Digital Technology in Implant Dentistry
Lee Culp, Natalie Y. Wong, Carl E. Misch
The Harmony of Function and Esthetics with Digital Technology
The ultimate goal to replace the natural dentition is to restore a patient to normal contour, comfort, function, esthetics, and health. The attainment of perfection in the duplication of natural dentition is the ultimate achievement in contemporary esthetic dentistry. Understanding the complex relationship between tooth form and function and how they relate and combine to create the esthetics of natural dentition is the basis of study for achieving predictable success in oral reconstruction. Throughout the years, restorative trends and techniques have come and gone. Some material developments have transformed the face of esthetic dentistry, but other initial concepts have phased out and died.
As patients become more educated to modern dentistry’s advances, their motivation and desire for natural esthetic restorative dentistry is increasing at a dramatic rate. Dentists are now more predictably fulfilling these patient demands but still often use dental laboratories and restorative techniques that do not offer predictable efficiency and quality. Digital dentistry is a methodology to expand the predictable aspect of restorative dentistry, especially when replacing part or all of the natural dentition.
The concept of digital dentistry is one that started out small and has progressively increased in momentum until its boundaries appear to have become endless. However, new technologies in dentistry will only be successful if they are combined with a complete understanding of basic comprehensive dentistry. Although new technology and computerization can make procedures more efficient, less labor-intensive, and more consistent, it will not replace education, practical experience, and clinical and technical judgment.
The most exciting factor surrounding these technologies is not, however, only in the potential applications of the technologies that are being hypothesized by dental professionals. The excitement truly lies in the fact that these “hypothetical” applications are currently being developed today, and some are even in the final stages. Implants are now well documented for fulfilling the functional requirements in prosthetic tooth replacement. These new technologies along with evolution of surgical and prosthetic techniques allow the dental team predictable, consistent results in implant rehabilitation. In a relatively short time period, digital technology will revolutionize the quality of dental care that is being delivered in modern practice.
The newest technology to enter restorative dentistry is CAD/CAM (computer-aided design/computer-aided manufacturing). Based on technology adopted from aerospace and automotive and even the watch-making industry, this technology is accepted because of its advantage of increased speed, accuracy, and efficiency. Today’s CAD/CAM systems are being used to design and manufacture metal, alumina, and zirconia frameworks, as well as all-ceramic, full-contour crowns, inlays, and veneers that may be stronger, fit better, and are often more esthetic than restorations fabricated using traditional methods. When partnered with predictable implant technology, CAD/CAM offers restorative dentists and technicians an expanding horizon of dental prosthetic options. This success awakens a new focus; esthetics in implant prosthesis is now of major concern in both the surgical and prosthetic phases of treatment.
As dentistry evolves into the digital world, the successful incorporation of computerization and new technology will continue to provide more efficient methods of communication and fabrication while at the same time retaining the individual creativity and artistry of skilled dentists and dental technicians. The utilization of new technology will be enhanced by a close cooperation and working relationship of the dentist–technician team. The evolution from hand waxing to “digital waxing” using the diagnostic wax-up and provisional restorations and their digital replicas to guide us in the creation of CAD/CAM restorations will be presented. The utilization of these new technologies, along with the evolution from “hand” design to “digital’ design, with the addition of the latest developments in intraoral laser scanning, materials, and computer milling and printing technology will only enhance the close cooperation and working relationship of the dentist–dental laboratory team.
The Dental Laboratory
The dental laboratory’s primary role in restorative dentistry is to perfectly copy all of the functional and esthetic parameters that have been defined by the dentist into a restorative solution. Throughout the entire restorative process, from the initial patient consultation, diagnosis, and treatment planning to final restoration placement, the communication routes between the dentist and the laboratory technician now can provide a complete transfer of information. Functional components, occlusal parameters, phonetics, and esthetic requirements are just some of the essential types of information that are necessary for technicians to complete the fabrication of successful, functional, and esthetic restorations. Today, as in the past, the communication tools between the dentist and the technician include photography, written documentation, and impressions of the patient’s existing dentition. The clinical models from these impressions may be created and mounted on an articulator, which simulates the jaw movements of the mandible.
The Digital Laboratory
As restorative dentistry evolves into the digital world of image capture, computer design, and the creation of dental restorations through robotics, the dental laboratory must evolve as well (Figure 27-1). To fully understand this concept, a laboratory must be clearly defined. At first thought, it may seem that a laboratory is the place where a dentist sends his or her patient’s impressions to be processed into restorations, which are sent back to the dentist for adjustment and delivery. This definition fits well with the traditional concept of a laboratory–dentist workflow. However, just as the Internet has forever changed the landscape of communication through related computer technology, the possibility to use CAD/CAM restoration files electronically has provided the catalyst for a significant change in the way we view and structure the dentist–laboratory relationship.

Imagine that the laboratory is not a physical place but exists only in the talents of those performing the restorative process: the dentist and the technician. The equipment used to create the restoration may be located centrally, remotely, or both. The laboratory is essentially a workflow, which is as flexible as the abilities of the dentist, the technician, and the equipment will allow. The primary decision becomes where the hand-off from one partner to another should occur. The dentist who has the ability to optically scan teeth for impression making and chooses CAD/CAM restorations as the treatment option for his or her patients has enhanced freedom as to where the hand-off to the technician should occur. As a result, the laboratory is no longer a place; it is instead, to a large degree, virtual.
The Digital Process
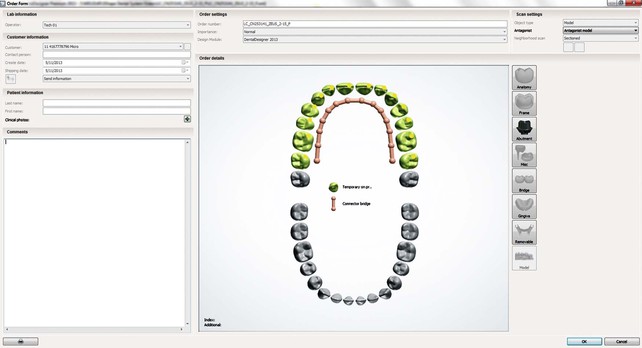
The new millennium has brought with it a change in digital dentistry because more than 20 different CAD/CAM systems have now been introduced as solutions for restorative dentistry. The introduction of digital laboratory laser scanning technology along with its accompanying software allowed the dental laboratory to create a digital dental environment to accurately present a real three-dimensional (3D) virtual model that automatically takes into consideration the occlusal affect of the opposing and adjacent dentition. This process also includes the ability to design 16 individual full contour anatomically correct teeth at the same time (Figure 27-2). It essentially takes a complex occlusal scheme and its parameters and condenses the information, displays it in an intuitive format that allows dental professionals with basic knowledge of dental anatomy and occlusion to make modifications to the design, and then sends it through to the automated milling unit. For the dental laboratory profession, the introduction of digital technology can effectively automate or even eliminate some of the more mechanical and labor-intensive procedures (waxing, investing, burnout, casting, and pressing) involved in the conventional fabrication of a dental restoration, allowing the dentist and technician the ability to create functional dental restorations with a consistent, precise method.
Linear versus Vertical Manufacturing
The successful laboratory of the future will need to focus not just on quality of the final end product but also more efficient production methods to reduce turnaround time within the laboratory process. Digital technology allows the laboratory production to become vertical rather than linear. The current laboratory fabrication process follows a very linear progression; model fabrication on day 1, waxing on day 2, finishing on day 3, ceramics on day 4, and so on. Average production time for an all-ceramic or porcelain-fused-to-metal (PFM) restoration is approximately 5 to 7 working days based on this fabrication method.
In the digital laboratory, impressions will still be received from the client. But instead of taking days or weeks to go through several processes, the same process can be accomplished in 2 to 3 days. After the impression is received into the laboratory, the impression has the possibility to be scanned, and those data will be sent to several digital production stations at the same time. This will potentially allow the model and the restorations, including the framework, the wax-up, and the final ceramic restoration, to be completed at the same time.
Digital Diagnostic and Treatment Planning
The basis for all long-term success in restorative dentistry is a comprehensive diagnosis and treatment plan. The ability to preview a case from start to finish, communicating and co-diagnosing with other specialists and specialties about dental patients via the virtual world is the true power and capability of digital dentistry.
The emergence of cone-beam computed tomography (CBCT) scanning 3D volumetric imaging systems now provides dentists and specialists complete views of all oral and maxillofacial structures, giving the dental profession improved diagnostic information for a variety of treatment areas. Digital dentistry may allow for more accurate diagnosis and treatment planning, which leads to more predictable treatment outcomes. This includes implant placement and restoration, diagnosis and treatment of temporomandibular joint disorder, and the creation of functionally esthetic all-ceramic restorations. With the ability now to combine high-resolution data that are acquired from intraoral laser scanning, with the amazing global information that CBCT offers, we now have the ability to create a true digital patient. This combination of data sets will offer dentistry the ability to predictably offer accurate diagnosis, treatment planning, and restorative outcomes.
The combination of computed tomography (CT) scanning and laboratory-based laser scanning technology (e.g., 3 Shape, Laserdenta, Dentalwings) along with intraoral digital impression capture technology (e.g., E4D, NEVO, 3M Lava COS, Cerec, and iTero), in harmony with the design capabilities of state-of-the-art software would offer for the first time in dentistry the accurate representation of a virtual patient. This concept will have the ability to preview and even test different treatment options to enhance patient care, combining the data to develop a proper treatment plan for patient analysis and treatment. As a result, one can create solutions that would include all functional and esthetic aspects of oral rehabilitation.
Dental design software is currently available that will allow dentists and technicians and even patients the ability to communicate and create numerous anterior tooth arrangements based on functional and esthetic parameters, as well as the patient’s desires. This would encompass both software and output devices to simulate and fabricate intraoral devices for tooth movement, tooth restoration, and tooth replacement.
Digital Fixed Prosthetics
Historically, PFM restorations have been manufactured through the traditional lost wax casting process. The recent proliferation of dental CAD/CAM systems is having little effect on the PFM manufacturing process because machining metal substructures in popular alloys is inefficient and costly. However, now with metal laser sintering technology, dental laboratories can produce bridges and copings directly from CAD data without waxing and investment casting. The technology virtually relieves the dental laboratory of the least valuable tasks in the prosthesis manufacturing chain. The laboratory no longer needs to spend time waxing, investing, and casting but instead can concentrate on core competencies such as the ceramic veneering of the metal framework. The laser sintering process is faster, more economical, and requires only a minimum amount of manual labor while providing the dental laboratory with a scalable technology irrespective of technician availability. At the same time, the cycle times decrease to a minimum, thus resulting in an enormous increase in productivity and a definite technological advance for the dental industry.
The Digital Process
The laboratory technician’s primary role in restorative dentistry is to perfectly copy all functional and esthetic parameters that have been defined by the dentist into a restorative solution. It is an architect–builder relationship. Throughout the entire restorative process, from the initial consultation through treatment planning, provisionalization, and final placement, the communication routes between the dentist and the technician require a complete transfer of existing, desired, and realistic situations and expectations to and from the clinical environment. Functional components, occlusal parameters, phonetics, and esthetic information (shade and contour) are just some of the essential information that is required by the technician to complete the fabrication of successful, functional, and esthetic restorations.
Communication of Occlusion
Historically, the transfer of occlusal and functional information from the clinical environment to the laboratory was somewhat limited. There was little, if any, direct communication of the functional requirements for a case beyond the dentist providing an opposing model and an impression and sometimes an interocclusal record with the shade preferences. With limited guidance, the technician would mount and articulate the case (most often on a hinge articulator) and restore the case by filling spaces and trying to mimic the existing dentition using his or her own interpretation and experience. The result was a close approximation that the technician hoped would meet or exceed the dentist’s and patient’s expectations. In situations like this, the dentist expected to spend considerable chair time seating a case, adjusting the occlusion, and recontouring restorations. The results were often a complete removal of anatomy, occlusal form, and sometimes an esthetic and functional compromise of the final restoration.
There were, of course, dentists and technicians who desired more predictable results and sought a solution through advanced continued education courses that encouraged a dentist and technician team approach and sought out the combination of restorative and functional requirements. This group was introduced to the concept of comprehensive dentistry, which took into account optimum oral health, anatomic and functional harmony, and occlusal stability rather than singling in on just the restoration of aspect and tooth.1 To accomplish this, the dentist–technician partnership became a “diagnostic team” with the dentist and technician both participating in the complete understanding of the cause-and-effect relationship of the problems before initiating treatment.
Computerized Design and Fabrication
With traditional laboratory procedures, after the elastomeric impression of the implant impression coping is obtained, the dental laboratory must pour up a stone or an epoxy working model to fabricate the restoration and implant abutment. The lost wax technique developed in 1907 by Taggart is still currently used in many dental laboratories.2 Inaccuracies during the laboratory phase can include dimensional instability of the stone material, wax, casting investment, and alloy material, which results in an inaccurate fitting restoration and abutment.3,4
CAD/CAM technology originated in the 1950s with numerically controlled machines feeding numbers on paper tape into controllers wired to motors positioning work on machine tools. Advances were made in the 1960s with the creation of early computer software that enabled the design of products in the aircraft and automotive industries. The introduction of CAD/CAM concepts into dental applications was the innovation of Dr. Francois Duret in his thesis titled “Empreinte Optique” (“Optical Impression”) in 1973.5 He developed and obtained a patent for a CAD/CAM device in 1984 and took it to the Chicago Midwinter Meeting in 1989 where dentists witnessed a crown fabricated in 4 hours. In 1980, a Swiss dentist, Dr. Werner Mörmann and an electrical engineer, Marco Brandestini, developed the concept for what was to be introduced in 1987 by Sirona Dental Systems LLC (Charlotte, NC) as the first commercially viable CAD/CAM system for the fabrication of dental restorations—CEREC.6
Dental Impressions
As with any conventional laboratory-prescribed restorative process, this procedure begins the same: the clinician prepares the case according to the appropriate preparation guidelines, impressions the case, and sends all critical communication aspects to the laboratory. When the laboratory receives all the materials, the impressions are poured, the models mounted, and the dies trimmed. A bite registration is taken using the mounted models and will be used in a subsequent step.
The overall excellence and marginal fit of any definitive fixed restoration in dentistry depends on the accuracy of the dental impression. The introduction of CAD/CAM to dentistry through digital impression systems has paved the way to a completely digitized design and manufacturing process, which simplifies the creation of restorations and makes them more reliable.7
Digital dental impressions have potentially eliminated the need for taking conventional impressions for crowns and other fixed prostheses.2 In implant dentistry, the goal in the prosthetic phase of treatment is to fabricate an accurate restoration of high quality and an abutment with an appropriate emergence profile, occlusion, and esthetic appeal. In the standard crown and bridge approach, to fabricate a restoration with an ideal fit, the impression material used must capture the details of the abutment margin, the gingival anatomy, and the adjacent and opposing dentition.3 The accuracy of crown and bridgework is determined by the accuracy of the many steps of the process, including making and extracting the impression, pouring models, cutting and trimming dies, and the properties of the dental stone itself. Each of these steps decreases the accuracy of the clinician’s work, which leads to expensive increases in chair time, costly laboratory remakes, and unhappy patients.
To make a good impression, the material used must meet all the ideal properties and requirements (Table 27-1). Such requirements include sufficient working and setting time, hydrophilicity, wettability, tear strength, and elastic recovery.4 Similar to conventional fixed prosthetics, impression materials used to fabricate a restoration and an abutment for the implant must meet all the requirements to capture a good impression. However, dental impression materials were designed to capture tooth margins and may not be as accurate when used with metal or ceramic abutment materials.8,9 A survey of laboratory technicians indicated that as high as 90% of conventional dental impressions have incomplete registration of finish lines.10 Without an accurate duplication of finish lines, the prosthesis becomes little more than an approximation of the properly fitted prosthesis.
TABLE 27-1
Properties of Impression Materials
| Viscosity | Border | Wash | Co-lamination between Viscosities | Hydrophilicity | High Tear Strength | Engage Undercuts | Working and Setting Time | Patient | Operator | |
| Plaster | Light | No | Yes | No | Yes | No | No | Not constant | Sensitive | Sensitive |
| Impression compound | Heavy | Yes | No | No | No | No | No | Not constant | Sensitive | Sensitive |
| ZOE | Light and medium | No | Yes | No | No | No | No | Not constant | Sensitive | Sensitive |
| Alginate | Light and heavy | No | Yes | No | Yes | No | Yes | Not constant | Sensitive | Sensitive |
| Polysulfide | Light and heavy | Yes | Yes | No | No | Yes | Yes | Somewhat constant | Sensitive | Sensitive |
| Polyether | Multiple | Yes | Weak yes | Yes | Yes | Weak yes | Yes | Constant | Slightly sensitive | Not sensitive |
| Condensation silicone | Light and medium | Yes | Yes | Weak yes | No | Yes | Weak yes | Not constant | Not sensitive | Not sensitive |
| Polyvinyl siloxane | Multiple | Yes | Yes | Yes | Yes | Yes | Yes | Constant | Not sensitive | Not sensitive |
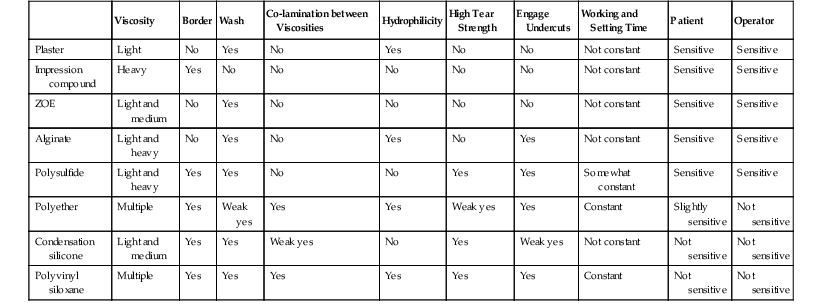
Conventional Impression Materials
The purpose of making a dental impression is simply to transfer 3D data from the patient’s mouth to a model as accurately and as comfortably as possible. The goal of the material used to make a dental impression must be to replicate hard and soft tissue structures under both wet intraoral and dry laboratory conditions with minimal hygroscopic distortion. A wide variety of impression materials have been developed to help us in achieving this. Rubber base (slow setting and foul smelling) was the most common and best available material into the mid 1970s. In the late 1970s, hydrophobic polyvinyl impression materials were introduced, and they gained popularity. They are the most commonly used impression materials in North America. In the mid 1990s, truly hydrophilic polyvinyl materials that could take accurate impressions of wet intraoral surfaces were introduced. Other enhancements included material strength, tear resistance, repeated pourability, and easy-to-read coloration. Polyvinyl siloxane (PVS) impression materials quickly became the material of choice in conventional impressions because they were accurate; fast; predictable; and last but not least, easy to use.11 Table 27-1 is a comparison of the advantages and disadvantages of properties of all impression materials. PVS is the most commonly used material for conventional dental impressions, and its properties will be compared with digital impressions.
Dimensional Accuracy
The dimensional accuracy of PVS is excellent if the margins of the preparation are isolated, the impression material covers the preparation adequately and uniformly, and the material is completely set before removal. Otherwise, the accuracy decreases because there is a risk of distortion of the impression material. In comparison, a digital impression technique will have equal or better dimensional accuracy because there is no impression material and thus no risk of any material distortion. Although moisture control and tissue management are required for both, digital impressions require this control for only one image at a time.
Capturing Detail
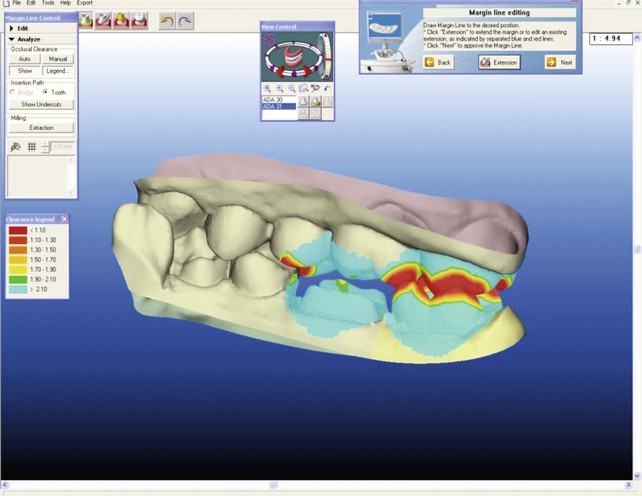
Capture of detail in a conventional impression is good when there is no movement of the impression tray and no air entrapment and the impression material is allowed to set completely. In the case of the digital impression technique, the images capture detail and are magnified, which allows any problems with the preparations to be visualized immediately. In addition, occlusal clearances are also verifiable (Figure 27-3).
Time
Dental impression materials on the market today require on average 5 to 8 minutes of mixing and setting time. The digital impression technique will have an initial learning curve of approximately five to 10 scans, after which an average quadrant scan is 3 to 5 minutes. This may seem to be just a small savings in time; however, the task in which the digital impression technique shows its superiority is in a remake situation. Remaking of a conventional impression doubles the time as it will require another 5 to 8 minutes for the second impression. In addition, the entire impression needs to be remade. A survey by the Consilium Associates in Irvine, California, states that 36% of dentists have to remake their impressions at least three times or more per month. With the digital impression technique, the only area that needs to be rescanned is the area that was missed.
Intraoral Access
Intraoral access using conventional impression techniques can be a challenge for those with an active gag reflex, excess saliva, small oral cavities, or large cheeks and tongue. With the conventional technique, the entire impression (the tray and the material) needs to be in the mouth and stable until the impression material has set completely. With the digital impression technique, a significant advantage is that the image capture process can be paused and continued multiple times to ensure the patient is comfortable during the procedure. A/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses