sieve; this is reduced to 58% in a patient wearing complete dentures.61 A study of 367 denture wearers (158 men and 209 women) found that 47% exhibited low masticatory performance.62 The 10-fold decrease in force and the 40% decrease in efficiency affect the patient’s ability to chew. Lower intakes of fruits, vegetables, and vitamin A by women are noted in this group. Denture patients also take significantly more drugs (37%) compared with those with superior masticatory ability (20%), and 28% take medications for gastrointestinal disorders.63 The reduced consumption of high-fiber foods could induce gastrointestinal problems in edentulous patients with deficient masticatory performance. In addition, the coarser bolus may impair proper digestive and nutrient extraction functions.
Mandibular discomfort was listed in a study by Misch and Misch with equal frequency as movement (63.5%), and surprisingly, 16.5% of the patients stated they never wear the mandibular denture.64 In comparison, the maxillary denture was uncomfortable half as often (32.6%), and only 0.9% were seldom able to wear the prosthesis. Function was the fourth most common problem reported by these 104 denture wearers. In persons with dentures, 29% are able to eat only soft or mashed foods; 50% avoid many foods; and 17% claim they eat more efficiently without the prosthesis.64 The psychological effects of the inability to eat in public can be correlated with these findings. Other reports agree that the major motivating factors for patients to undergo treatment were related to the difficulties with eating, denture fit, and discomfort63 (Box 29-4).
Advantages of an Implant Overdenture
The use of dental implants to provide support for an IOD offers many advantages compared with the use of removable soft tissue–borne restorations (Box 29-5). A primary reason to consider dental implants to replace missing teeth is the maintenance of alveolar bone. The most common position to insert implants for an overdenture is in the anterior mandible. After the implants are inserted, the anterior bone under an overdenture may resorb as little as 0.6 mm vertically over 5 years, and long-term resorption may remain at less than 0.05 mm per year.35,40 Stress and strain may be applied to the bone surrounding the implant. As a result, the decrease in trabeculation and volume of bone that occurs after tooth extraction is reversed. There is an increase in bone trabeculae and density when the dental implant is inserted and functioning. The overall volume of bone around the implants is also maintained. An endosteal implant can maintain bone width and height as long as the implant remains healthy.47 As with a tooth, periimplant bone loss may be measured in tenths of a millimeter and may represent a more than 20-fold decrease in lost bone structure compared with the resorption that occurs with removable prostheses.
The features of the inferior third of the face are closely related to the supporting skeleton. When vertical bone is lost, the dentures only act as “oral wigs” to improve the contours of the face. The dentures become bulkier as the bone resorbs, making it more difficult to control function, stability, and retention. With implant-supported prostheses, the vertical dimension may be restored, similar to natural teeth. In addition, the implant-supported prosthesis allows a cantilever of anterior teeth for ideal soft tissue and lip contour and improved appearance in all facial planes. This happens without the instability that usually occurs when an anterior cantilever is incorporated in a traditional denture. The facial profile may be enhanced for the long term with implants rather than deteriorating over the years as can occur with traditional dentures.
The complete mandibular denture often moves during mandibular jaw movements during function and speech. In addition to the lack of retention from bone loss, a mandibular denture often moves when the mylohyoid and buccinator muscles contract during speech or mastication. The maxillary teeth are often positioned for lower denture stability rather than where natural teeth usually reside. With implants, the maxillary teeth may be positioned to enhance esthetics and phonetics rather than in the neutral zones dictated by traditional denture techniques to improve the stability of a lower prosthesis.
Occlusion is difficult to establish and stabilize with a completely soft tissue–supported prosthesis. Because the mandibular prosthesis may move as much as 10 mm or more during function, proper occlusal contacts occur by chance, not by design.65,66 An implant-supported restoration is stable. The patient can more consistently return to centric relation occlusion rather than adopt variable positions dictated by the prosthesis’ instability.
Proprioception is awareness of a structure in time and place. The receptors in the periodontal membrane of the natural tooth help determine its occlusal position. Although endosteal implants do not have a periodontal membrane, they provide greater occlusal awareness than complete dentures. Whereas patients with natural teeth can perceive a difference of 20 microns between the teeth, implant patients can determine 50-micron differences with rigid implant bridges compared with 100 microns in those with complete dentures (either one or two).67 As a result of improved occlusal awareness, the patient functions in a more consistent range of occlusion.
With an implant-supported prosthesis, the direction of the occlusal loads is controlled by the restoring dentist. Horizontal forces on removable prostheses accelerate bone loss, decrease prosthesis stability, and increase soft tissue abrasions. Therefore, the decrease in horizontal forces that are applied to implant restorations improves the local parameters and helps preserve the underlying soft and hard tissues. An IOD provides improved retention and stability of the prosthesis, and the patient is able to consistently reproduce a determined centric occlusion.43
In a randomized clinical trial by Kapur et al., the implant group of patients demonstrated a higher level of eating enjoyment and improvement of speech, chewing ability, comfort, denture security, and overall satisfaction.68 The ability to eat several different foods among complete denture versus mandibular overdenture patients was evaluated by Awad and Feine.69 The IOD was superior for eating not only harder foods, such as carrots and apples, but also softer foods, such as bread and cheese. Geertman et al. evaluated complete denture wearers with severely resorbed mandibles before and after mandibular IODs. The ability to eat hard or tough foods significantly improved.70,71
Researchers at McGill University evaluated blood levels of 30 patients who had complete dentures and 30 patients with maxillary dentures opposing mandibular implant prostheses 6 months after treatment.72 Within this rather short period, implant patients had higher B12 hemoglobin (related to an iron increase) and albumin levels (related to nutrition). These patients also had greater body fat in their shoulders and arms, with decreased body fat in their waists. Beneficial effects such as a decrease in fat, cholesterol, and the carbohydrate food groups have been reported, as well as significant improvement in eating enjoyment and social life.73–75
The maximum occlusal force of a traditional denture wearer ranges from 5 to 50 lb. Patients with an implant-supported fixed prosthesis (FP) may increase their maximum bite force by 85% within 2 months after the completion of treatment. After 3 years, the mean force may reach more than 300% compared with pretreatment values.60 As a result, an implant prosthesis wearer may demonstrate a force similar to that of a patient with a fixed restoration supported by natural teeth.
Chewing efficiency with an implant prosthesis is greatly improved compared with that of a soft tissue–borne restoration. The masticatory performance of dentures, overdentures, and natural dentition was evaluated by Rissin et al., and the traditional denture showed a 30% decrease in chewing efficiency.61 The tooth-supported overdenture loses only 10% of chewing efficiency compared with natural teeth. These findings are similar with implant-supported overdentures. Geertman et al. reported similar results comparing chewing ability of conventional complete dentures with mandibular IODs.70,71 In addition, rigid implant-supported prostheses may function the same as natural teeth.
The stability and retention of an implant-supported prosthesis are great improvements over soft tissue–borne dentures. Mechanical means of implant retention are far superior to the soft tissue retention provided by dentures or adhesives and cause fewer associated problems. The implant support of the final prosthesis is variable, depending on the number and position of implants; yet all treatment options demonstrate significant improvement.
Phonetics may be impaired by the instability of a conventional denture. The buccinator and mylohyoid muscles may flex and propel the posterior portion of the denture upward, causing clicking, regardless of the vertical dimension.66 As a result, a patient in whom the vertical dimension already has collapsed 10 to 20 mm may still produce clicking sounds during speech. Often the tongue of the denture wearer is flattened in the posterior areas to hold the denture in position. The anterior mandibular muscles of facial expression may be tightened to prevent the mandibular prosthesis from sliding forward. The implant prosthesis is stable and retentive and does not require these oral manipulations. The implant restoration allows reduced flanges or palates of the prostheses. This is of special benefit to new denture wearers, who often report discomfort with the bulk of the restoration.
Patients treated with implant-supported prostheses judge their overall psychological health as improved by 80% compared with their previous state while wearing traditional, removable prosthodontic devices. They perceived the implant-supported prosthesis as an integral part of their body. For example, Raghoebar et al. evaluated 90 edentulous patients in a randomized multicenter study.76 Five years after treatment, a validated questionnaire targeted patient esthetic satisfaction, retention, comfort, and the ability to speak and eat with a complete mandibular denture, complete mandibular denture with vestibuloplasty, or mandibular two-implant overdenture. IODs had significantly higher ratings, but no significant difference was found between the two complete-denture groups.
For patients with the inability to afford a fixed implant prosthesis, the IOD is a significant improvement compared with their traditional denture. In a randomized clinical report, Awad et al. compared satisfaction and function in complete denture patients versus patients with two implant-supported mandibular IODs.11 There was significantly higher satisfaction, comfort, and stability in the IOD group. A similar study in a senior population yielded similar results.12 Thomason et al., in the United Kingdom, also reported a 36% higher satisfaction for the implant IOD patients than the complete denture wearers in the criteria of comfort, stability, and chewing.13
The success rate of implant prostheses varies, depending on a host of factors that change for each patient. However, compared with traditional methods of tooth replacement, the implant prosthesis offers increased longevity, improved function, bone preservation, and better psychological results.
Advantages of Implant-Supported Overdentures versus Fixed Prostheses
The IOD provides some practical advantages over the implant-supported complete fixed partial denture (Box 29-6). Fewer implants may be required when a RP-5 restoration is fabricated because soft tissue areas may provide additional support. The overdenture may provide stress relief between the superstructure and prosthesis, and the soft tissue may share a portion of the occlusal load. Regions of inadequate bone for implant placement therefore may be eliminated from the treatment plan rather than necessitating bone grafts or placing implants with a poorer prognosis. As a result of less bone grafting and number of implants, the cost to treat the patients is dramatically reduced.
The implant position is less specific for an overdenture compared with a FP. The cervical contours of the prosthesis are controlled by implant position in a fixed restoration. The implants have a greater demand for parallelism for a FP, especially when a cemented restoration is desired. The postoperative evaluation and hygiene of an IOD is easier than for a FP, especially when cervical ridge laps are used in the restoration.
The overdenture restoration is easier to repair because it is already readily removable. The FP may be difficult to remove when cement retained and even when screw retained takes considerable time and effort. The transitional restoration during fabrication of the final prosthesis is typically the complete denture the patient was wearing before treatment. A fixed restoration often requires an additional restoration to be fabricated during the treatment process.
The IOD may be removed at night to reduce the noxious effects of nocturnal parafunction. These cyclic forces increase the risk of biomechanical problems not only of the implants but also of the entire implant system, including the prosthesis occlusal material, the screws and cements that retain the prosthesis, the abutment screws, the crestal marginal bone, the complete bone–implant interface, and fracture of any of the prosthetic components or even the implants themselves.
An overdenture may be more esthetic than a FP, especially in the maxillary arch when the soft tissues of the face need additional support as a consequence of bone loss. Hygiene procedures are also not compromised when additional facial support is gained with a labial flange of the overdenture compared with the situation with a FP.
When cost is a factor, a two-implant–retained IOD may improve the patient’s condition at a lower overall treatment cost than a fixed implant–supported prosthesis. A survey by Carlsson et al. in 10 countries indicated a wide range of treatment options.19 The proportion of IOD selection versus fixed implant dentures was highest in the Netherlands (93%) and lowest in Sweden and Greece (12%). Cost was cited as the number one determining factor in the choice.
In conclusion, the primary indications for a mandibular IOD relate to problems found with lower dentures such as lack of retention or stability, decrease in function, difficulties in speech, tissue sensitivity, and soft tissue abrasions. If an edentulous patient desires a RP, an IOD is often the treatment of choice. If cost is a problem for a patient who desires a fixed restoration, the overdenture may serve as a transitional device until additional implants may be inserted and restored.
Disadvantages of Implant Overdentures
Implant overdentures also have disadvantages compared with fixed prostheses (Box 29-7). This aspect of overdenture treatment should be reviewed with the patient to reduce patient complaints after treatment. Whereas an overdenture is a prosthesis, a fixed restoration is considered a body part. Patients with an IOD respond, “These are much better than my denture.” When patients have a fixed restoration, they often state, “These are better than my teeth.”
A greater crown height space (CHS) is required for an overdenture. Hence, when abundant bone is present and implants are already inserted, a FP will have less issues of fracture or positioning teeth over a bar.
More maintenance is required for an overdenture. Attachments wear and need to be replaced, relines are necessary for RP-5 restorations, and denture teeth wear more rapidly on an IOD than a denture. As a result, a new IOD may need to be fabricated every 7 years.
A side effect of an IOD is food impaction under the prosthesis. The denture is border molded, so the muscles are in their contracted position. Otherwise, because the prosthesis is more rigid than a denture, sore spots develop during function. In the relaxed muscle state, food goes beyond the denture border. Then when the patient swallows, the food is pushed under the denture. Because the IOD moves less than a denture, the food remains under the IOD.
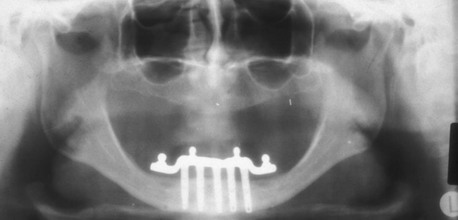
The majority of mandibular IODs used by the profession are supported by two implants anterior to the mental foramina and soft tissue support in the posterior regions (Figure 29-8). Yet posterior bone loss occurs four times faster than anterior bone loss.51,52 In a completely edentulous patient, the eventual paresthesia and mandibular body fractures are primarily from posterior bone loss. Dental implants placed in the anterior mandible help retain a lower denture and are a benefit over a complete denture. But the posterior bone loss will continue and may eventually lead to significant complications.77–79 The anterior implants allow improved anterior bone maintenance, and the prosthesis benefits from improved function, retention, and stability. However, the lack of posterior support in two- and three-implant overdentures allows continued posterior bone loss.
A primary concern for RP-5 overdentures (soft tissue support in the posterior regions) compared with RP-4 or fixed restorations (restorations completely supported, retained, and stabilized) should be the continued bone loss in the posterior regions. Not only does the posterior bone resorb faster than the anterior bone, but the implant prostheses with posterior soft tissue support may also accelerate posterior bone resorption two to three times faster than in a complete denture wearer.80 Therefore, the short-term benefit of decreased cost for RP-5 overdentures may be offset by the accelerated bone loss that is a primary consideration, especially in the younger edentulous patient (Figure 29-9).
Patients wearing complete fixed implant–supported prostheses show little to no posterior bone loss and usual occurrences of bone apposition. For example, studies by Davis et al.,81 Reddy et al.,82 Wright et al.,83 found that prostheses completely supported by implants in the edentulous mandible actually may increase the posterior bone volume (even though posterior implants are not inserted) (Figure 29-10). Misch has noted a similar condition of posterior and anterior bone maintenance with complete implant-supported overdentures even though no implants were positioned behind the mental foramina (Figure 29-11). He observed even grafts of iliac bone to the jaws, which usually resorb without dental implant insertion within 5 years, are instead stimulated and maintain overall bone volume in both the anterior and posterior regions while also maintaining implant integration. Therefore, the next progression in the implant philosophy is to convert all mandibular implant and soft tissue–supported restorations to a completely implant-supported prosthesis (fixed or removable).

In conclusion, the profession should treat bone loss after tooth extraction in a similar fashion as bone loss from periodontal disease. Rather than waiting until the bone is resorbed or the patient complains of problems with the prostheses, the dental professional should educate the patient about the bone loss process after tooth loss. In addition, the patient should be made aware that the bone loss process can be arrested by a dental implant. Therefore, most completely edentulous patients should be informed of the necessity of dental implants to maintain existing bone volume and improve prosthesis function, masticatory muscle activity, esthetics, and psychologic health.
From a bone volume conservation standpoint in the jaws, completely edentulous patients should be treated with enough implants to completely support a prosthesis whether the patient is partially or completely edentulous. The continued bone loss after tooth loss and associated compromises in esthetics, function, and health make all edentulous patients implant candidates. As a result, complete implant–supported restorations should be the restoration of choice.
As a consequence of continued posterior bone loss with a two- or three-implant overdenture, the recommendation is to consider a RP-5 prosthesis as an interim device designed to
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses