Biomechanical Strategies for Optimal Finishing
Flavio Andres Uribe, Padma Mukherjee, Ravindra Nanda
Orthodontic finishing is described as an “art” composed of individual perceptions and small detailing. Finishing distinguishes a true master of the profession from an average orthodontist. It is a critical step that involves fine-tuning individual tooth positions and intra-arch and inter-arch relationships and optimizes the treatment results.1 This step can be especially challenging to the clinician since the minor changes performed generally are not appreciated by patients.
Finishing is the last phase of “active” treatment and thus is heavily dependent on the previous stages of treatment. It is extremely difficult, if not impossible, to achieve an acceptable end result when the treatment objectives have not been met and the mechanics have not been delivered properly. Major tooth movement should have been executed properly so that the minute tooth movements can be achieved with precision in the final finishing phase of treatment. When the treatment mechanics are less than optimal, the finishing stage often includes indiscriminate use of intermaxillary elastics and quick-fix therapies such as interproximal reduction. Although there are definite indications for these procedures, they should not be used routinely to compensate for deficiencies in treatment planning and/or application of mechanics. Overall, the finishing stage of treatment should be evaluated according to four major categories: intraoral, extraoral, radiographic, and functional objectives. In each category specific objectives must be met to obtain a desirable finish (Fig. 27-1).
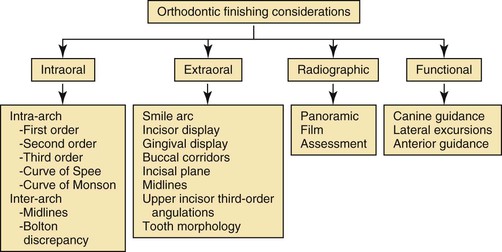
Figure 27-1 Systematic approach to finishing.
Intraoral Objectives
Intraoral objectives are arguably the most important of the four major categories.2 The intraoral objectives are classified into two subcategories: intra-arch and inter-arch objectives. The primary objective in both is to achieve ideal occlusion with well-aligned arches. Most of these intraoral objectives are described in the American Board of Orthodontics (ABO) grading criteria.2
Intra-Arch Analysis
Each tooth must be evaluated with reference to its first-, second-, and third-order position. When evaluating the first order, teeth should have no rotations and have tight interproximal contacts.1 In addition, tooth morphology must be taken into consideration and the cusp tips and fossae should follow the perfect arch form. An occlusal mirror can be very useful to identify minor rotations and buccolingual displacement of teeth outside of the perfect arch form (Fig. 27-2). The upper first molar has special considerations regarding its first-order position. A mesial-out rotation of the mesiobuccal cusp3 is considered to be ideal. It has also been advocated that the buccal surface of the upper first molar should be parallel to the palatal suture (Fig. 27-3).4
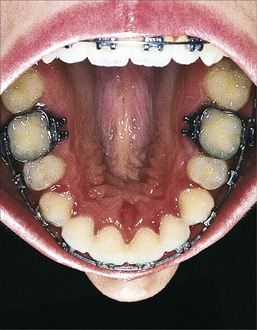
Figure 27-2 Occlusal mirror used as an aid to evaluate intra-arch discrepancies during finishing. This view is used to identify first-order rotations, spacing, and any arch form problems.
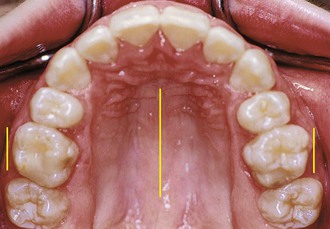
Figure 27-3 Occlusal view of a finished case where the buccal surface of the upper first molar is parallel to the midpalatal raphe.
In the second order, the root parallelism and marginal ridges are evaluated. The marginal ridges should be at the same level, particularly in the buccal segments. Often when marginal ridges between adjacent teeth coincide, root parallelism also will. A panoramic x-ray is an adjunct to evaluate second-order discrepancies. In extraction cases, a small degree of crown tipping most likely will occur and root parallelism will be required. Small adjustments in the second-order angulation of the anterior teeth (i.e., accentuating the distal tip) can help to decrease any excess space in the anterior region (Fig. 27-4).1 The third order is most relevant to the inter-arch objectives (i.e., the occlusal relationship) and to the esthetics of the smile (an extraoral category, discussed below). Regarding the intraoral objectives, a small curve of Monson between the buccal segments allows for proper occlusal function (i.e., adequate intercuspation without balancing interferences). An accentuated curve of Monson usually results in balancing interferences, especially in the second molar area.5 This clinical situation is commonly encountered in adults after the dental correction of buccal crossbites without expansion of the basal bone and palatal suture (Fig. 27-5). Proper third-order angulation of anterior teeth is also important for good occlusion (Fig. 27-6). Furthermore, regarding the extraoral category, third-order angulation is important for good esthetics of the smile (Fig. 27-7).1 Significant emphasis on the upper canine and first premolar third-order inclination has been proposed by some clinicians.6 In general, the buccal surfaces of these teeth should be close to parallel to the midsagittal facial line in an ideal smile.
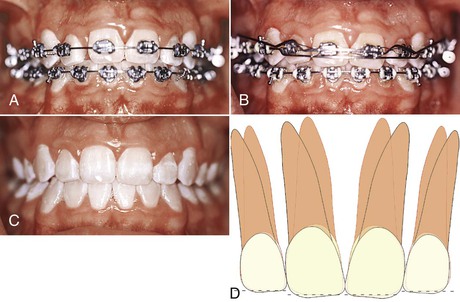
Figure 27-4 A–C, Patient shows no overjet but excess space between the incisors due to a Bolton discrepancy. These spaces can be closed or reduced by accentuating the distal root tip of the incisors, thereby increasing the interproximal contact distance. Incisal adjustments (enamoplasty) were done at the appliance removal visit. D, Diagram showing the distal tip and enamoplasty required.
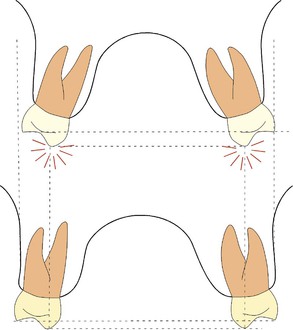
Figure 27-5 Proper third-order angulation needed in the posterior buccal segments may not be achieved in adults after arch width expansion without surgery. Occlusal balancing contacts may result from the dental third-order compensation. The lower diagram shows the difference in skeletal width and vertical cusp position that can be achieved with skeletal expansion.
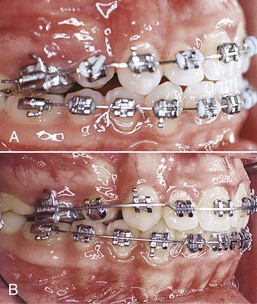
Figure 27-6 A and B, Patient showed an improvement in the occlusion after proper third-order angulation of the anterior teeth was obtained.
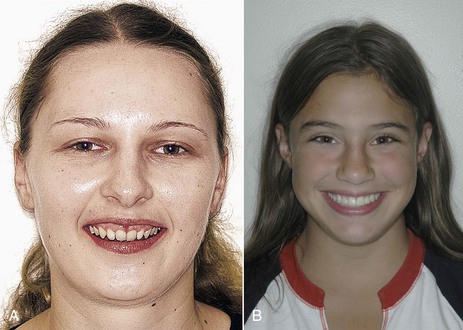
Figure 27-7 Depending on the upper anterior third-order angulation, light is reflected differently in the frontal view. A, Patient with retroclined incisors. Note the light reflected in the periodontal tissues. B, Patient with proper incisor inclination. Note the light reflected in the middle third of the incisors.
The final intra-arch objective is to achieve a gentle curve of Spee from the anterior teeth to the posterior buccal segments.1 The magnitude of this curve will vary depending on the overbite (inter-arch relation) and incisor display (an extraoral objective, discussed below).
Inter-Arch Analysis
The first molars and canines are the most important teeth to evaluate regarding the interocclusal relationship. Traditionally, orthodontists have classified malocclusion in the anteroposterior dimension and thus the static analysis of the occlusion has primarily been based on the first molar relationship. Additionally, the canine is of primary importance if canine-guided functional occlusion is to be achieved. The main objective is to “seat” the canines in a Class I relationship and obtain good coupling with the antagonistic canines. This ideal interocclusal relationship is difficult to achieve when a significant tooth size discrepancy exists between the dental arches (i.e., a Bolton discrepancy).7 The upper lateral incisors and lower second premolars are usually responsible for this inter-arch tooth size discrepancy,8 as abnormal tooth morphology is more common in these teeth. This results in less than ideal occlusion, such as a Class II canine tendency on that side, that becomes apparent during finishing (Fig. 27-8).

Figure 27-8 Bolton discrepancy reflected in the occlusion in the finishing stage. There is a tendency toward a Class II canine relationship due to the small upper laterals.
Two types of occlusion have been considered ideal: cusp-to-fossa and cusp-to–interproximal space relationships. In the natural dentition, a cusp-to–interproximal space relationship is most characteristic.3 The lingual cusps in the upper arch and the buccal cusps in the lower arch are primarily responsible for function. The buccal cusps of the upper premolars and the lingual cusps of the lower premolars should occlude in the interproximal space. In Class II patients, some of the anteroposterior correction can be achieved by overrotation of the buccal cusps of the upper premolars distally to coincide with the lower interproximal spaces.9,10 In the anterior segment, overbite and overjet are the most critical factors in achieving a proper interocclusal relationship. These two occlusal traits determine the disclusion of the posterior teeth during protrusive movements. More than 50% overbite may be excessive, as the contact of the lower incisors on the lingual surface of the upper incisors in these patients would not be on the cingulum (the most suitable portion to receive occlusal forces). Finally, it is important that the lingual surface of the upper incisors be properly inclined to allow the lower incisors to slide anteriorly in an angle that is in synchrony with the articular eminence.11
Arch coordination is also evaluated from the frontal view. This allows proper cusp seating to be visualized. The intercanine and inter-molar widths should be coordinated to prevent excessive buccal overjet or a buccal crossbite tendency. The premolar area is also inspected transversely for proper coordination between the upper and lower arches.
Midlines are also used to evaluate interocclusal relationships. During finishing, minor midline problems should be addressed. Any discrepancy >2-mm should have been addressed during the previous phases of treatment. A discrepancy of 1- to 2-mm or more between the midlines is usually due to a tooth size discrepancy and will probably result in an inadequate occlusal relationship, at least in one of the buccal segments (Class II or Class III on one side) (Fig. 27-9). The midline objectives in the finishing stage are evaluated in the extraoral finishing category as well, particularly in the upper arch.
Extraoral Objectives
The extraoral objectives are based on esthetic concepts, with the majority of these concerning the smile. The key factors within the smile that must be addressed are smile arc, incisor display, gingival display, buccal corridors, incisal plane, midlines, upper incisor third-order inclination, and tooth morphology in the esthetic zone.
Smile Arc
The ideal smile arc is discussed in Chapter 1. In the finishing stage, little can be done to significantly affect the smile arc. Small finishing bends can differentially extrude or intrude the anterior teeth but that is about all that can be accomplished. The dilemma concerning these wire bends is the potential for antagonistic effects on the interocclusal finishing objectives. An example of this is seen when the overbite is perfect and the teeth need to be extruded to achieve an ideal smile arc. A choice between achieving an esthetic objective (ideal smile arc) and an occlusal objective (ideal overbite) is needed. A compromise might be the best decision. In such situations the initial objectives of the individual treatment plan must be reviewed. More importantly, a limit to the amount of compromise for each characteristic should be set (i.e., avoiding finishing with >50% overbite and a flat or reverse smile arc).
Incisor Display
On average, females show 2- to 3-mm of incisor at rest and 1-mm of gingiva when smiling.12 Males show approximately 1-mm less incisor in each of these lip positions. During the diagnosis and treatment planning phases, an appropriate plan for correction of any deviation should be made. By the finishing phase of treatment the vertical incisor objectives should have already been accomplished. Detailing in this area should be limited to proper alignment and leveling of the incisal edges (provided no restorations are needed). Attempting to significantly intrude or extrude the incisors may complicate and prolong treatment.
Open-bite malocclusions with moderate to excessive incisor display present a challenge, as they are difficult to correct. It is not unusual to find an open-bite tendency still present at the finishing phase in this type of malocclusion. If no additional upper incisor display is desired, the overbite correction should be done by extruding the lower anterior teeth. This can be accomplished by accentuating the lower curve of Spee.
Gingival Display
The amount and characteristics of the gingival display (symmetry and height relationships of adjacent teeth) are important aspects to consider in a smile. Generally, males do not show any marginal gingiva when smiling. Females, on the other hand, display approximately 1-mm of gingiva on smiling.13 Symmetry in the gingiva and proper gingival height relationships in the upper arch are important considerations during initial bracket positioning and final finishing repositions (Fig. 27-10).

Figure 27-10 Finished treatment in a young female patient who displays the upper gingiva on smiling. An asymmetry in the gingival heights of the lateral incisors is evident.
During finishing, gingival display and symmetry can be altered within a narrow range of approximately 1-mm by selective intrusion or extrusion of any of the anterior teeth. Most frequently, the incisal edges will reflect gingival height asymmetries provided that incisal wear is not present (Fig. 27-11). The overbite will be the limiting factor of the magnitude of the finishing bends. However, if wear is present, the gingival height relationship will determine the finishing movements of the anterior teeth in the vertical dimension, instead of it being determined by the level of the incisal edges (Fig. 27-12).14 The final incisal edge position, if there is significant incisal wear, is determined by proper tooth proportions, gingival heights, relationship to the upper lip, crown/root ratio, and overbite (Fig. 27-13).
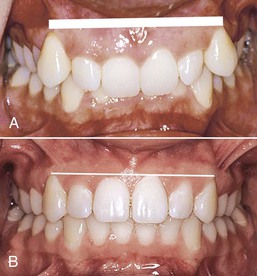
Figure 27-11 A, Incisal edges reflect the discrepancies in the gingival heights provided that no incisal wear is present. B, Correction of the incisal edges generally results in adequate gingival heights.
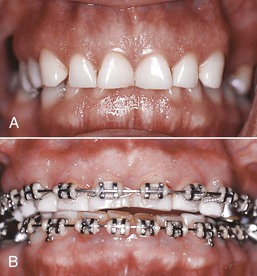
Figure 27-12 A, Inadequate gingival height in the upper anterior region with excessive overbite and worn incisors. B, Intrusion mechanics of the four upper anterior teeth to obtain proper gingival heights. Restoration of the incisors is needed to achieve adequate proportions and overbite.
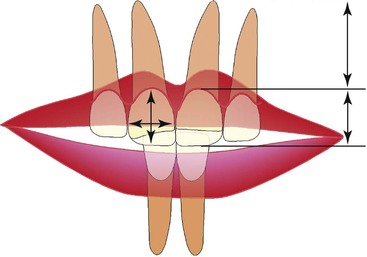
Figure 27-13 Factors involved in the final incisal edge position. The interrelationship of gingival height, tooth proportions, lip to tooth relationship, crown/root ratio, and overbite determines the position of the upper incisor in space.
Periodontal procedures should be considered as an adjunct to the esthetic objectives after finishing in patients with an excessive gingival display or asymmetrical gingival heights. The periodontal procedures that can be considered are gingivectomy or crown lengthening (depending on the alveolar bone level) (Fig. 27-14). These procedures may also be combined with prosthetic alternatives in patients with worn incisal edges or abnormally shaped incisors (i.e., peg laterals).

Figure 27-14 Asymmetrical gingival heights. A, Upper right lateral incisor has a more coronal gingival height. The upper right central incisor also has a slight coronal relationship of the gingival margin compared with its contralateral tooth. B, Gingivectomy performed on the upper right central and lateral incisors. C, Postsurgery.
A common unesthetic result after gingivectomies or crown lengthening (performed exclusively in the anterior segment) is seen in the transition area from the canine to the premolars. Ideally, there should be a 1-mm step down in gingival height between these teeth. When gingivectomies are not carried to the premolars, excess gingiva remains more pronounced in the corners of the smile (Fig. 27-15).15

Figure 27-15 Excess gingival show on the upper buccal segments. Gingival heights are adequate from canine to canine. A smoother transition from the canine to the first premolar can be obtained through periodontal surgical procedures.
In the literature little attention has been given to the gingival heights of the lower teeth. Symmetry and gingival height of the lower incisors in relation to the canines are important factors, especially in individuals over 30 years of age, as the lower gingival margin is more visible.12 It is not uncommon to find a discrepancy in gingival heights between the lower incisors and the canines, particularly in deep bite patients (Fig. 27-16). In young patients, the gingival margin usually follows the incisal edges of the lower anterior teeth. This problem is corrected as the canines and central incisors are leveled during the initial phases of orthodontic treatment. In the adult, wear facets can complicate the determination of where proper gingival heights should be located. As the incisors supraerupt, a good incisal edge relationship with the canines will exist but a significant discrepancy in the gingival height will develop. To correct this discrepancy a decision must be made from the following choices: gingivectomy/crown lengthening to match gingival heights with no restorations, gingivectomy/crown lengthening and restorations (composites or veneers or crowns), intrusion of the four anterior teeth to level the gingival heights (no surgery), and restorations (composites, veneers, or crowns). A very important additional factor in deciding among these alternatives is the crown/root ratio. Any osseous resective periodontal procedure (crown lengthening) increases this ratio; therefore a good assessment of the eventual remaining root structure is required (Fig. 27-17).

Figure 27-16 Discrepancy between the gingival heights of the lower incisors and the canines. Supraeruption of the lower incisors is evident at the incisal edges and is reflected on the overbite.
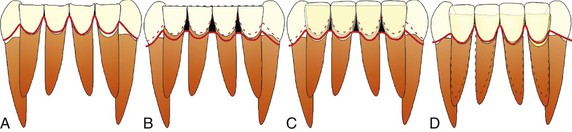
Figure 27-17 A, Significant attrition with supraeruption of the lower incisors. Different treatment modalities include the following. B, Gingivectomy/crown lengthening to match the gingival heights. As the gingival margin is brought down, a more tapered crown morphology is observed. Black triangles may result with this alternative. C, Gingivectomy/crown lengthening with additional restorat/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



