27
Choice of Intracoronal Restorations
Intracoronal restorations are defined as those surrounded by one or more natural tooth surface(s) and can broadly be categorised according to Black’s cavity classification; classes I, II, III, IV and V, and the newly added class VI.
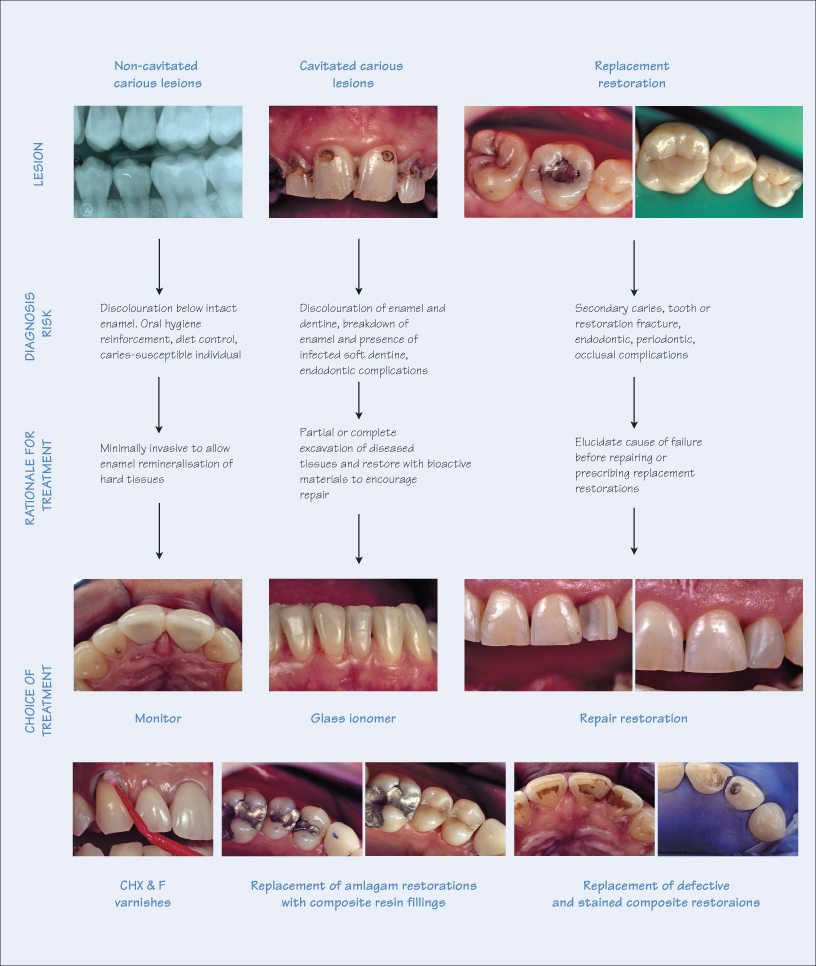
Treatment for intracoronal lesions depends on a variety of factors, and for optimal clinical decision–making, it is necessary to accurately diagnose pathology, determine aetiology, identify risk factors and assess prognosis for various treatment options.
Non-Cavitated Carious Lesions
Current research has highlight the ability for enamel to remineralise following carious attack. Therefore, a non-cavitated carious lesion extending into dentine, with appropriate treatment, has the potential to be arrested by remineralisation of the demineralised enamel hard tissues. The factors to consider for non-cavitated lesions are:
- Aetiology – cariogenic bacteria;
- Clinical presentation – discolouration below surface of an unrestored tooth; caution is necessary when using sharp probes, in order to avoid piecing the delicate demineralised surface enamel;
- Symptoms – none or sporadic sensitivity;
- Risk assessment – patients with poor oral hygiene, inadequate diet control, or individuals with high caries susceptibility require restorative intervention;
- Treatment options – minimally invasive, monitor for low-risk patients, or restore for high-risk patients;
- Type of restoration – chlorhexidine (CHX) and fluoride (F) varnishes, fissure sealing, direct restorations;
- Choice of restorative materials – bioactive restorative materials (glass ionomers, resin-based composites), or amalgam;
- Prognosis/outcome:
a) Halted carious lesion with or without remineralisation of enamel – monitor with periodic application of varnishes and/or fissure sealants;b) Reparative ‘healing’ with bioactive restorative materials – monitor;
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


