Binder Syndrome
Evaluation and Treatment
In 1939, Noyes first described a patient whose face was characterized by a flat nasal tip and a retruded maxillary–nasal base.32 He did not recognize this as an entity unique from other known forms of maxillary retrusion. It was not until 1962 that von Binder came to recognize the specific entity of nasomaxillary hypoplasia that is now called Binder syndrome.53 He described physical findings of nasomaxillary hypoplasia, a convex lip, a vertical (short) nose, a flat frontonasal angle, an absent anterior nasal spine, limited nasal mucosa, and hypoplastic frontal sinuses. von Binder postulated that the hypoplasia was the result of a disturbance of the prosencephalic induction center at a critical phase during development. In 1989, Sheffield and colleagues reviewed 103 cases of chondrodysplasia punctata (CDP) seen in Melbourne, Australia, over a 20-year period.48 They concluded that Binder syndrome should be classified as a mild form of CDP. In 1991, Sheffield and colleagues pointed out that most patients with Binder syndrome seek medical attention during adolescence.47 By this age, the confirmatory diagnostic radiologic features of CDP have disappeared, so the diagnosis of CDP is often not considered. Older patients may show terminal phalangeal hypoplasia of the hand and variable anomalies of the vertebrae (i.e., vertebral clefting). Associated malformations of the cervical spine primarily affect the atlas and the axis without known clinical sequelae.35,43 Familial recurrence has been reported, and inheritance may occur as an autosomal recessive trait with incomplete penetrance.34 The syndrome may also be of a threshold character with a genetically multifactorial background.5,14,45
The physical findings of Binder syndrome result from hypoplasia of the anterior nasal floor (fossa praenasalis), and the anterior maxilla including the pyriform rim region.26,33 When viewing the nose–upper lip complex from the worm’s-eye perspective, typical variations from normal are described as a retracted columella–lip junction, a lack of normal triangular flare at the nasal base, a perpendicular alar–cheek junction, a convex flat nasal tip with a wide and shallow philtrum, crescent-shaped nostrils without a distinct sill, and a stretched and shallow cupid’s bow.27,41 Striking profile characteristics of the nose include vertical shortening of the columella, a lack of tip projection, perialar flattening, and an acute nasolabial angle.11,28 The dentition and occlusion in an untreated individual will typically demonstrate the proclination of the maxillary incisors, “peg” laterals, and a canine Angle class III negative overjet tendency.21
Anthropometric explanations for these findings were first suggested by Zuckerkandl in 1882, when he described an anomaly in the anterior nasal floor in which the normal crest that separates the nasal floor from the anterior surface of the maxilla was absent.56 Instead, a small pit—the fossa praenasalis—constituted the pyriform aperture.18,24 Other investigators have pointed out that the premaxilla of normal Caucasian individuals is incorporated into the upper arch.2,3 This results in a prominence or projection of the base of the nose. By contrast, when the premaxilla (i.e., the primary palate) is not incorporated into the arch (i.e., in higher primates, certain racial groups, persons with Binder syndrome, and individuals with bilateral clefted alveolar ridges and lips), there will be flattening of the premaxillary region and of the base of the nose.6 This is more commonly seen among African and Asian people.10
In an attempt to reconstruct the skeletal deformities associated with Binder syndrome, clinicians have suggested a spectrum of procedures, including Le Fort I osteotomy, Le Fort II osteotomy, Le Fort III osteotomy, and a combination of Le Fort I and II osteotomies.4,8,12,17,19,20,22,23,31,36,39,42,44,49,51,55 Augmentation of the infraorbital rims, the pyriform rims (paranasal), and the anterior maxilla with the use of a spectrum of materials have all been tried.7,25,40,50 Suggested nasal reconstructive options have included autogenous, homogenous, and allogenic bone and cartilage grafts that extend up the columella (i.e., from the base of the maxilla to the nasal tip) and over the nasal dorsum (i.e., from the radix to the tip).1,9,13,15,19,29,30,38,39,46,52 Suggested soft-tissue procedures include septal cartilage and mucosal flaps, upper lip to nasal skin flaps to lengthen the columella, and a variety of subcutaneous augmentation procedures and fillers.37,54 Compensating orthodontic or dental restorative work may also be undertaken.
With Binder syndrome, a degree of hypoplasia of the premaxilla and of the quadrangular cartilage of the nasal septum is a consistent finding. This author agrees with Holmstrom and colleagues that, with this anomaly, there is a local shortage of bone in the premaxillary region and an absence of cartilage in the anterior septum.18–20 However, as Tessier pointed out, there is no significant shortage of soft tissue available.50–51 Furthermore, modification of the uninvolved orbits, zygomas, and upper nasal dorsum (i.e., the nasal bones) is rarely indicated or advantageous. The observed facial features in an individual with Binder syndrome are dependent on the degree of hypoplasia of the anterior nasal floor (fossa paranasalis) present at the time of birth. The deformities are believed to be non-progressive with age.
Current Approach to Reconstruction
The approach to the correction of the Binder syndrome deformity is to plan for a staged reconstruction to coincide with facial and dental growth patterns and psychosocial needs.16,39 An analysis of each patient’s morphology is followed by a review of the reconstructive options with the patient and family. The most gratifying long-term functions (i.e., occlusion and breathing) and facial aesthetics are generally achieved when carrying out the reconstruction after the completion of growth and before the individual’s graduation from high school (Fig. 29-1 through 29-5). Orthodontic treatment should be coordinated with consideration of orthognathic correction and premaxillary augmentation to be followed by definitive nasal reconstruction. The ideal orthodontic treatment often includes maxillary first bicuspid extractions with retraction and alignment of the anterior teeth to produce ideal incisor inclination within solid basal bone. Unfortunately, many individuals with Binder syndrome will have already been treated with an orthodontic camouflage approach. During the process, the maxillary incisors are tipped facially, and the mandibular incisors are often retroclined. This will typically achieve successful neutralization of the occlusion (i.e., the correction of overjet), but it will leave the patient looking as if he or she has a maxillary deficiency. Attempts at surgical augmentation after orthodontic camouflage are generally suboptimal. When indicated, definitive orthognathic reconstruction is planned to idealize the vertical, transverse, and horizontal midface proportions. A Le Fort I osteotomy (horizontal advancement and a variable degree of vertical lengthening) is frequently combined with an osseous genioplasty (vertical shortening and horizontal advancement). Sagittal split ramus osteotomies are often needed to avoid the limitations inherent to mandibular autorotation. Further reconstruction involves the application of a crafted bone graft to the deficient premaxillary and pyriform rim regions. This is best accomplished simultaneously with the orthognathic procedures.
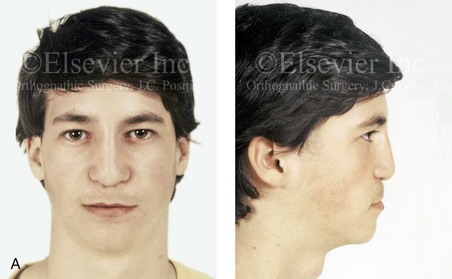
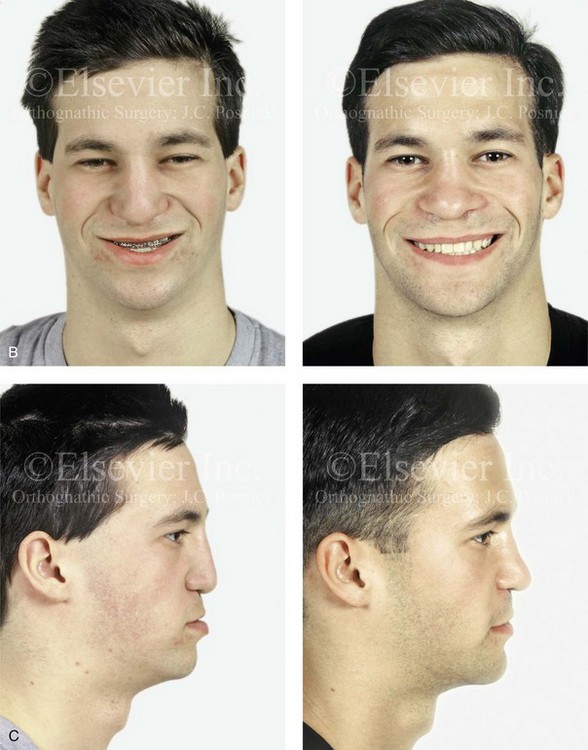
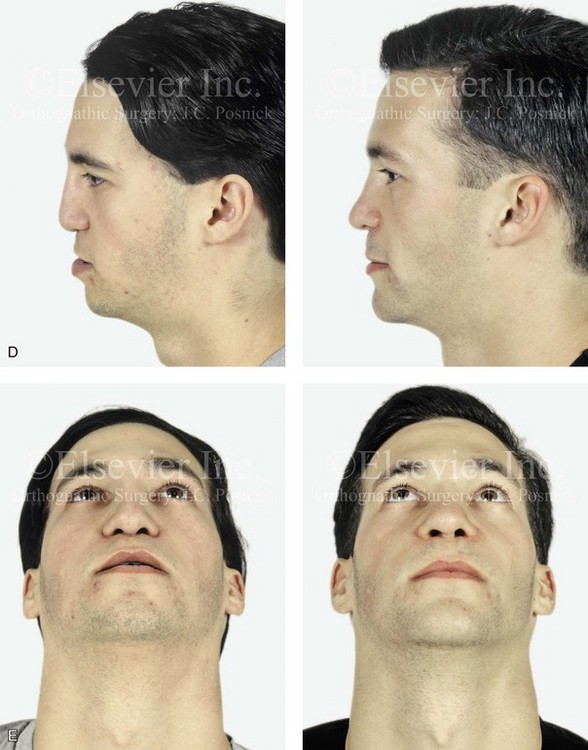
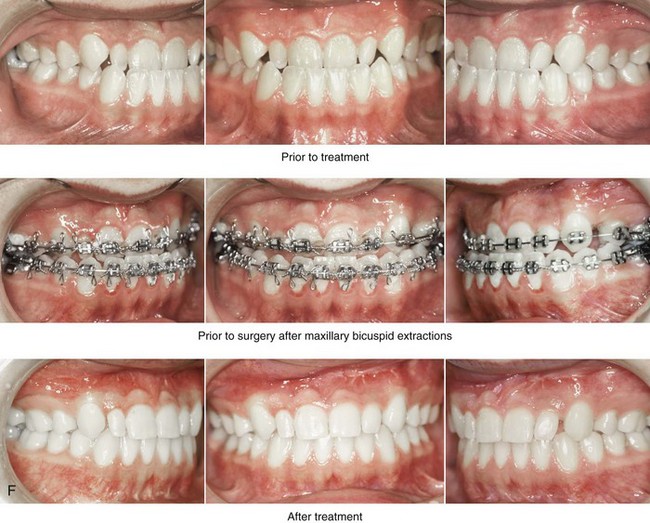
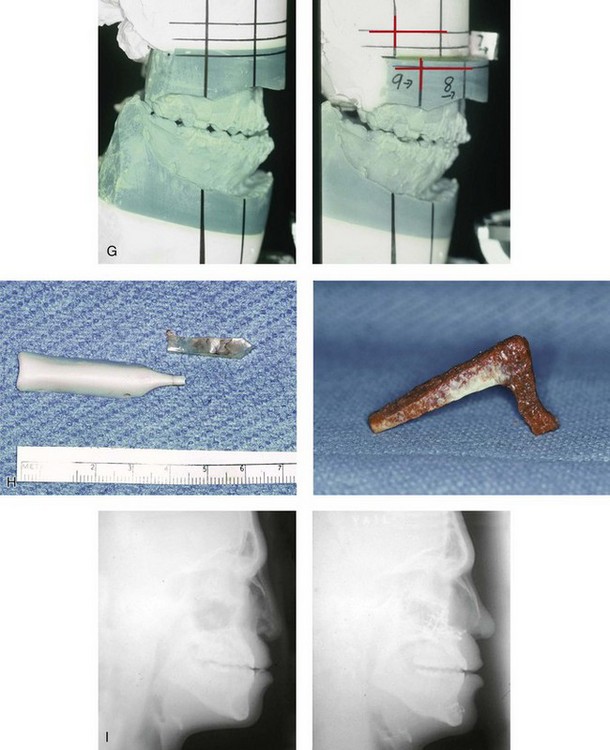
Figure 29-1 A 17-year-old boy, who was born with Binder syndrome was referred by his orthodontist for surgical evaluation. When he was 7 years old he underwent nasal augmentation with Silastic implants with another surgeon. Orthodontic treatment including maxillary first-bicuspid extractions and orthognathic and nasal surgery was chosen. The patient’s procedures included a Le Fort I osteotomy (horizontal advancement); the removal of nasal implants; osseous genioplasty (horizontal advancement); and nasal reconstruction (corticocancellous iliac graft). A, Facial views at 10 years old with Silastic implants in place. B, Frontal views with smile before and after reconstruction. C and D, Profile views before and after reconstruction. E, Worm’s-eye views before and after reconstruction. F, Occlusal views before and after reconstruction. G, Articulated dental casts that indicate analytic model planning. H, Intraoperative views of removed Silastic nasal implants. The crafted iliac corticocancellous bone graft before inset is also shown. I, Lateral cephalometric radiographs before treatment and after reconstruction. A (right), B, C, F, H, I, From Posnick JC, Tompson B: Binder syndrome: Staging of reconstruction and skeletal stability and relapse patters after Le Fort I osteotomy using miniplate fixation, Plast Reconstr Surg 99:967, 1997.


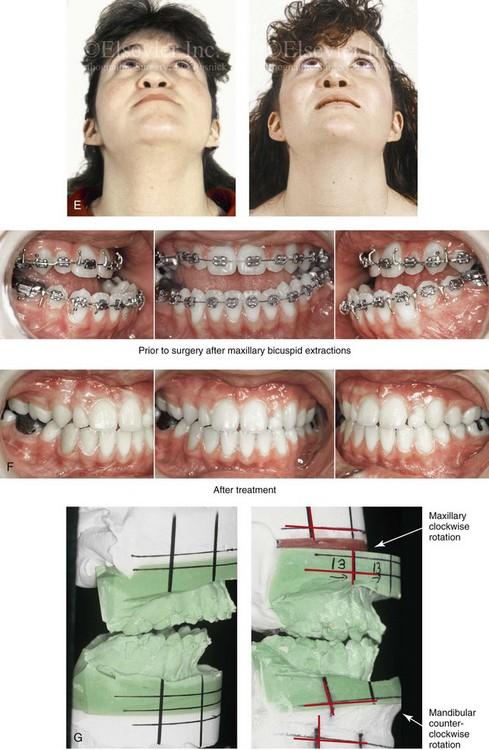
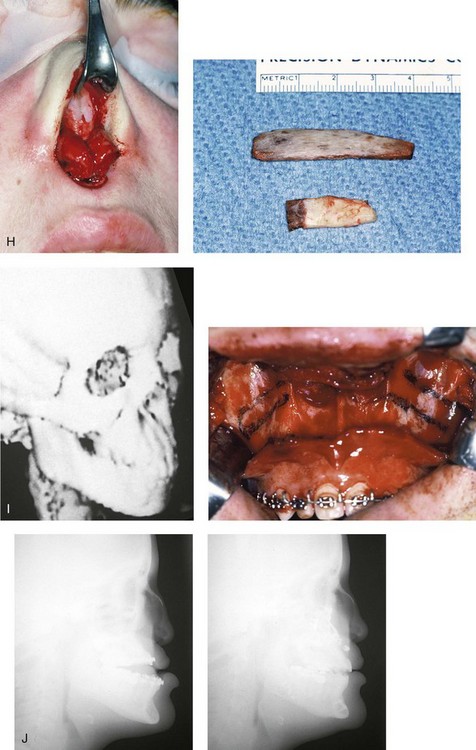
Figure 29-2 A 16-year-old girl who was born with Binder syndrome was referred by her orthodontist for surgical evaluation. She agreed to orthodontic treatment that included maxillary first bicuspid extractions and orthognathic and nasal surgery. The patient’s procedures included Le Fort I osteotomy (horizontal advancement); bilateral sagittal split ramus osteotomies; osseous genioplasty; and nasal reconstruction (autogenous rib graft). A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Worm’s-eye views before and after reconstruction. F, Occlusal views before and after reconstruction. G, Articulated dental casts that indicate analytic model planning. H, Intraoperative views of open rhinoplasty exposure. The rib bone (dorsal strut) and rib cartilage (caudal strut) grafts are shown before inset. I, Computed tomography scan and intraoperative views that confirm premaxillary hypoplasia consistent with Binder syndrome. J, Lateral cephalometric radiographs before and after reconstruction. B, F (top center and bottom center), H, From Posnick JC, Tompson B: Binder syndrome: Staging of reconstruction and skeletal stability and relapse patters after Le Fort I osteotomy using miniplate fixation, Plast Reconstr Surg 99:965, 1997.
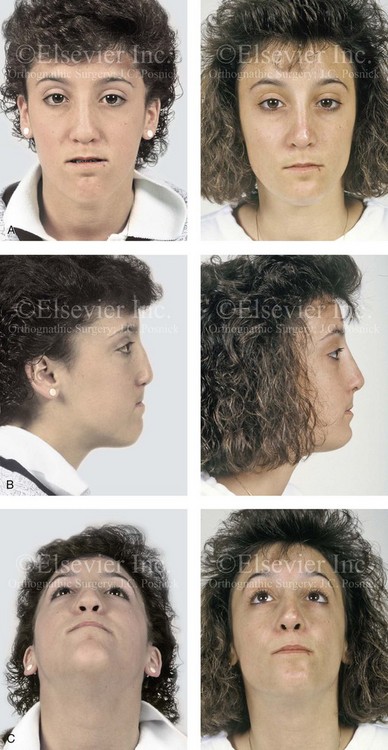
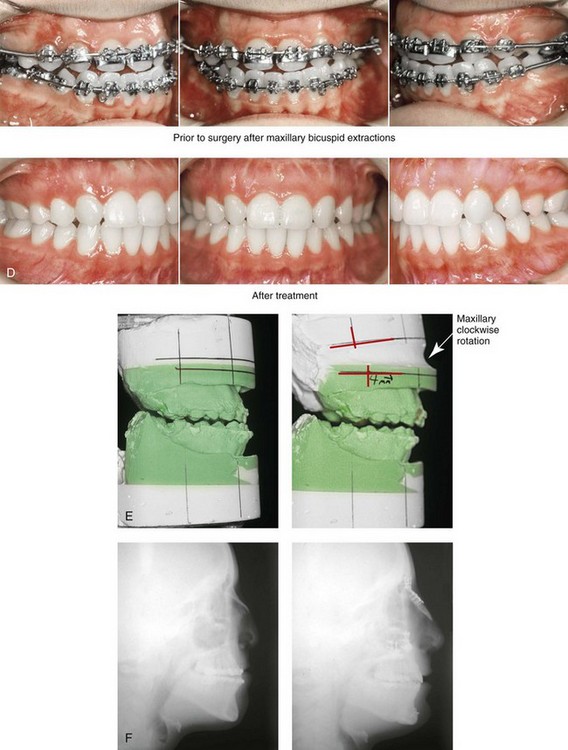
Figure 29-3 A 16-year-old girl who was born with Binder syndrome was referred by her orthodontist for surgical evaluation. She agreed to orthodontic treatment that included maxillary first bicuspid extractions and orthognathic surgery. The patient’s procedures included Le Fort I osteotomy (horizontal advancement); osseous genioplasty (horizontal advancement); and nasal reconstruction. The nasal reconstruction (cranial graft) was complicated by pressure necrosis of the nasal tip skin, which necessitated the removal of the distal aspect of the graft. Six months later, through an open rhinoplasty approach, autogenous rib cartilage (a caudal strut) was used to revise the nasal tip. A, Frontal views in repose before and after reconstruction. B, Profile views before and after reconstruction. C, Worm’s-eye views before and after reconstruction. D, Occlusal views during orthodontics and after reconstruction. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction.

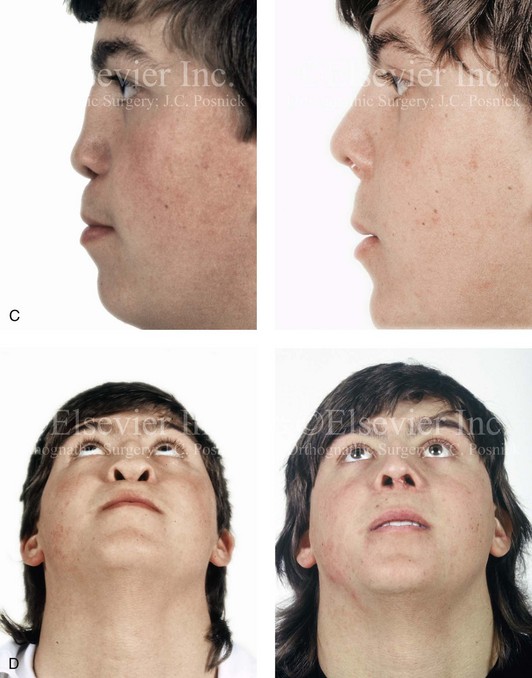
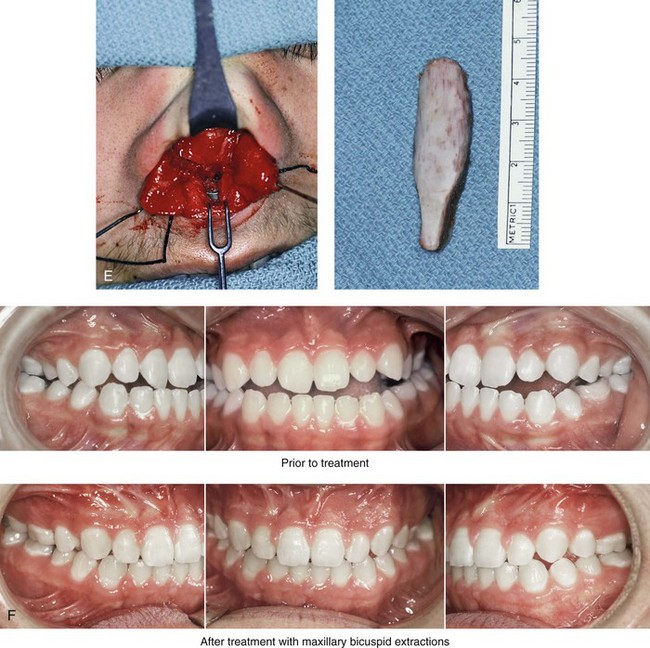
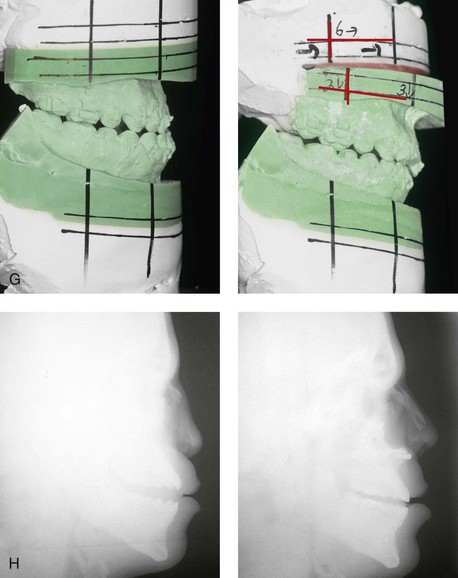
Figure 29-4 A 17-year-old boy who was born with Binder syndrome was referred for surgical evaluation. He agreed to orthodontic treatment that included maxillary first bicuspid extractions and orthognathic and nasal surgery. The patient’s procedures included Le Fort I osteotomy (horizontal advancement) and nasal reconstruction (autogenous rib graft). The nasal reconstruction was carried out through an open (columella />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


