Interrelationship of Orthodontics with Periodontics and Restorative Dentistry
Vincent G. Kokich, Vincent O. Kokich
Today, orthodontics is not just for children and adolescents. For the past two decades, increasing numbers of adults have been referred to orthodontists to correct their malocclusions. Adults are usually wonderful patients because they are cooperative, clean their teeth, show up for appointments, and are appreciative of the clinician’s efforts. However, adults may have problems other than malposed teeth and jaws that make their orthodontic treatment more challenging. Whereas children and adolescents have intact dentitions with few restorations and a healthy periodontium, adults may have old failing restorations, edentulous spaces, abraded teeth, periodontal bone defects, gingival level discrepancies, hopeless teeth, and a variety of other restorative and periodontal problems that could compromise the orthodontic result. In the past orthodontists made all decisions about the treatment plan for a child or adolescent. However, in the compromised adult malocclusion, a team consisting of an orthodontist, oral and maxillofacial surgeon, periodontist, endodontist, and restorative dentist must interact to make prudent treatment decisions for the patient.
This chapter elucidates the dilemmas encountered in the orthodontic patient with multidisciplinary problems and describes a series of 10 guidelines to help manage the interrelationship of orthodontics with periodontics and restorative dentistry.
Generate Realistic Treatment Objectives
The first step in any type of dental therapy is to establish the treatment objectives. It is impossible to achieve the correct end result if the appropriate goals or objectives have not been identified before treatment. In nonrestored, adolescent patients with complete dentitions, orthodontic treatment objectives tend to be idealistic. After all, if patients have intact dentitions without restorations, it is appropriate to expect that ideal esthetic and occlusal treatment should be attainable, if the patient cooperates. Because of this tendency, most orthodontists are trapped into applying these same idealistic treatment objectives to adult patients with missing teeth, abraded teeth, old restorations, or other restorative and periodontal complications. Idealistic treatment objectives may not be appropriate for ortho-perio-restorative patients. For these patients it is important to establish realistic, not idealistic, treatment objectives. Realistic treatment objectives generally should be economically realistic, occlusally realistic, periodontally realistic, and restoratively realistic.1
If an adult orthodontic patient is missing several teeth, the edentulous spaces created during orthodontic treatment will require restoration after the removal of the orthodontic appliances. Several restorative alternatives may exist to replace the missing teeth. The cost of these restorative treatment plans may differ widely. Furthermore, each type of restoration may require slightly different tooth positioning. Therefore it is mandatory for the team to establish a treatment plan that is economically realistic for each patient. If the team fails to establish economically realistic objectives, the patient might not complete the restorative treatment following orthodontic therapy.
In young patients it is important to establish ideal occlusal objectives, such as a Class I canine relationship with normal overbite and overjet relationships. When planning occlusal treatment for young patients, the orthodontist is missing two critically important pieces of information: (1) because of their young age, there is no occlusal history and (2) the orthodontist unfortunately cannot predict the future habits or problems that a young patient will encounter during his or her lifetime. Therefore in these situations it is appropriate for the orthodontist to create an ideal occlusion. However, in the adult patient, orthodontists often overlook the most valuable piece of information: the patient’s dental history. Has the adult patient demonstrated parafunctional occlusal habits, evidence of temporomandibular disorders, cracked teeth or restorations, wear facets, abraded incisors, or other signs and symptoms that would suggest that the treatment plan should alter the existing occlusion? Not all existing occlusions in adult patients need to be corrected to an adolescent ideal (Fig. 26-1). In all adult patients the dental history, as well as the future restorative requirements, plays a greater role in determining the final occlusion (Fig. 26-2). For example, it may not be necessary to correct posterior crossbites in adults who have no occlusal interferences and no shift of the mandible and who can be restored adequately in a posterior crossbite relationship (Fig. 26-3).
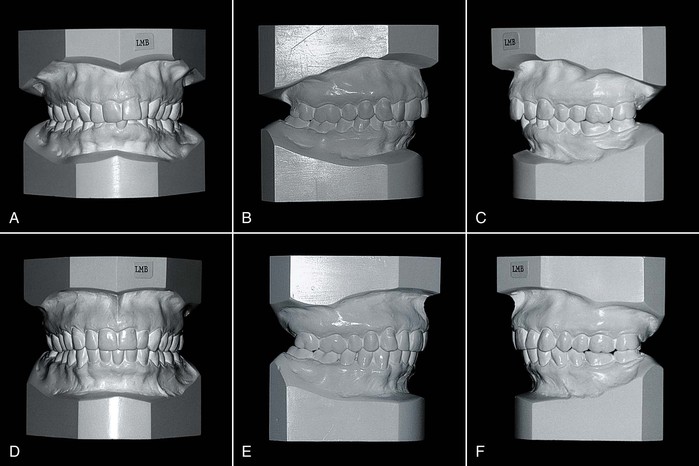
Figure 26-1 A 68-year-old female had (A) a deep anterior overbite with (B) Class I molar and canine relationships on the right and (C) Class II molar and canine relationships on the left. She had no temporomandibular joint symptoms and a healthy periodontium. D, Treatment objectives included alignment of teeth in both arches and reduction of the deep overbite. Because of an anterior tooth size discrepancy, proclined mandibular incisors, and upright maxillary incisors, her treatment objectives did not include correction of the Class II molar and canine relationships on the left. E and F, At the end of treatment all treatment objectives were achieved, including maintaining the original posterior occlusal relationships.
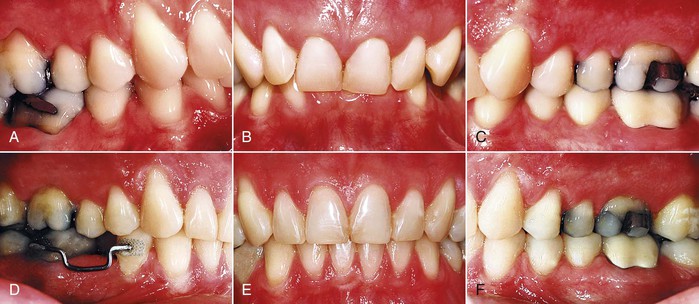
Figure 26-2 A 52-year-old male had (A) a bilateral Class II, Division 2 malocclusion with a deep anterior overbite, (B and C) retroclined maxillary incisors, a missing mandibular second premolar, and a mandibular dental midline that deviated to the right. The patient had no temporomandibular joint symptoms and the periodontium was healthy. Treatment objectives included (D) reduction of the deep overbite, opening space for the missing premolar, correction of the dental midline, and establishing normal overjet. Because of the inclination of the anterior teeth and the anterior tooth size relationships, (E) a Class I canine relationship was established on the right and (F) a Class II relationship was maintained on the left. The objectives were achieved without correcting the Class II canine relationship on the right side.
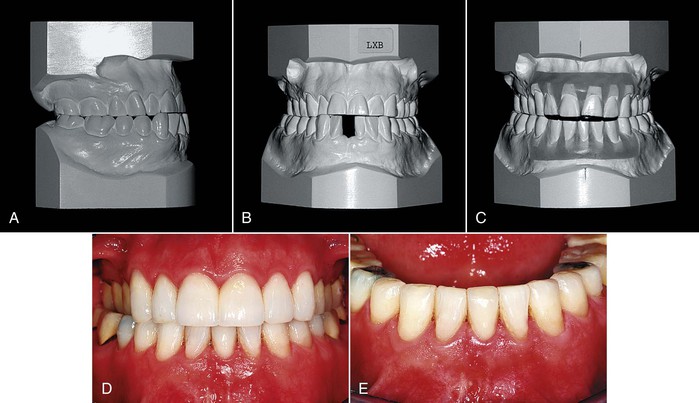
Figure 26-3 A 57-year-old male had (A) a Class III end-to-end posterior occlusion with an anterior dental crossbite, a missing mandibular incisor (failed endodontic therapy), severe wear of the maxillary incisors, and (B) bilateral posterior dental crossbites with no lateral shift of the mandible. He had no temporomandibular joint symptoms and the periodontium was healthy. Treatment objectives included correction of the anterior crossbite to create an overjet to restore the abraded maxillary incisors. Correction of the bilateral dental crossbites was not a treatment objective. C, A diagnostic setup showed that the mandibular space could be closed to create restorative space. The final photographs of the restored (D) maxillary and (E) mandibular incisors show that correction of the posterior crossbites was not necessary to achieve the restorative objectives.
If patients are missing many teeth, it may not be prudent to establish idealistic occlusal objectives. An ideal Class I posterior occlusion is achievable in a patient with a complete nonrestored, nonabraded dentition. However, if the patient is missing several teeth and will require extensive restorative treatment after orthodontics, it may be more prudent to establish treatment objectives that are occlusally realistic for the specific patient. For example, if the patient will require extensive restorations after orthodontic treatment, the restorative dentist may suggest altering a Class I occlusion to facilitate restoration of the teeth (Fig. 26-4). It is critical for the orthodontist to be aware of these alterations before bracket placement to achieve an occlusally realistic relationship for the restorative patient.1
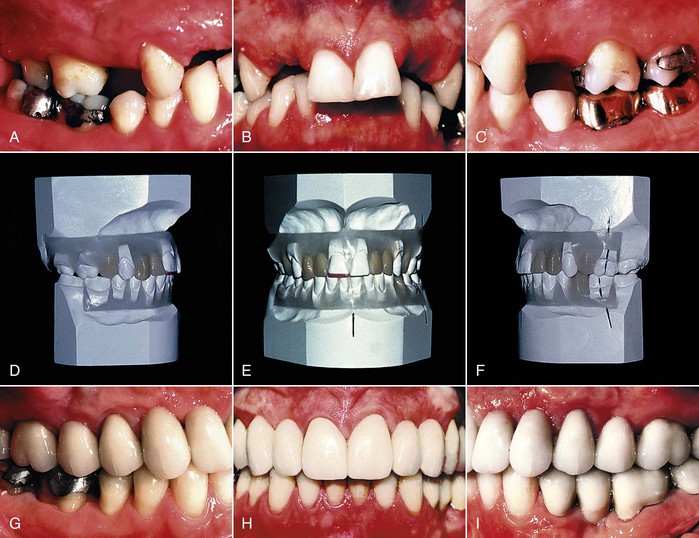
Figure 26-4 A–C, A 32-year-old female had a Class II, Division 1 malocclusion with a deep anterior overbite. She was congenitally missing both maxillary lateral incisors and all four maxillary premolars. The restorative dentist wanted the maxillary canines positioned in the first premolar positions in order to restore the maxillary arch with three segments of fixed restorations connected at the canines with a semirigid connector. D–F, A diagnostic wax setup provided the guide for the orthodontist to position the canines in their appropriate position. G–I, After the final restorations were placed, the widths of the pontics and abutments in the maxillary arch were functionally and esthetically correct because the vision had been created with the diagnostic setup.
A common occlusal treatment objective in children is to align the marginal ridges of the posterior teeth in order to produce a uniform vertical relationship between the maxillary and mandibular posterior teeth.2 In a nonabraded, periodontally healthy adolescent dentition, aligning the marginal ridges helps to establish even contact of the posterior teeth, when they are brought into occlusion. However, in the adult patient with interproximal bone loss and uneven wear of the posterior teeth, the marginal ridges are poor guides for positioning the posterior teeth.3 In these patients the periodontal objectives outweigh the occlusal objectives. The role of the orthodontist in the periodontal patient is to level the bone during orthodontic treatment. This could require equilibration and reshaping of the posterior teeth in order to maximize the occlusal contacts. In most of these situations the teeth that have been equilibrated will require restoration anyway after orthodontic treatment.
Certain types of restorations require specific positioning of adjacent or opposing teeth. As a result, orthodontists must not establish idealistic treatment objectives for patients who will require extensive restoration. If teeth are worn or abraded, it may be more important to position the teeth in a restoratively realistic location to facilitate the appropriate restoration.
Create the Vision
After an orthodontist has treated several hundred adolescent patients with complete dentitions, it is easy for him or her to visualize or foresee the final orthodontic result before beginning treatment. However, some adult orthodontic patients may be missing several permanent teeth. If teeth have been absent for several years, the remaining teeth may have drifted. In other situations it may be necessary to position teeth in unusual situations. These patients may require a combination of orthodontics and restorative dentistry to rehabilitate their occlusion. In these patients it may be difficult for the orthodontist to visualize or foresee the final result, as he or she may not be aware of the restorative requirements or the eventual restorative treatment plan. Similarly, it may be difficult for the restorative dentist to visualize the final result, as he or she may be unaware of the orthodontic possibilities.
However, it is possible to predetermine the final occlusal and restorative outcome by completing a diagnostic wax setup for these types of patients. A diagnostic setup is mandatory for any patient who is missing multiple permanent teeth4 and will require a combination of orthodontics and restorative dentistry (see Fig. 26-4). In addition, patients who will have implants used first for orthodontic anchorage and later for restorative abutments will require a diagnostic setup5 to position the implants properly prior to the beginning of orthodontics (Fig. 26-5). The orthodontist should never make the restorative decisions but rather should consult with the restorative dentist when planning treatment for these types of patients. In that way the orthodontist may reposition the teeth to simulate realistic orthodontic objectives that will be in harmony with the patient’s restorative requirements. Both practitioner and patient can visualize the result. The diagnostic wax setup is the blueprint for treatment in these types of patients.
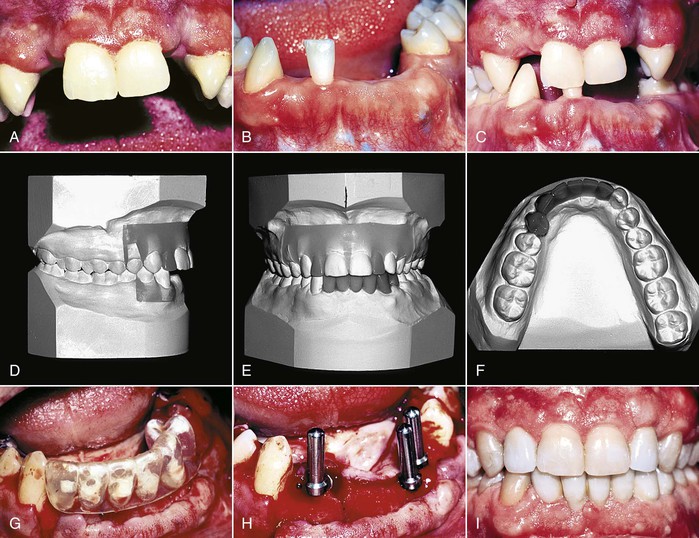
Figure 26-5 A 24-year-old male was the victim of a robbery during which he was shot in the face and lost (A) his maxillary lateral incisors and (B) most of his mandibular anterior teeth. The restorative plan involved single-tooth implants in the maxilla and an implant-supported bridge in the mandible to replace the missing teeth. The implants were also to be used as anchors to intrude the mandibular right canine and first premolar. D–F, A diagnostic setup was constructed to determine the appropriate implant position prior to orthodontics. G, A placement guide was constructed from the setup so the surgeon could (H) guide the placement of the implants. I, After orthodontics, the same implants that were used as orthodontic anchors were used to restore the missing teeth.
A diagnostic wax setup is also necessary for patients who have unusual combinations of missing teeth and in whom the orthodontist is planning to substitute one tooth for another. For example, if a patient were missing maxillary lateral incisors and the orthodontist were planning canine substitution, a diagnostic wax setup would be mandatory to determine whether the occlusion will fit properly and if the teeth can be shaped accordingly. Occasionally a patient is missing a central incisor6 and a treatment option could be to restore the opposite lateral incisor as a central incisor in order to avoid an implant or fixed bridge (Fig. 26-6). A diagnostic wax setup would be necessary to determine whether the tooth arrangement will be both esthetic and functional.
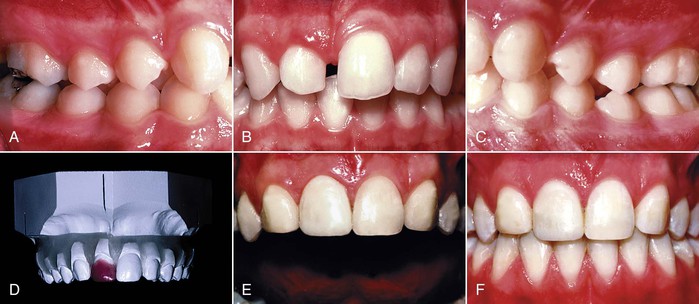
Figure 26-6 A–C, A 14-year-old female lost her maxillary right central incisor in a horseback riding accident as a child. No treatment was done at the time and the edentulous space had closed partially. She had a bilateral Class II malocclusion, no crowding in either dental arch, and a good facial profile. Although various treatment options were considered initially, the final plan involved extraction of the left lateral incisor, restoration of the right lateral as a central incisor, and bilateral canine substitution. D, A diagnostic wax setup was necessary to confirm that the treatment plan would satisfy the objectives. The setup helped the orthodontist to achieve an excellent (E) esthetic and (F) occlusal result.
Finally, adult malocclusions with significant mandibular incisor crowding occasionally are treated with extraction of a single mandibular incisor.7 This type of extraction improves long-term stability, easily eliminates the crowding, simplifies the mechanics, preserves facial esthetics, and improves periodontal health in certain adults. However, before extracting the incisor the orthodontist must know whether the occlusion will fit properly, especially in the canine and incisor region (Fig. 26-7). A diagnostic wax setup will give the clinician the appropriate information to make the correct decision when planning incisor extraction in crowded adult malocclusions.
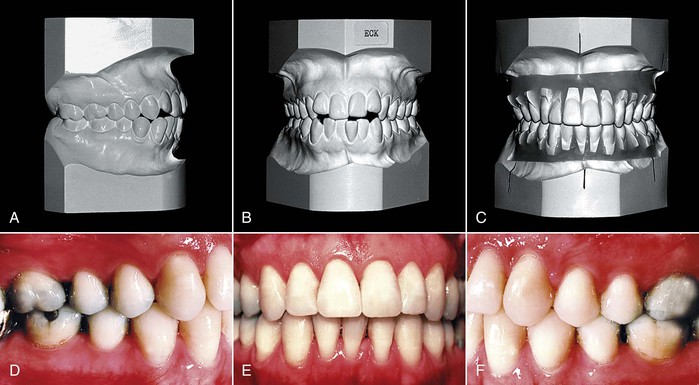
Figure 26-7 A 32-year-old female had (A) a bilateral Class I occlusion with (B) mild crowding of the maxillary teeth and moderate crowding of the mandibular incisors. C, A diagnostic setup was constructed to determine whether extraction of a mandibular incisor would eliminate the crowding and permit satisfactory overbite and overjet. D–F, The setup was invaluable in creating the vision and allowing the orthodontist to achieve a well-interdigitated occlusal result.
Establish the Sequence of Treatment
Many orthodontic-restorative patients also require adjunctive periodontal therapy and orthognathic surgery. As the number of dentists involved in a patient’s treatment increases, the complexity of the treatment also increases. In many of these situations, different specialists must interact at varying intervals during the patient’s overall treatment. Therefore the team of specialists not only must establish a realistic plan of treatment, but also should determine the sequence of interaction between the different specialists (Fig. 26-8).
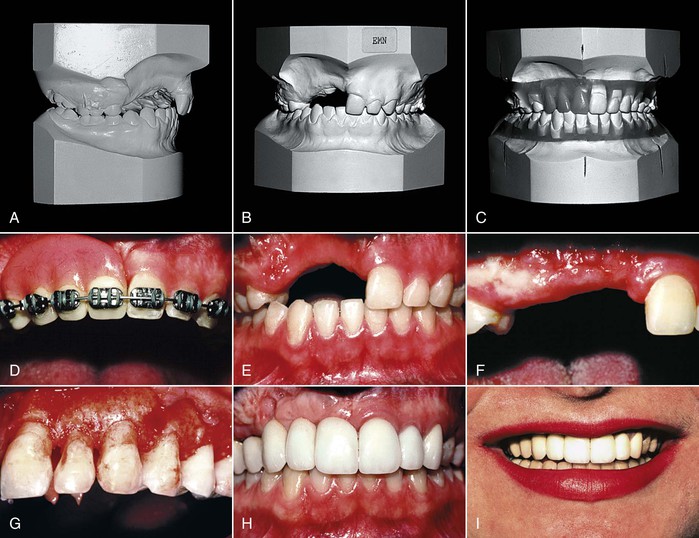
Figure 26-8 A and B, A 14-year-old female lost her maxillary anterior teeth in a water skiing accident, which left a huge void in the maxillary alveolus. C, A diagnostic setup was constructed to create the vision for the practitioners and patient. Several treatment options were discussed but the final plan involved (D and E) orthodontics, segmental maxillary jaw surgery, sagittal split ramus osteotomy, (F) autogenous soft tissue ridge grafting, (G) crown lengthening, provisionalization, and (H and I) final restoration. Because of the complexity of the treatment plan, the four practitioners on the patient’s team established the sequence of treatment before beginning therapy. Having the flow chart or treatment sequence facilitated the smooth treatment of this complicated case by keeping all practitioners aware of the timing of each step along the way.
This critical step is often overlooked. It requires that the team members meet to discuss the patient’s treatment before the initiation of therapy. After the sequence of intervention has been determined, it should be recorded by one of the clinicians.1 A copy of the treatment sequence should be given to each of the participating dentists and to the patient. Then, at any time during treatment, any of the team members can review the sequence, determine his or her point of interaction, and feel secure that the plan is proceeding properly. In addition, the patient is aware of the pathway toward completing treatment. The importance of this step in interdisciplinary treatment cannot be overemphasized. Success in treating a patient with complex restorative, periodontal, orthognathic, and orthodontic problems is dependent on not only the correct plan of treatment, but also the correct sequence of interaction among different practitioners during the course of treatment.
Identify Who Will Correct the Periodontal Defects
Many adult orthodontic patients have underlying periodontal defects that will need to be resolved before, during, or after the orthodontic therapy. It is mandatory that the orthodontist and periodontist discuss the management of these patients to determine who will be responsible for correcting the periodontal problems.8 These problems are generally divided into two categories: soft tissue or gingival discrepancies and hard tissue or bony defects. Gingival discrepancies include recession, lack of attached gingiva, and open gingival embrasures. Bony alveolar defects include interproximal craters; one-, two-, and three-wall defects; furcation defects; and generalized or localized horizontal bone loss secondary to periodontal disease. Each of these defects must be discussed prior to the initiation of orthodontic bracketing to determine who will be responsible for correcting them.
Gingival recession and inadequate attached gingiva often will require the placement of a connective tissue graft. In some cases it is best to perform the grafting prior to orthodontic treatment. This is especially important when the adult patient has preexisting recession and dental crowding and will be treated without the extraction of teeth.3 If there is a dehiscence labial to the tooth and recession has already occurred, it could get worse during orthodontic treatment. Therefore the periodontist will probably place a connective tissue graft prior to the orthodontic therapy to ensure that the recession will not progress and to cover the exposed root with gingiva.
Open gingival embrasures often occur during orthodontic therapy. If not corrected, these dark spaces between the teeth create an esthetic compromise after orthodontic therapy. The presence of a space above the central incisor interproximal contact may be caused by one of three factors.9 The first possible cause is diverging roots of the maxillary central incisors. This is usually the result of improper bracket placement (Fig. 26-9). In patients with overlapping and abraded maxillary central incisors, brackets may be placed inadvertently at an angle that is not perpendicular to the long axis of the central incisor. As the teeth are aligned, the roots may diverge distally. To identify this cause the clinician should evaluate a periapical radiograph. If the roots diverge, the brackets should be removed and repositioned with the bracket slots perpendicular to the long axes of the roots. As the roots align, the interproximal contact lengthens and moves apically toward the papilla. Usually the distal-incisal corners of the centrals also move apically. This reflects the amount of incisal wear that may have occurred before orthodontic treatment. These teeth usually require an incisal restoration to restore proper incisal contour.
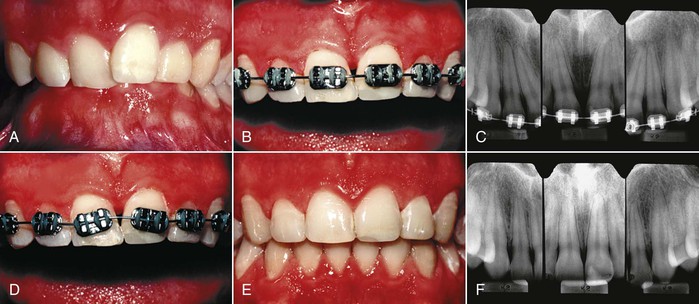
Figure 26-9 A, A young adult male had a Class II deep overbite malocclusion with mild crowding in both arches. B, During alignment of his overlapped maxillary incisors, an open embrasure developed between the maxillary central incisors. C, Progress periapical radiographs showed that the central incisor roots were diverted distally, causing the open embrasure. D, Therefore the teeth were rebracketed with the bracket slot perpendicular to the long axis of the roots. E and F, This permitted uprighting of the central incisor roots, which moved the contact gingivally and the papilla incisally to close the open embrasure.
A second possible cause of space above the interproximal contact of the central incisors is abnormal tooth shape.9 In some patients the crowns of the central incisors are much wider at the incisal edges than at the cervical region (Fig. 26-10). In these situations the contact between the incisors is located in the incisal 1-mm between the two centrals. This is an unusual contact relationship, as the contact should occupy about half the distance between the gingival margin and the incisal edge. One method of correcting this problem is to recontour the mesial surfaces of the central incisors and close the space (see Fig. 26-10). The other method is to restore the contact with either a composite or a porcelain laminate restoration. If recontouring of the tooth will make it too narrow, then restoration is appropriate. In all other cases, recontouring of the teeth and space closure is the easiest way to correct the open embrasure. The amount of enamel that must be removed from each tooth is equal to half the distance between the mesial surfaces of the incisors at the level of the tip of the papilla. Usually this will be about 0.5- to 0.75-mm and does not penetrate into the dentin. After this diastema has been created, the space between the teeth is consolidated. As this occurs, the contact lengthens and moves toward the papilla.
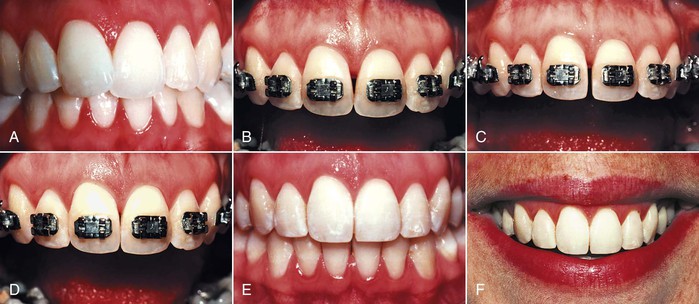
Figure 26-10 A, A 28-year-old female had a mildly crowded Class I malocclusion. Four premolars were extracted early in her life but no orthodontic treatment was performed. The objectives were to align the teeth and reduce the overbite. B, During alignment an open embrasure developed between the central incisors. The papilla height was normal but the contact between the centrals was too low, due to the triangular shape of the maxillary central incisors. C, The mesial surfaces of both centrals were reshaped with a diamond disc and (D) the space was closed, moving the contact gingivally toward the normal papilla. E and F, After orthodontics, the open embrasure had been eliminated and the occlusion and esthetics were satisfactory.
In patients with advanced generalized or localized periodontal disease and destruction of the crestal bone between anterior teeth, the papilla may be absent. This produces an unesthetic large gap after orthodontics. Several methods may be needed to resolve this problem (Fig. 26-11). In some cases reshaping the adjacent teeth, altering the root angulation, eruption of the adjacent teeth, and restoration will be necessary to move the bone coronally and to squeeze the gingival tissue between the adjacent crowns to establish a papilla between adjacent teeth after orthodontic therapy.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



