Principles of Fixed Implant Prosthodontics
Cement-Retained Restorations
Carl E. Misch
Protection of the Prosthesis
A predictable surgical protocol for endosteal rigid fixation was developed and reported by Brånemark and Adell et al. more than 30 years ago.1,2 However, on occasion, an implant may fail during the initial healing process from traumatic surgery, compromised healing, poor case selection, or unknown reasons. Patients understand that medicine is not an exact science and that their bodies may respond with individual variation to a standardized procedure. As a result, patients are more inclined to accept the implant surgical failure. To the contrary, once the implant is uncovered and the patient is told that it is successful, any short-term complications that lead to its loss or compromise of the implant often become unacceptable to the patient.
The patient rarely can evaluate the causes of implant surgical failure but, on the contrary, can assess several aspects of the prosthetic result, such as esthetics, occlusion, function, speech, and maintenance. The additional time, appointments, laboratory steps, and associated cost of inventive prosthetics required on poorly placed implants are not fully appreciated. Patients may believe that bone loss or implant loss resulted because the screws were too tight or too loose, the casting did not fit adequately, or the occlusion was incorrect rather than understand the original cause of poor bone quality or poorly angled implant bodies from the surgical phase. All of these factors complicate patient management for restoring dentists.3
The time required to remove a failed implant after initial healing and place an additional implant is often minimal and often may be accomplished at the second-stage surgical appointment. The time required to fabricate the prosthesis is usually five or more prosthetic appointments. An implant failure after final prosthesis delivery also may result in five additional prosthetic appointments and additional laboratory fees. In addition, an implant failure after loading may cause significant bone and soft tissue loss. As a result, replacing the implant may require bone and soft tissue grafting and additional time required before reimplantation. The patient may blame the restoring dentist for the associated bone loss after implant failure.
The restoring dentist usually educates the patient about the limitations of the restoration of a malpositioned tooth. Orthodontic treatment or extraction often is suggested with natural teeth rather than a compromised final prosthetic result. Yet, still too often, dentists consider implants successful with the sole criterion of rigidity. They often overlook an underengineered implant foundation with too few implants, improper implant placement in mesiodistal and buccolingual directions, an excessive sulcus depth, insufficient load-bearing surface area of the implant body, poor angulation, poor bone quality, unacceptable soft tissue contour and quantity, and the relationship of these to esthetic requirements and their influence on complications. Long-term acceptable criteria should be established and the limiting factors identified before the prosthetic reconstruction to minimize the occurrence of complications related to the restoration, maintenance, or patient management.
The retention system of the prosthesis should be designed before surgery. In a screw-retained fixed prosthesis, anterior implants are to be placed more lingual than for a cement-retained restoration because the access hole to the prosthetic screw is placed in the cingulum. The correction of facially placed implants for screw-retained restorations may be more difficult and may lead to unmanageable esthetic compromises.
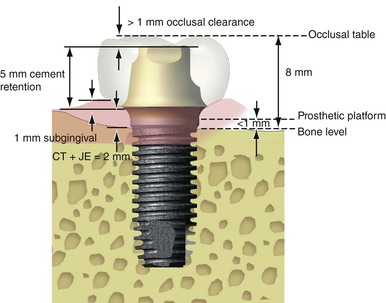
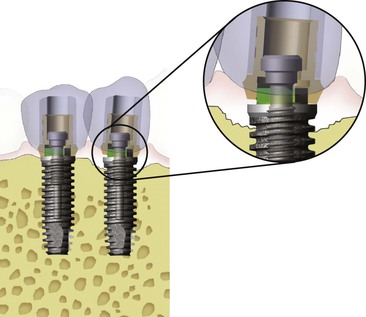
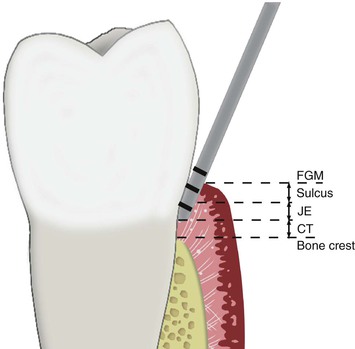
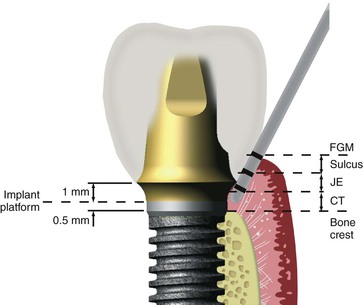
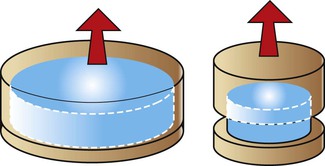
A cement-retained restoration should ideally have 8 mm or more of crown height space (CHS). This dimension permits at least 1 mm for occlusal material on the crown, 5 mm of abutment height for retention and resistance form (with a subgingival margin), a 1-mm subgingival margin, and 2 mm for a junctional epithelial attachment above the bone (Figure 26-1). If inadequate space is present, an osteoplasty of the bone is indicated before implant insertion. In other words, the restoring dentist should identify the type and contour of the restoration, including the type of retention system (i.e., cement or screw retained), early in the treatment plan and convey this information to the implant surgeon before implant placement. The surgical phase should aim at providing the best possible foundation to protect the long-term performance of the prosthesis.3
Cement-Retained versus Screw-Retained Implant Fixed Prostheses
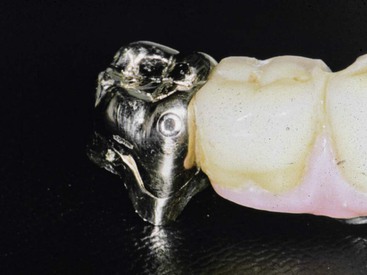
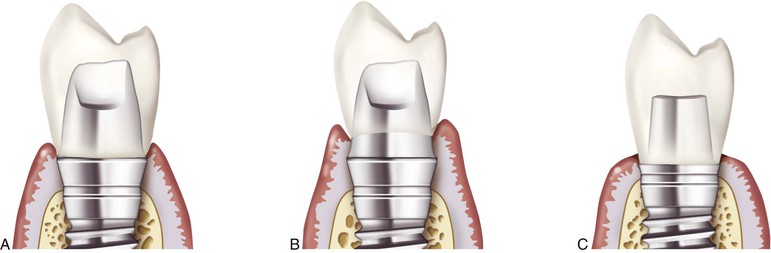
The discussion of screw versus cement retention of the prosthesis applies to the crown or superstructure, not the abutment (Figure 26-2). The abutment is screw retained into the implant body because of reduced surface area of the small diameter and length of abutment posts and to eliminate the risk of cement at the bone-level margin of the abutment and implant. Abutment screw loosening is a prosthetic complication and is addressed in Chapter 28.

Retrievable Restoration
Implant prostheses have more complications (i.e., abutment screw loosening, porcelain fracture, crestal bone loss, and implant failure) during the first year of loading. As such, if the prostheses were able to be removed, it would be advantageous. Some implant manufacturers and dentists recommend screw-retained fixed prostheses on implants as a general rule, suggesting that only a screw-retained restoration is retrievable (Figure 26-3). In addition, if screw loosening occurs and the crown no longer is connected to the implant body, the implant is protected from overload. However, these two reasons to screw retain a restoration overlook several factors.
Although widely variable figures have been published, one can estimate that fixed partial dentures (FPDs) on natural teeth have a mean life span of 10 to 15 years.4–8 In contrast, implant-supported fixed prostheses routinely have demonstrated an implant survival rate greater than 90%.9–16 The complication most often observed with fixed prostheses supported by natural teeth for which a new prosthesis is required is decay.4,7 The second most often occurring complication is related to endodontics. Implant abutments do not decay or need endodontic therapy. As a result, this is a primary reason fixed restorations on natural teeth often have a shorter long-term life span than implant restorations. Hence, implant prostheses have more short-term complications, and natural teeth have more long-term complications.
If a restoring dentist desires to fabricate a screw-retained prosthesis to permit removal and facilitate the management of potential complications, a consistent thinking process would be to use this type of restoration for prostheses on natural teeth because of their higher incidence of late complications. A screw-retained prosthesis may be fabricated for natural teeth in fewer appointments and with less cost than for implants. A coping may be cemented to the tooth with a receptor site for a screw, and the screw may retain the prosthesis (using the same impression and stone model technique) (Figure 26-4). Yet almost all restoring dentists choose to cement tooth-supported restorations. Many of these same dentists still feel obligated to retain implant-supported restorations with screws for retrievability yet continue to use permanent cement on natural abutments. This is an inconsistent philosophy to retain fixed restorations.
The need for implant prosthesis removal often is justified by the need to address problems that have evolved from the screw-retained procedure (e.g., prosthetic screw loosening and increased risk of porcelain fracture). Clinical experience, case series studies, and implant registries indicate higher complication rates with screw-retained fixed prostheses.12,14,17 As the profession has evolved and understands the benefit of cement-retained restorations, the trend toward the use of cement-retained prostheses has grown.15–20
Advantages of Cement-Retained Prostheses
Considerable advantages can be gained with cement-retained restorations, including retrievability, ease of splinting implants, reduced incidence of unretained prostheses, more passive castings, improved correction of nonpassive castings, progressive loading, improved direction of loads, improved hygiene of the implant sulcus, enhanced esthetics, improved access, reduced fracture of components, reduced crestal bone loss, reduced porcelain fracture, reduced cost, and less chair time18–20 (Box 26-1). As a result, the vast majority of the fixed prostheses are cement retained in the United States. This chapter presents the principles for cement-retained fixed implant prostheses.
Retrieval of the Cement-Retained Fixed Prosthesis
The statement that screw-retained restorations are retrievable implies that cemented prostheses are not. For almost every fixed prosthesis on natural teeth, a transitional prosthesis is cemented and then retrieved to cement the final restoration (Figure 26-5). Hence, cemented fixed prostheses can be retrievable when a “soft-access” cement is used as a luting agent.

In a screw-retained prosthesis, the access hole is covered with composite. To retrieve the screw-retained restoration, the dentist must remove the occlusal obturation, the underlying cotton pellet, and the coping screw. After the prosthesis is reinserted, the screws may need to be changed and are torqued, and the occlusal access holes are restored by the dentist. This represents a considerable time investment. To remove and recement a cemented prosthesis is easier and faster.
Protection of the Implant
A loose prosthetic screw can protect the implant under the loose crown because the mobile crown reduces the stress to the implant body. But for implant prostheses with more than one implant splinted together, one must remember that every time a screw loosens, the remaining abutments bear an additional force. The forces include increased moment force offset loads and additional forces on the remaining abutments. The increased loads to the remaining implants may lead to implant loss, component fracture, and bone loss.21,22 It is easier to splint cemented crowns together than to connect screw-retained restorations.
Unretained Restorations
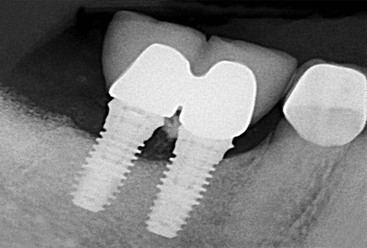
Reports indicate that as many as 6% to 20% of maxillary prosthetic screws loosen at least once during the first year of function.23 The prosthetic screws are less than 1.5 mm wide and engage only three or four threads of the abutment (Figure 26-6). The condition is found more often in single-tooth restorations than when abutments are splinted.13,14,22 However, in clinical studies, reports of unretained cemented implant prostheses constitute fewer than 5% of cases.24,25 Recurring uncemented prostheses are a more unusual occurrence compared with loose prosthetic screws. Hence, when implant abutments are splinted together, it is safer to cement rather than screw retain the restoration.
Passive Casting
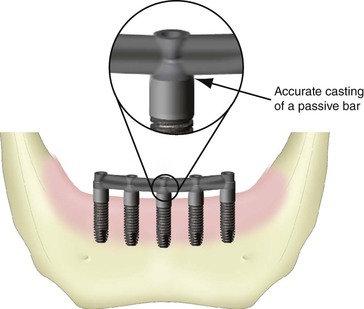
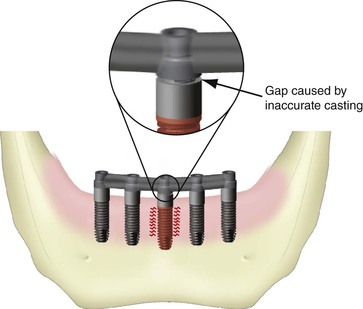
Ideally, when a prosthesis is retained by prosthetic (coping) screws, the restoration passively sits on top of the abutments, and the prosthetic screws fixate the two components together. The screws place a compressive or tensile force on the abutments, but no force is transmitted to the implant bodies (Figure 26-7). If, however, the casting of the prosthesis does not sit passively on the abutments for screws, the force of the prosthetic screws are then transmitted to the implant bodies (Figure 26-8).
A screw is a combination of inclined planes and wedges and is one of the most efficient machine designs. A torque force of 20 N-cm applied on a screw can move two railroad cars. This same force applied to a nonpassive casting tends to distort the superstructure, underlying bone, and implant components (Figure. 26-9). Because the force is constant, it can introduce biomechanical creep into the system, which can fatigue materials and bone. An implant does not predictably move within bone, yet retained stresses from nonpassive castings must be accommodated through a bone remodeling process.
When the screw-retained prosthesis is attached to the abutment for screw retention of the implant, no space exists between the crown and abutment. Instead, a metal-to-metal system with zero tolerance for error is created. Nonpassive screw-retained restorations may create permanent strain conditions on the implant system that can be many times greater than that of cemented prostheses. The microstrain applied to the bone may fall beyond the overload zone and into the pathologic zone in which bone remodeling occurs with crestal bone loss or even implant failure.
Nonpassive castings are a primary cause of unretained restorations, crestal bone loss, implant component fracture, and implant mobility.26,27 A truly passive screw-retained dental restoration is virtually impossible to fabricate on multiple splinted implants.27 Too many variables are out of the dentist’s control when attempting to fabricate a prosthesis with zero tolerance for error, and laboratory procedures may lack the precision needed for such an exact result.
All impression materials shrink while setting.28 For example, polysulfide materials shrink 0.22%, and addition silicone (polyvinyl-siloxane) shrinks 0.06% at 24 hours.29,30 Shrinkage may be clinically relevant because implant analogs used in the impression for a screw-retained restoration do not compensate for the dimensional change of the impression material (Figure 26-10).
Dental stone expands 0.01% to 0.1% and does not correlate to the dimensional changes of impression materials.31–33 In addition, the wax patterns distort while setting or spruing, and the investment material expands32 (Figure 26-11). The metal castings shrink when cooled, and the shrinkage does not permit an accurate metal-to-metal connection.34–37 The metal superstructures are often thicker and larger in implant prostheses than in traditional prostheses because the implant abutment is of reduced diameter, and bone loss volume often is replaced by the final prosthesis. Dimensional changes during metalwork fabrication are correlated directly with the size of the casting.38
The marginal fit and tolerance between the implant analog and implant abutment are often different from actual implant and abutment components.39 Implant components are not all fabricated to exact dimensions, and each transfer of an implant component has a slightly different size, which leads to misfit and is magnified by the number of different pieces used during the fabrication steps.
Full-arch restorations more often are not passive despite an acceptable metal try-in because the volume of porcelain or acrylic shrinkage may have caused material distortion. Porcelain and acrylic shrinkage also is related directly to material volume and may distort the superstructure even though the superstructure was initially passive.32
As a result of all these variables, implant prosthesis distortions ranging from 291 to 357 microns may be observed during the fabrication of the restoration.37 Passive final restorations are highly unlikely when more than two implants are splinted together and support a prosthesis with screw retention as the method of fixation. If a casting has a 50-micron misfit, the casting and implant may have to move 200 microns before the system is completely passive (Figure 26-12). This is a considerable risk to create crestal bone loss, loose prosthetic screws, and implant failure.
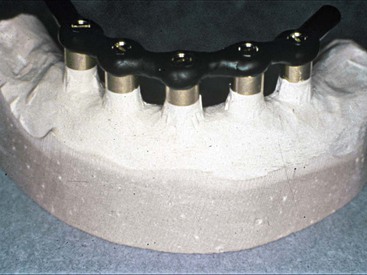
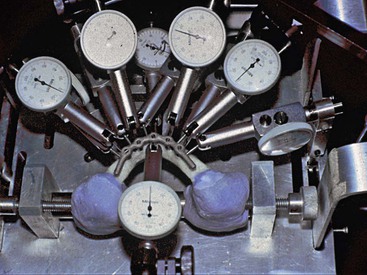
In a study by Strong and Misch, a screw-retained bar was fabricated on five Nobelpharma implants placed in a simulated anterior mandible made of polymethylmethacrylate with a hardness factor of D1 bone density. Three different impression materials and two different dental stones were used (with both direct and indirect impression procedures). The castings were cast with precious metal. After 100 castings were fabricated, the most passive bar (retained with 10 N-cm) moved every implant from 3 to 8 microns (Figure 26-13). This provides a visual report that screw-retained restorations immediately load implants enough to distort the bone–implant interface, which makes the casting appear as clinically passive.
The “clamping down” while tightening the prosthetic screws of an inaccurate structure may lead to screw loosening and fracture.40 After prosthesis delivery, an abutment for screw retention or prosthesis screw may loosen between appointments.41 This usually indicates that the casting is not seated passively, yet the cause often is overlooked. Instead, the screws are tightened again (often with more torque), and the bone must remodel to release the strain in the implant system. This strain may lead to crestal bone loss and even implant failure.
Passive castings represent a considerable advantage for cemented prostheses. Stone dies are often used for cemented prostheses, and the expansion of the stone makes the casing more passive. In addition, die spacers on the stone dies help create approximately a 40-micron cement space that compensates for some of the dimensional variation of laboratory materials and permits the fabrication of a more passive casting with cement-retained restorations (Figure 26-14). This cement space even may extend to the margin of the restoration because cement fills the space and decay is not a consequence with implants.
Correction of Nonpassive Prostheses
If a cemented prosthesis is not passive, the casting or abutment may be modified slightly at the same try-in appointment. High-speed carbides with copious amounts of water may be used to modify the abutment, adjust the internal aspect of the casting, or both and may provide an immediate solution.
A screw-in prosthesis that is not clinically passive requires casting separation and soldering of the casting or a new impression (Figure 26-15). The separation of the metal superstructure must respect specific dimensions to ensure the precision of the soldering (0.008 inch). Too much space causes solder shrinkage and a weak joint; too little space may cause distortion from expansion during heating of the casting.42 Indexing the separate pieces also requires greater time, and the patient must return for another appointment after the laboratory process of soldering, which includes an additional laboratory fee.
Progressive Loading
The bone around an implant takes 1 year or more to obtain its full strength. As a consequence of the surgery, the bone remodels with woven bone (the bone of repair), which is 60% mineralized and is less organized than lamellar (load-bearing) bone. In addition, the strength of bone is often increased after loading in response to the microstrain conditions that change within the bone cell. A gradual loading process to the bone may increase the bone strength and delay the full occlusal load until the bone is stronger.43 A bilateral comparative study demonstrated that even single-tooth implants sustained greater crestal bone loss and exhibited less dense bone when they were not loaded gradually compared with progressively loaded restorations.44
The transitional restoration for a screw-retained fixed prosthesis is more difficult to fabricate. As a result, dentists often do not fabricate a transitional restoration in nonesthetic regions or maintain the same removable prosthesis during the fabrication of the final restoration as was used during implant healing. And even when a screw-retained transitional is fabricated, it is not completely passive. As a result, the implant-to-bone interface is not loaded gradually to improve its density. Instead, the implant-to-bone interface is initially loaded when the nonpassive screw-retained prosthesis is inserted. A screw-retained prosthesis presents difficulty in progressively loading the bone because of the misfit factors for a zero tolerance system as previously discussed.
A cement-retained transitional prosthesis may be used before the delivery of the cement-retained final restoration and gradually load the implant-to-bone interface with acrylic occlusals and gradually increase occlusal contacts over an extended time frame. This protocol does not affect the properties of the final prosthesis retention and leads to an increase in bone density and strength.
Axial Load
A cement-retained implant prosthesis and the implant body may be loaded axially, thus decreasing crestal bone loads. The decrease in crestal bone strain may reduce the incidence of bone loss.45,46 In addition, the literature has provided evidence that offset loading may cause increased incidence of component failure or screw loosening.47,48
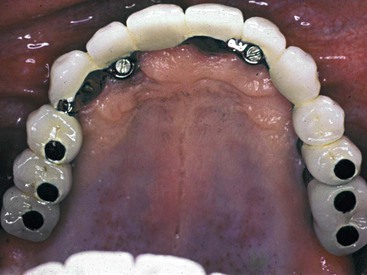
In contrast, the axial occlusal load on a screw-retained restoration must load the occlusal screw region. Screw holes are usually 3 mm in diameter, representing 30% or more of the total occlusal surface of posterior teeth and 50% of their functional area because only two thirds of the occlusal table is in the functional regions of loads.20 Occlusal screws are usually in the ideal location (along the long axis) for primary occlusal contact45 (Figure 26-16). Most manufacturers suggest the placement of a composite occlusal restoration over the screw access hole or offset loading the crown lateral to the occlusal screw region. To direct loads along the long axis of the implant body with a screw-retained crown, occlusal adjustments are made on the occlusal composite obturation placed over the top of the screw. These restorations require additional chair time and wear more rapidly than porcelain or metal, which is the occlusal contact material of choice for a cement-retained restoration. Anterior restorations that are screw retained cannot be loaded as ideally as cemented prostheses. The prosthesis fixation screw is often placed in the cingulum area.
A related advantage is that cemented restorations permit the design of narrow occlusal tables because no minimum dimensions are required for screw holes and surrounding metal. This in turn proves a valuable advantage to prevent overcontouring and promote the design of an emergence profile favorable to periimplant tissue health.
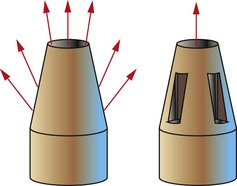
Hygiene of the Implant Sulcus
A screw-retained restoration does not fit the abutment or implant body with a hermetic seal. Therefore, a screw-retained prosthesis does not seal the abutment-to-crown interface or margin, which may harbor bacteria in the crevice (Figure 26-17). The crevice may even act as an endotoxin pump if the components are flexing under load, encouraging the proliferation of microorganisms in the sulcular region.49,50 This is especially a concern in a subgingival margin. When these screw-retained components are disassembled, the dentist often smells an odor indicative of anaerobic bacteria activity. A cemented crown seals the crown–abutment connection and impairs bacteria penetration.
A screw-retained restoration in the anterior region or in the esthetic zone usually requires the abutment for screw retention to be positioned in the cingulum or the central fossa region of the crown. As a consequence, the facial aspect of the implant crown is cantilevered from the implant with a ridge lap of porcelain, which complicates hygiene procedures at the facial cervical region51 (Figure 26-18). The emergence profile of an anterior cemented crown does not require a facial porcelain ridge lap because the implant may be placed under the incisal edge rather than the cingulum. This also facilitates the achievement of an esthetic result.
Esthetics
An abutment for cement retention angulated slightly too facially often may be prepared as a natural tooth. The implant body even may be prepared to this effect. A screw-retained restoration on an implant placed slightly too facial may not be able to be modified. Hence, the esthetic aspect of the restoration may be compromised.52 The occlusal holes in the posterior screw-retained restorations require occlusal restorations to avoid an unesthetic result. Even when composite is placed into the access holes, the restoration is less esthetic. The occlusal aspect of a cement-retained crown is all porcelain and is more esthetic.
Occlusal Material Fracture
The third most common complication for fixed prostheses on natural teeth is porcelain fracture.4,5 Occlusal material fracture is more common with implants than natural teeth because of the lack of periodontal stress relief with implants and a resultant higher impact force to the occlusal material.23 A decreased incidence of porcelain or acrylic fracture of the prosthesis has been observed with cement-retained restorations compared with screw-retained prostheses. The screw hole may increase stress concentration to the restoring material and more often leads to unsupported porcelain (Figure 26-19). For example, a study presented by Nissan et al. examined the porcelain fracture incidence of screw-retained restorations compared with cemented prostheses.53 The study used a split-mouth evaluation for bilateral edentulous sites in partially edentulous patients. Ceramic fracture was 38% for screw-retained versus 4% for cemented prostheses. The mean loading period for these restorations was 5 years.

After the material fractures, the repaired site is weaker than its original strength, and recurrent fractures are more common. The patient’s concerns and psychological comfort with the prosthesis often are affected. A cement-retained prosthesis does not have a weak link through the surface of the occlusal material.
Access
Access is more challenging in the posterior regions of the mouth for insertion of screw-retained restorations, especially in patients with limited jaw opening. The screwdrivers to place and torque the prosthetic screws are usually greater than 15 mm in height. The manipulation of small screws and screwdrivers is far more time consuming and challenging than the abutment preparation and cementation of a cemented restoration.
When a screw or screwdriver is dropped in the posterior regions of the mouth, the patient may swallow or aspirate the device.54–56 This is a greater risk when working in the posterior region; small components are not magnetic because precious metals or titanium is used for the screws, so a functional fit is necessary to carry them to the receptor site, and they often become dislodged.
Component Fracture
A long-term complication of screw-retained prostheses is fatigue failure of the screw components.23,57 The narrow diameter of the prosthesis screw reduces its long-term strength. The bending fracture resistance for a solid object is π/4(R4).58 In other words, a screw twice the diameter is 16 times stronger. Because the diameter of the occlusal screw is the smallest of any implant component, the screw is most at risk for breakage (Figure 26-20).

Fatigue fracture is related to the number of cycles of load. The fatigue or endurance limit is about half the ultimate strength of a material. The prosthesis screws receive increased cyclic loads under parafunction. As a result, the coping screws are at long-term risk of fracture or loosening. These complications account for many of those encountered in screw-retained prostheses with screw loosening reported in up to 38% of the posterior single-tooth restorations.59,60 Screw loosening increases the force to any other implant still part of the support system of the prosthesis and may lead to additional prosthesis screw complications, abutment screw loosening or fracture, and even implant body fracture for components that remain connected.
Wearing of the threads from screw loosening may occur when the restoration is removed and reinserted repeatedly over several years or when retorqued after loosening. As a result, screw fracture and component loosening may increase in long-term restorations. Cemented prostheses have no small-diameter components and no metal-to-metal wearing; as such, similar complications are not observed.
Cost and Time
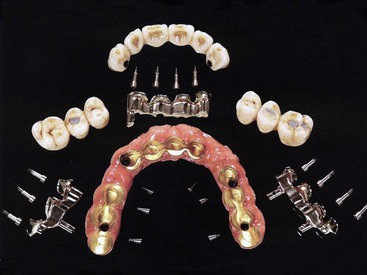
The laboratory costs for a screw-retained restoration are greater than those for a cemented prosthesis.17,60 Screw-retained restorations require additional laboratory components such as impression transfers, analogs, copings, and screws (Figure 26-21). As a consequence, implant manufacturers may generate four times more profit in screw-retained restorations compared with cement-retained restorations. In addition, laboratory components and time are increased to fabricate the prosthesis. Consequently, laboratory costs are 1.5 to 2 times higher than for a cemented restoration.
Fewer and shorter prosthetic appointments are required to restore a patient with a cemented prosthesis than with a screw-retained restoration.61 Passive castings, progressive loading, and esthetics management are less complex for cemented prostheses.
Advantages of Screw-Retained Prostheses
There are several advantages to a screw-retained prosthesis as compared with a cement-retained restoration. These include low-profile retention, reduced moment forces with overdentures, reduced risk of residual cement, and splinting nonparallel abutments (Box 26-2).
Low-Profile Retention
The primary advantage of a screw-retained superstructure is the lower profile retention of the abutment system.62 Cemented prostheses require a vertical component of at least 5 mm to provide retention and resistance form.63 A crown height reduction of 2 mm may decrease the retention as much as 40% when the implant abutment is only 4 mm in diameter.18 The screw-retained system is more resistant to removal forces than the cement abutment when the abutment height is less than 5 mm. The low-profile abutment may also offer significant advantages for removable prostheses (RP-4 or RP-5) (Figure 26-22). The lower height of the superstructure permits easier placement of denture teeth. The greater volume of acrylic also increases the strength of the acrylic portion of the restoration.
On occasion, low-profile retention is required for posterior fixed prostheses with short crown height. However, in such conditions, the space required to insert a screwdriver may be a limitation not appreciated until the prosthetic appointment. The prosthesis should be screw retained if the crown height does not allow sufficient abutment height and surface for cementation.
Osteoplasty before implant placement can increase the abutment height to improve the retention of the cemented fixed prosthesis. However, the dentist must consider the decrease in implant body height. In addition, a gingivoplasty after osteoplasty almost always is indicated to decrease sulcular depth and improve oral hygiene conditions. The dentist also may consider placement of additional implants and abutments or a customized abutment to increase cement retention.
An abutment with reduced height may be required when the implant is positioned too lingual or palatal (Figure 26-23). A 5-mm or greater height of the abutment may interfere with a tongue position or occlusion.
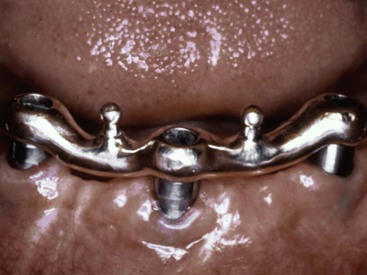
Reduced Moments of Force
A screw-retained superstructure bar for a RP-5 overdenture (implant and soft tissue support) may be subjected to less moment forces during prosthesis movement. The moment force to the implant is reduced with a low-profile abutment when stress breakers on the superstructure separate the removable prosthesis from the implant support (Figure 26-24). These elements decrease the effect of lateral loads on the implant body.
Risk of Residual Cement in the Sulcus
Another advantage of screw-retained crowns is the absence of residual cement in the gingival crevice, which may cause irritation to the surrounding tissues and lead to increased plaque retention and inflammation, similar to an excess cement condition with crowns on natural teeth.64
When possible, the crown margin of a cement-retained prosthesis should be above the tissue so that cement excess can be readily removed. Subgingival margins increase the incidence of incomplete cement removal on teeth or implant abutments. The cement may remain embedded deeper into the sulcus of the implant abutment because of the less tenacious junctional epithelial tissue and the lack of connective tissue attachment compared with a natural tooth.
Nonparallel Implants
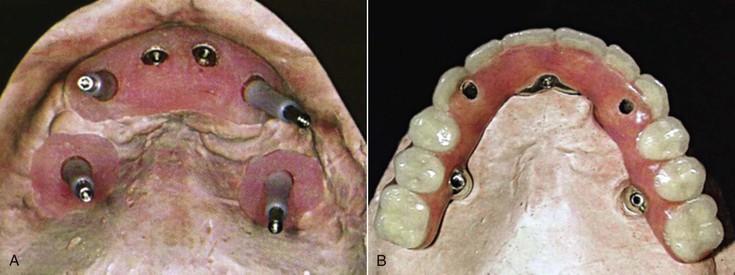
When implant bodies are unparallel by more than 30 degrees, an abutment for cement retention cannot be adequately prepared for a path of insertion. A low-profile screw abutment may engage the implant bodies at significant angles. For example, a pterygoid or zygomatic implant may be placed at 45 degrees from anterior implants, yet these implants may be splinted together with a screw-retained restoration (Figure 26-25).
Therefore, greater low-profile retention, reduced moment force in RP-5 overdentures, greater space for denture teeth or occlusal materials, and absence of cement residues are advantages for screw-retained superstructures. Most of these conditions are more characteristic of implant-supported overdentures than fixed restorations.
An interesting note is that in the mid 1980s and 1990s, practitioners who challenged the concept of implant-supported, cement-retained restorations were regarded as a minority. Over the past decades, the profession has reassessed its position, and today most fixed prostheses on implants (≈90%) are restored with cement-retained restorations rather than screw-retained prostheses.20,60,65
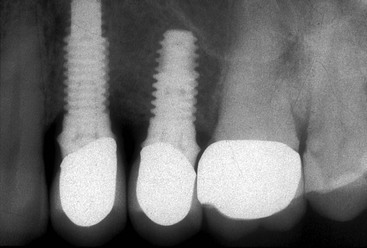
Complications of Cemented Prostheses
Residual Cement
The most common complication of a cement-retained implant restoration is residual cement left in the gingival sulcus of the implant65 (Figure 26-26). Residual cement in the sulcus after cementation of the prosthesis is a source of periimplantitis.64,66,67 The occurrence of this complication is more often found with implants than natural teeth. In a report by Wilson, excess dental cement was found in 81% of patients with clinical or radiologic signs of periimplant disease.68 Hence, this complication has led some practitioners to encourage screw-retained restorations.
There are several reasons why implant prostheses have more residual cement complications than natural teeth. They primarily include the position of the prosthetic margin in relation to the free gingival margin and a difference in the sulcular attachment to the implant or tooth.
Difference in Gingival Attachment
The natural tooth–to–soft tissue interface includes (1) the sulcus, (2) the junctional epithelial attachment, and (3) the connective tissue attachment. Each of these three zones is approximately 1 mm in height at the midfacial and lingual tooth position. A periodontal probe inserted into the soft tissue crevice will go through the sulcus and the epithelial attachment zones. The periodontal probe stops at the connective tissue attachment region because six of the 11 fiber groups in the soft tissue physically insert into the cementation of the tooth (Figure 26-27). Hence, if excess cement is expressed into the gingival crevice, it does not extend to the level of the bone.
An implant–soft tissue interface does not have a connective tissue attachment zone. A dental probe introduced into the crevice may proceed to the level of the bone. Hence, there is no barrier to prevent excess cement from extending deeper into the soft tissue region (Figure 26-28).
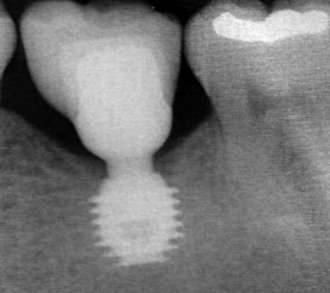
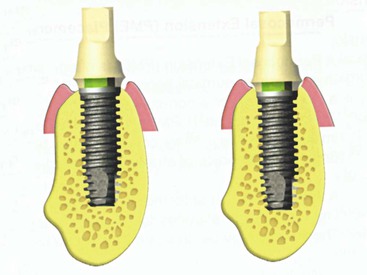
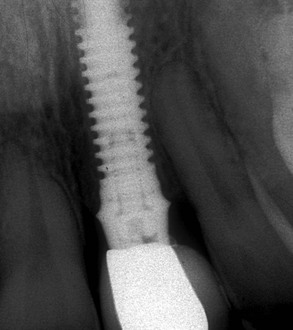
In addition, the gingival crevice of an implant may be more than 3 mm in depth, especially in the interproximal region because a scallop of bone does not exist around an implant (compared with a 3-mm incisal scallop of an anterior natural tooth). The tissues on the crest of the ridge may also be thicker than 3 mm even on the midfacial and palatal regions. As a result, the sulcular depth of an implant may be more than 3 mm thick, especially in the maxilla. When the implant platform is positioned below the bone, the bone loss below the abutment connection also increases the sulcus depth (Figure 26-29). As such, the extrusion of excess cement may extend many millimeters below the free gingival margin of an implant crown.
Position of a Crown Margin
There are seven indications for a subgingival margin in prosthetics: existing caries, to replace a previous restoration with a subgingival margin, to increase retention, to improve esthetics, subgingival tooth fracture, to correct cervical defects, and to reduce root sensitivity69 (Box 26-3).
Implant restorations do not decay or have cervical defects or tooth fractures. Hence, in cemented implant restorations, the margin of the crown should be at or above the free gingival margin out of the esthetic zone when increased abutment height is not necessary to increase retention.18 This would permit easy access to the crown margin to remove any excess cement.
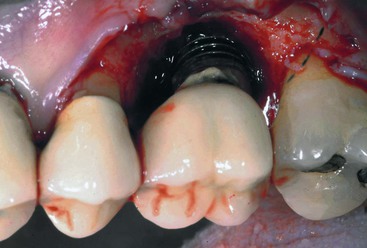
When a subgingival margin is indicated in a restoration, it should not proceed more than 1.0 mm ± 0.5 mm into the sulcus.69,70,71 Unfortunately, many practitioners (and laboratories) attempt to place the implant crown margin at the abutment flare of an implant abutment for cement. Because the abutment is usually wider than the implant body dimension and then tapers to the incisal portion, the implant abutment flare appears to many dentists as a crown margin (Figure 26-30).

The flare of an implant abutment is often placed near the crest of the residual bone, especially when the implant body is countersunk below the crest of the residual bone (Figure 26-31). As a consequence, the restoring dentist has difficulty in capturing the “margin” of the abutment flare in an impression because it may reside more than 2 mm below the free gingival margin, especially in the interproximal region.
To capture the abutment flare (“margin”) of the abutment several millimeters below the tissue, the dentist often makes an implant body transfer impression to capture the position of the implant body. The laboratory, whether it is using a dental impression of the “margin” or a stock abutment for cement retention with an implant body impression, places the crown margin to the abutment flare, several millimeters below the gingival margin.
When the dentist attempts to seat the implant crown several millimeters below the tissue, the subgingival crown contour pushes the tissue away from the abutment, which often prevents the crown from being passively seated, and the tissue pushes the crown and elevates its position from the “margin.” As a result, the dentist often cements the restoration before evaluation of the occlusion or esthetics. Hence, an occlusal adjustment or esthetic try-in is not accomplished before cementation.
When excess cement extrudes from the subgingival crown “margin,” it then extends beyond the abutment flare into a subgingival undercut of the abutment (Figure 26-32). Because the margin is several millimeters below the free gingival margin and in an undercut below the flare, the dentist has difficulty removing the excess cement.
An alternative to this problem selected by many dentists and laboratories is for an implant body transfer and analog with an indirect laboratory technique followed by the fabrication of a customized abutment. The customized post is designed with the crown margin 1 mm below the free gingival margin (Figure 26-33). Hence, the crown may be passively seated, the esthetics and occlusion modified as needed, and the excess cement able to be more easily removed. This option is often encouraged by dental laboratories and implant manufacturers because this technique is associated with a greater laboratory fee, and the purchase of a transfer coping and an analog is necessary.
All of the problems of difficult impression making, increased laboratory and implant company fees, difficulty in seating the restoration, and residual excess cement stem from the dentist (and laboratory technician) believing the abutment for cement flare is a crown margin. The abutment flare is not a “margin” for a crown; rather, it is a biomechanical feature to increase abutment taper, increase crown retention, and increase strength of the abutment wall. It can also improve the subgingival cervical contour of the tissue, which improves the emergence profile of a crown to improve the cervical esthetics (Box 26-4).
The Abutment Flare
The wider the base of an abutment, the more taper may be placed on the abutment. Because the implant body has a smaller diameter than the tooth it replaces, the amount of taper is reduced. A limiting factor of the abutment taper is the outer wall of the abutment at the incisal aspect. The abutment for cement retention has a fixation screw hole 2.5 mm in diameter, so the abutment screw may enter and fixate the abutment to the implant body (Figure 26-34). As a consequence, a 3.5-mm-diameter abutment at the base may have a taper of only 5 degrees. A 6-mm-wide abutment at the base may have a taper of 25 degrees. The greater the taper, the easier it is for the dentist to splint implants together or have a path of insertion for the prosthesis. When the cervical aspect of the abutment is 3 to 4 mm in diameter (and is similar to the implant body dimension), the taper of the abutment is limited to 5 to 10 degrees. This makes it almost impossible to splint implant crowns together and makes it necessary for the implant body position to be similar to the path of insertion of the crown. Hence, the abutment flare is designed because it is wider than the implant body, so the taper may be greater.
The wider an abutment, the more surface area for cement and the greater the retention of a cemented crown. Hence, when the abutment is wider than the implant body, the cement retention is increased. The greater the retention, the less hard the cement requirements in shear and tension used to retain the restoration. Hence, the restoration may be more easily removed to correct a prosthetic complication.
The more metal dimension flanking the abutment fixation screw hole, the greater the strength of the abutment to prevent fracture. When the cervical aspect of the abutment for cement retention is wider than the implant body, the strength of the abutment to prevent fracture is dramatically increased. An abutment for cement may be compared to an open cylinder in mechanics. The strength of an open cylinder is π4(R4 − RI4), where R is the outer radius and RI is the inner radius.52 In other words, small changes of the outer diameter of the abutment increase the strength of the abutment to the power of four times.
The wider abutment at the base allows the subgingival contour to be increased and improves the emergence profile of the crown to be more similar to a natural tooth. Because the implant body is smaller than the tooth it replaces, a wider abutment permits the crown to have a greater emergence profile.
As a consequence of the biomechanical advantages of a wider cervical portion of an abutment and improved emergence profile, there is an undercut from the abutment flare to the implant body. This feature increases the difficulty to remove residual cement beyond the crown margin when the margin is positioned at the abutment flare.
Instead of positioning the crown margin at the implant abutment flare, the crown margin should be positioned at the gingival sulcus (or above) when it is out of the esthetic zone, or no more than 1.5 mm below the free gingival margin of the sulcus (for esthetics or for more retention). The crown margin preparation may be a knife edge because the abutment is narrower than the tooth it replaces (Figure 26-35). Hence, the crown margin may more easily be captured in the impression, a stock abutment may be used, a stone die may be used to fabricate the crown, the crown may more easily be passively seated to check or modify occlusion or esthetics, and the residual cement may more easily be removed from the crown margin (Figure 26-36).
In conclusion, when the flare of the implant abutment is within 1.0 mm ± 0.5 mm of the gingival margin, it may be used as the crown margin. When the abutment flare is more than 1.5 mm below the tissue margin, it may remain below the tissue and crown margin with no consequence. There is no report indicating the subgingival abutment flare below the crown margin increases any risk of plaque retention or gingival shrinkage or contributes to crestal bone loss. If the abutment flare is above the gingival margin of the tissue as a result of gingival shrinkage or the implant body protruding several millimeters above the bone and a subgingival margin is desired, the abutment flare may be prepared to place the crown margin below the margin of the tissue (Figure 26-37).
Abutment Retention
Uncemented restorations on natural teeth are one of the most common complications of fixed prostheses.4,5 After the crown on the natural abutment becomes uncemented, a significant concern is caries. Decay may proceed rapidly and result in loss of the abutment, creating a need for endodontic treatment, post and core, a new prosthesis, or an abutment with even poorer retention. These same conditions exist if the natural retainer becomes uncemented from an implant–tooth restoration.
The implant abutment is at greater risk of uncementation than a natural tooth (Figure 26-38). The implant abutment is made of metal, so dental cements do not adhere to the interface as with dentin of a natural tooth. The porosity of an implant abutment is usually less than a tooth. The implant abutment is usually smaller in diameter and usually has less surface area than a natural tooth. The dentist often desires to make the restoration retrievable to more easily handle future complications. As such, a softer cement is often used for implant crowns. In addition, there is greater impact force to a cement–abutment interface for implant prostheses compared with natural tooth abutments. The partially retained implant fixed prosthesis then acts as a cantilever with a dramatic increase in moment force on the implant(s) that still retain the prosthesis. Crestal bone loss, prosthesis or abutment screw fracture, implant fracture, or mobility and failure of the implant are likely complications.
The principles of retention and resistance may be addressed specifically for both natural teeth and implant abutments. The retention features of a fixed-cemented restoration resist the removal of the retainer along the path of insertion. The forces applied to remove the crown in this direction are primarily shear or tensile forces on cement. The resistance of a crown opposes the movement of the abutment under occlusal loads and prevents removal of the restoration by forces applied in an apical or oblique direction. These are primarily compressive and tensile forces on cement. As with most materials, cements exhibit lower retention strengths compared with their resistance strengths (e.g., zinc phosphate exhibits greater than 100-MPa compression strength and only 5- to 9-MPa tensile strength).69
Specific features in the geometric configuration of the implant abutment for cement retention or a prepared tooth are requisites to avoid uncementation. The tenets of retention and resistance of fixed prosthodontics are directly applicable to implant abutments and include taper, surface area, height, the geometry of the abutment preparation, surface roughness, and luting agents70–72 (Box 26-5).
Abutment Taper
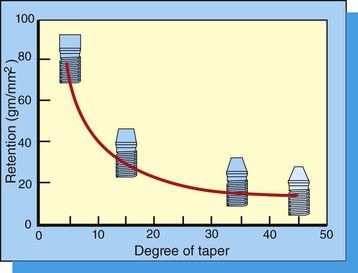
The retention of a crown rapidly decreases as the taper is increased from 6 to 25 degrees.71 (Figure 26-39). Taper degree is the sum of both sides of the preparation. A typical tapered diamond bur shows a taper of about 3 degrees on each side or a 6-degree total taper. The parallelism of the axial walls has been recognized to be the single most effective factor for retention.73 The ideal taper originally was recommended to be within 2 to 5 degrees of parallelism of the path of insertion, which also was placing minimal stress concentrations on prepared abutments.69 However, clinically acceptable preparations present a taper in the range of 20 degrees.73–75
Premanufactured stock implant abutments for cement may exhibit a total taper from 10 to an excess of 30 degrees. As a result, the retentive surfaces of some more tapered, unprepared implant abutments may provide less retention than natural abutments. Therefore, the preparation in the cervical third of the abutment near the crown margins may be indicated in the more tapered implant abutments to reduce the taper even when the path of insertion is satisfactory.
Abutment Surface Area
The parameters of retention are similar for a tooth or implant and mainly are influenced by the diameter and height of the abutment.76 The surface area of an implant abutment influences the amount of retention. A linear increase in retention occurs as the diameter increases for preparations with identical height, and a wider abutment offers greater retention than a narrower abutment77 (Figure 26-40). Molars are more retentive than premolars because of their increased surface area, all other factors being equal. It should be noted that controversy exists as to whether the increased surface area is responsible for the increased retention or whether the height-to-width ratio is more relevant.78–80
The diameter of an implant abutment for cement retention is often less than 5 mm, which is comparable to that of a prepared lateral incisor. Therefore, the decreased surface area results in poorer retention than most natural abutments. In addition, cements do not adhere as well to titanium as they do to prepared dentin. As a result, additional retention features for an implant abutment should often be incorporated.
Wider implant abutments have more retention than standard-size abutments. The wider abutment usually is obtained by two methods. First, a wider implant body has a wider abutment for cement than a smaller-diameter implant. Second, the abutment may have a wider emergence design than the implant body (or abutment flare). The greater-diameter abutment has advantages of providing a greater taper, a thicker outer body wall, and more surface area for retention.
Abutment Height
A tall preparation provides greater retention than a short abutment.76,81 An additional 2 mm of height may increase retention up to 40%, especially when the abutment is only 4 mm in diameter. The increase in height and the height-to-width ratio are determinants for retention. An increase in height from 4 to 7 mm results in a 67% increase in retention.18 When the height of the implant abutment is less than 5 mm, the diameter of the implant abutment is more critical to improve cement retention or resistance. A customized abutment, larger in diameter than the stock abutment, may be necessary to retain the restoration.
The additional abutment height not only increases the surface area, which increases retention, but also increases resistance because it places more axial walls under compressive and tensile stress rather than shear stress. Therefore, the retention and the resistance are increased, which decreases the risk of uncementation.
Limited natural tooth crown height (because of limited interarch space or short clinical crown) also decreases retention. Splinting of natural teeth with limited crown height to improve retention often compromises access for hygiene in the interproximal areas. Instead, crown lengthening is often indicated in case of limited interarch space to improve the retention of the prosthesis and the esthetic result without compromising home care. Crowns of reduced size require minimal tapering and additional retentive elements such as grooves or boxes to limit the path of insertion and direction of dislodgement.69,81
Geometry of Abutment
The strength of the cement interface is weakest under the shear component of a force. The surface area of an abutment submitted to shear forces is more critical than the total surface area under tensile force.69,81 Manufactured implant abutments for cement are usually circular in cross-section, providing little resistance to shear forces, especially on individual, unsplinted crowns. A flat side on the implant abutment preparation decreases shear forces on the cement interface. Whenever possible, a preparation with one or two flat sides should be made on circular abutments for cemented prostheses.
A tapered implant abutment post may provide multiple paths of insertion or removal. The addition of one or more parallel-sided grooves to an abutment limits the path of withdrawal of the crown to one direction69,82 (Figure 26-41). Therefore, whenever possible, retentive elements such as grooves parallel to the path of insertion, should be added to a short or excessively tapered implant abutment for cement. Additional grooves parallel to the path of insertion mechanically resist rotational forces, place compressive forces on the cement in these regions, and dramatically improve cementation83 (Figure 26-42). The outer wall of some two-piece abutments may be thin. As such, a groove may perforate or weaken the component.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses