Missing Maxillary Lateral Incisors
New Procedures and Indications for Optimal Space Closure
Marco Rosa, Bjørn U. Zachrisson
The maxillary lateral incisor is the second most common congenitally absent tooth. There are three treatment options to replace missing lateral incisors: canine substitution,1–8 a single-tooth implant,9–11 or a tooth-supported restoration.12
Available evidence indicates that proper orthodontic space closure is well accepted by patients, does not produce a major risk for temporomandibular joint disorder (TMD) problems, and from a periodontal standpoint is safer than prosthetic replacements.13–15
The advent of osseointegrated implants decreased the popularity of the space closure alternative among many orthodontists and referring dentists and the implant substitution became their first option. Although it may appear preferable from an esthetic and functional point of view to create space to replace the missing lateral incisor with a single-tooth implant crown, recent studies have demonstrated that frequent biological complications may occur in the long-term.16–28 Such problems may include blue coloring of the marginal gingiva following labial bone resorption,19 peri-implantitis,18 bone loss around neighboring teeth,20 abutment exposure due to retraction of the labial gingiva,28 and progressive infraocclusion.20 Infraposition of the clinical crown may occur even when the implant has been placed in a mature adult, due to continuous eruption of the adjacent teeth (Fig. 25-1).21,23–26,29–31 The cessation and degree of vertical growth is unpredictable.21,23–27,30,31 Even if some evidence exists to help define the “end of growth” period, at present the individual variation is high and it is not possible to predict when unforeseen changes will appear.29 This could itself contraindicate the single-tooth implant restoration in the esthetic zone of patients who show the gingival margins when smiling.
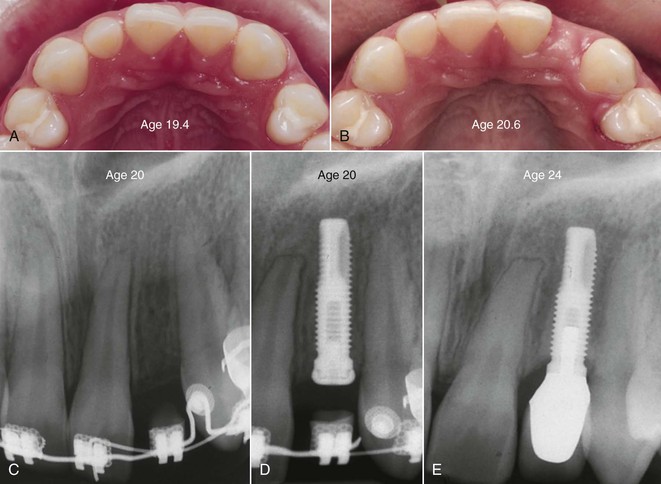
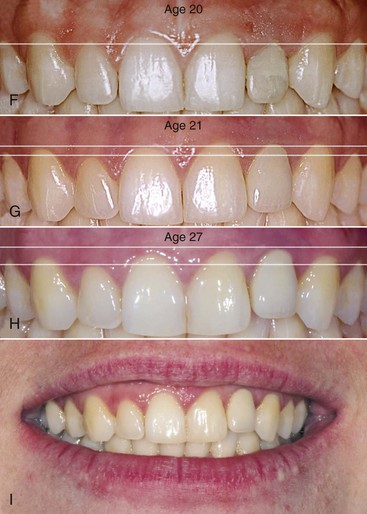
Figure 25-1 Infraocclusion of an implant crown placed at the “end of growth.” A and B, An adequate implant site was orthodontically opened in a 19-year-old woman. C and D, The osseointegrated implant was inserted during orthodontic treatment and a temporary resin restoration was cemented 1 month after the end of orthodontic treatment when the patient was 20 years old. F, The periodontal tissues were leveled similarly to the contralateral natural tooth. Due to continued eruption of adjacent teeth, (G) the gingival margin of the porcelain crown was already 2- to 3-mm higher than the implant restoration after 1 year and (E) uneven bone peaks were evident after 4 years. H and I, After 7 years the clinical situation was even worse. There is no reason to believe that this situation will remain stable. (The treatment was performed by the same team of professionals, in the same years and using similar procedures and implants, as the case shown in Fig. 25-18. It is impossible to explain why in this case an evident amount of infraocclusion occurred while in the case shown in Fig. 25-18 it did not.) (Periodontist: Dr. Francesca Manfrini; Prosthodontist: Dr. Giovanni Manfrini, Riva del Garda, Italy; Ceramist: Antonio Bertoni, Brescia, Italy.)
Another drawback of the space reopening alternative for a teenage patient is that several years must elapse between completion of orthodontic treatment and implant placement. After successful orthodontic opening of the implant space, the central incisor and canine roots may reapproximate during retention and prevent implant placement. Olsen and Kokich32 have reported that retreatment and orthodontic space reopening was needed in 11% of their patients. At this stage of treatment, related problems and questions arise, such as:
• What is the optimal retention device?
• Will a temporary resin-bonded bridge be esthetically acceptable?
• How long must we wait to place the implants?
In contrast, the canine substitution option has the indisputable advantage that the entire treatment is accomplished in one phase and the result is permanent and independent of residual maxillary growth.2–8 This point is particularly important since the majority of patients with missing maxillary lateral incisors are diagnosed at an early age.
It has to be stated, however, that even if space closure treatment results are well accepted by the patient and parents and acceptable from a functional standpoint,13,14 the simple substitution of the missing lateral incisor with the canine is not sufficient for today’s high esthetic standards. The reasons for this are several:
• The gingival margins frequently became unnatural. The borders are too high apically on canines moved to replace the lateral incisors and too short on the first premolars moved in the place of the canines (Fig. 25-2).

Figure 25-2 Long-term appearance after space closure. A, Twenty-five years after orthodontic space closure the result is stable and the periodontal tissues are healthy, although the esthetic result is not ideal and the smile is not natural. B, The gingival margins are not natural. They are too high on the canines, which were moved in place of the lateral incisors, and too short on the first premolar, which was moved to replace the canines.
Over the last decade, new clinical procedures have been proposed to improve the esthetic and occlusal outcome for canine substitution treatment by combining carefully detailed orthodontic finishing with techniques used in esthetic dentistry.5–8 Together, these procedures are able to provide the improvements needed to approach the appearance of a natural intact dentition, both functionally and esthetically, and provide predictable final results that are stable in the long-term (Figs. 25-3 and 25-4). It is the authors’ opinion that this will make orthodontic space closure a more attractive treatment alternative than before.
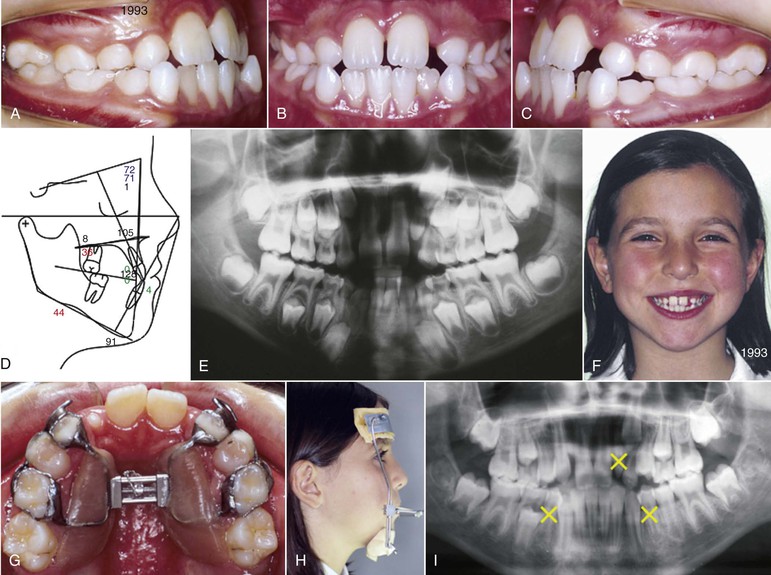
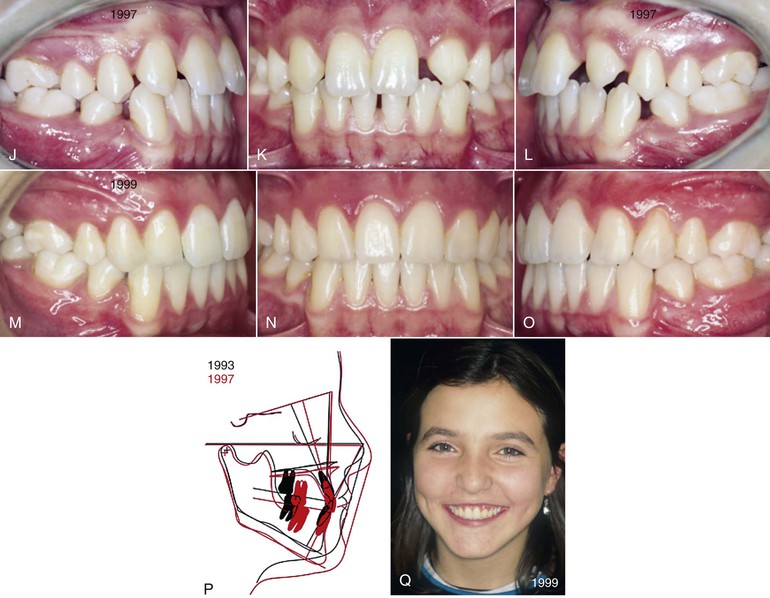

Figure 25-3 Long-term stability of space closure and gingival remodeling. A–F, An 8-year-old girl with hyperdivergent Class III malocclusion, narrow maxilla, lower crowding, and unilateral missing upper right lateral incisor in the early mixed dentition. Early orthopedic treatment included (G) rapid maxillary expansion (RME) and (H) maxillary protraction using deciduous teeth as anchors. Following (I) serial extraction of the upper left peg-shaped lateral incisor and the lower first premolar, (J–L) the upper left canine erupted in the lateral incisor’s site and simplified the second phase of treatment with fixed appliances. The fixed appliance stage lasted 11 months and effectively closed the spaces with a good occlusion (M–P). On the same day that debonding occurred, the upper canines were ground and restored with composite resin to close the “black triangles” and the first premolars were built up to resemble and function as canines. Q, The patient showed gingival margins when smiling and the overall exposure of teeth and periodontal tissues was in good balance. Twelve years after the end of treatment the patient was 27 years old. R–V, The occlusion is stable and (W) the overall esthetics remains satisfactory. Minimal maintenance of the composite buildups was needed, although substitution with porcelain veneers would increase the esthetic outcome and improve the long-term prognosis. (Composite buildups: Dr. Patrizia Lucchi, Trento, Italy.)
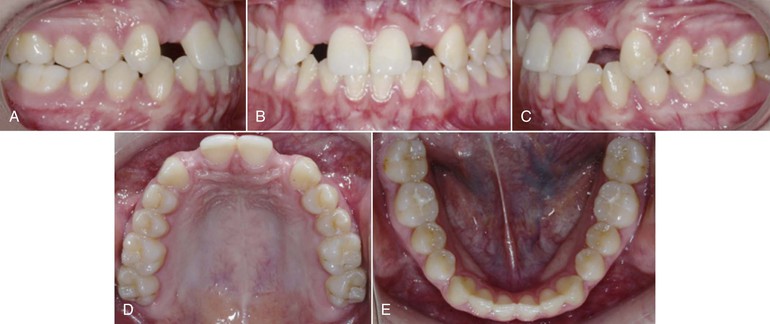

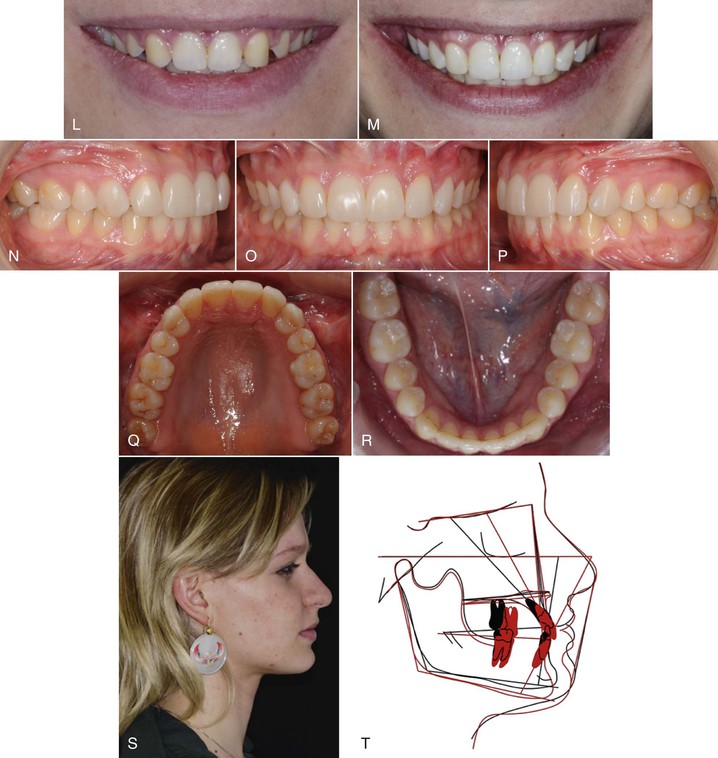
Figure 25-4 Space closure and facial surgery after unsatisfactory space reopening. A–H, In a previous treatment performed elsewhere, spaces were reopened for implant substitution in a 17-year-old female. The occlusion appears normal and maxillary lateral incisor spaces were prepared bilaterally for implants. Because of the Class III tendency with retruded maxilla, the upper incisors were protruded in an attempt to correct the overjet and improve the profile. The lateral incisors were temporarily replaced with a removable plate. I–K, The revised treatment plan included closure of all spaces in the maxilla. Uprighting of the maxillary incisors produced an anterior crossbite. J, Note that the soft tissue profile after the 7 mm incisor retraction didn’t change significantly when compared to the initial profile. The overjet was corrected surgically together with the skeletal discrepancy. L, The first premolars were intruded to achieve ideal levels of the gingival margins. L and M, On the day that debonding occurred, temporary composite direct restorations were made on the six front teeth. M–Q, Five years postop, the direct composite build-ups were substituted with resin veneers. M, The incisor display while smiling is ideal for a young adult woman. N–P, Final results show maxillary molars in Class II relationship. R, Retention consisted of one bonded six-unit retainer in the lower arch. The profile (S) improved significantly due to (T) the surgical vertical/sagittal maxillary repositioning and the concomitant mandibular rotation. T, Surgery involved just the maxilla, which was moved forward and down to increase the overall vertical dimension. The superimposition in T also shows that the upper lip did not move forward. (Surgeon: Dr. Mirco Raffaini, Parma, Italy; Composite restorations and veneers: Dr. Patrizia Lucchi, Trento, Italy.)
The goal of this chapter is to:
1. Describe the method for optimal space closure.
2. Define priorities in treatment planning.
3. Suggest new indications and contraindications for the space closure alternative.
4. Recognize and address the most frequent hidden problems.
Clinical Method for Optimal Space Closure
When the goal is the appearance of a naturally intact dentition, both functionally and esthetically, the patient needs a long, sometimes difficult two-phase interdisciplinary treatment approach.
Orthodontic Treatment
The overall goal of orthodontic treatment is not only space closure while correcting the malocclusion, but also proper finishing in the esthetic zone to create a well-balanced exposure of the upper front teeth, allowing the restorative dentist to perform minimally invasive, ideal restorations.
The specific goals of the orthodontic finishing phase are:
• Class I or Class II molar occlusal relationship (depending on the need for extractions in the lower arch) (see Figs. 25-3 and 25-4; Figs. 25-5 to 25-7).
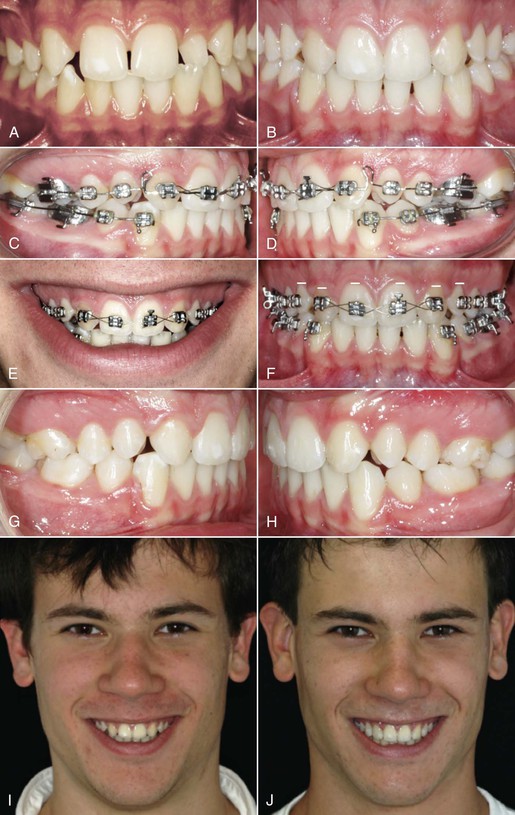
Figure 25-5 Space closure with lower premolar extractions. A, A 13-year-old boy with unilateral agenesis. Peg-shaped left lateral incisor and lower first premolars were extracted. C–F, Treatment lasted 22 months and (B and E–I) included gingival leveling by extrusion of the canines and intrusion of the first premolars. J, Composite resin buildups on six teeth included elongation of the central incisors to produce a nice smile arc. (Composite restorations: Dr. Patrizia Lucchi, Trento, Italy.)


Figure 25-6 Long-term stability of space closure and gingival remodeling. A–C, An 11-year-old girl presented with Class II, subdivision and a missing maxillary lateral incisor. The small left lateral incisor was extracted. The lower arch was treated with minor stripping to flatten the curve of Spee and solve the 2-mm crowding. D–F, Upper space closure was performed with maximum anchorage on the upper central incisors, extrusion of the canines, and intrusion of the first premolars to create a natural-looking gingival profile. At the end of active treatment (25 months), the patient was 14 years old. G–I, The result was satisfactory: good intercuspation with Class II molar relationship and natural-looking front teeth, mainly due to the “big” canines. Resin buildups were made directly on the canines and first premolars. J–M, Twelve years after treatment, cone beam computed tomography (CBCT) shows the adequate tissues were achieved by the palatal root torque of the canines during their extrusion and the labial root torque/palatal crown tip of the premolars during their intrusion. The occlusion is stable and the periodontal tissues are healthy. N–P, Twelve years after treatment, there is no bleeding on probing and probing depth (PD) is within the normal range. Q and S, Ten years postop and despite the satisfactory occlusal result and periodontal stability, the overall esthetics of the smile was not ideal due to the small teeth, especially the central incisors. R and T, After buildups on the central incisors and canines, the macroesthetic elements of the smile were improved. (Buildups: Dr. Patrizia Lucchi, Trento, Italy.)
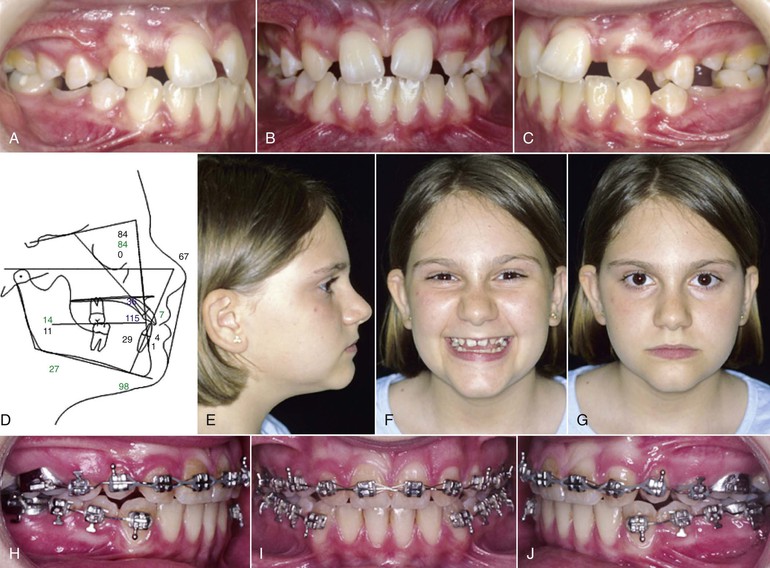

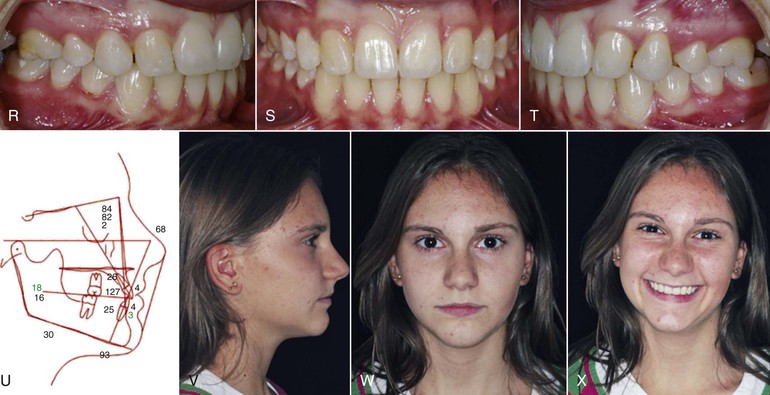
Figure 25-7 Space closure in Class III malocclusion with narrow maxilla and spaced upper arch. A–G and M, A 12-year-old girl presented with bilateral maxillary lateral incisor agenesis, Class III malocclusion, narrow maxillary arch, and pronounced spacing. Because of optimal motivation of and cooperation by the patient, the treatment plan was to close all spaces. H–J, After rapid maxillary expansion (RME), fixed appliances were used for space closure to obtain good intercuspation of the second premolars with Class II molar occlusion. Canine extrusion and first premolar intrusion, as well as torque control of anterior and posterior teeth, was achieved by archwire bending. As shown in K and L, the maxillary anterior teeth may need further elongation to improve their relationship to the lips. N, Note the detailed alignment on rectangular stainless steel archwires, with mesial and distal offset bends for the canines in lateral incisor position and distal offsets for the first premolars in canine position. At the end of treatment (R–T) the occlusion was good and (O) a fixed retainer was bonded on four teeth. The (V) profile and (W and X) frontal facial appearance improved significantly due to the mandibular posterior rotation, which increased the vertical dimension. The selective extrusion and intrusion of the canines and first premolars, respectively, leveled the gingival margins to (R–T) a natural high-low-high relationship. The composite resin buildups were made on the day of debonding for esthetic reasons and to stabilize the occlusion. The canines in lateral incisor position were not ground and shortened. P and Q, The clinical crown length of the central incisors was increased with the buildups to an improved proportion compared to the new lateral incisors and (Q and X) to provide a good smile arc. Q and X, After the cosmetic phase with composite resin buildups on all six front teeth and whitening (vital bleaching) of the canines, a balanced and naturally looking appearance was achieved. The smile is pleasant not because of the new lateral incisors but because of the restored first premolars in canine position and central incisors. (Composite resin buildups: Dr. Patrizia Lucchi, Trento, Italy.)
• Alignment of the incisal edges of the central incisors with the cusps of the canines and the buccal cusps of the restored first premolars (“new” canines) (see Fig. 25-7, N; Figs. 25-8 and 25-9).
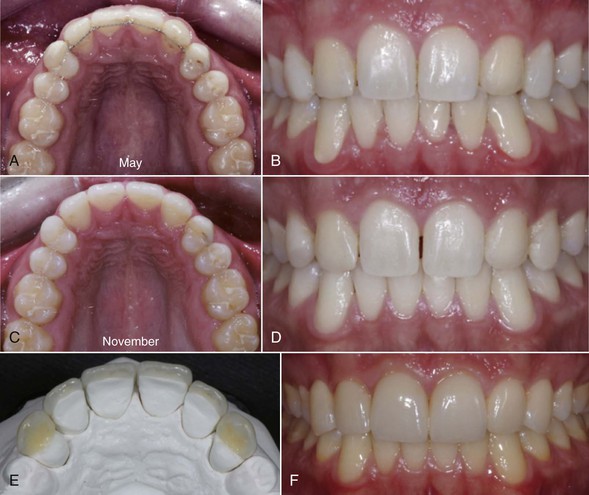

Figure 25-8 Porcelain laminate veneers (PLV) and long-term stability. A–D, At least 10 months before the PLV are made, the upper bonded retainer must be removed, which will allow small spaces to reopen. During this time the patient should not use any removable retainer in the upper arch. Selective grinding may become necessary to stabilize the occlusion. E and F, When the occlusion and the small spaces are stable, the PLV are made and will close the spaces. G–J, Two years after the porcelain restorations, the result was stable and no spaces were noticeable among the upper front teeth. The porcelain veneers will also optimize the functional occlusion. In the absence of a lingually bonded retainer, group function may be better than a cuspid protected occlusion to ensure long-term stability. G to J show simultaneous contacts on the second, third, and fourth tooth (blue marks in H and I). (Prosthodontist: Dr. G. Manfrini, Riva d G, Italy. Ceramist: A. Berto.)
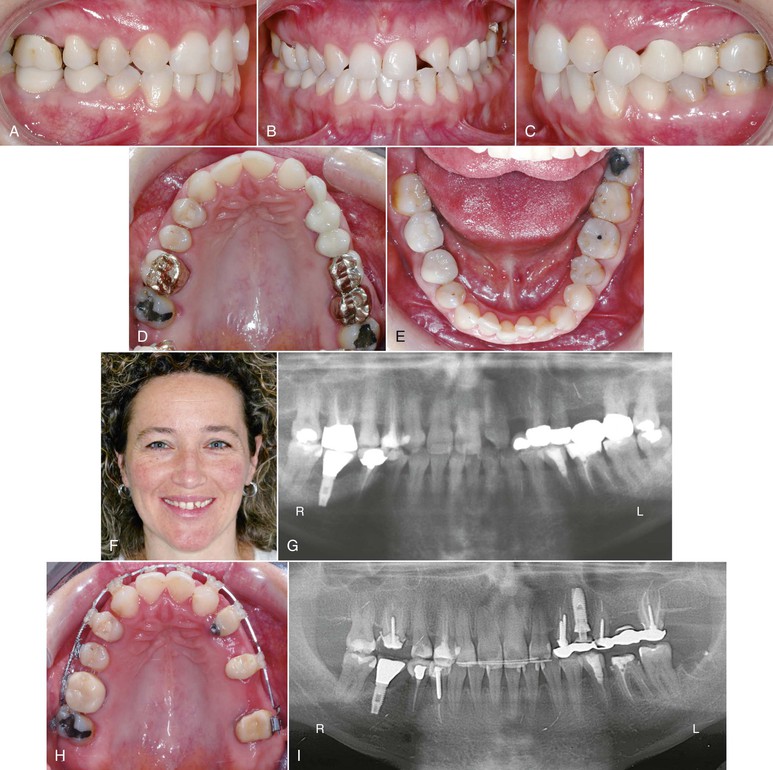


Figure 25-9 A–G, A 37-year-old female patient with bilateral agenesis of the maxillary lateral incisors and severe asymmetry of the upper small-sized front teeth. A 5-unit bridge restoration replacing the upper left first molar and a small canine (cantilever) is evident in the upper left arch. The treatment plan was to close the spaces in the smile area and correct the upper midline while reopening a space (implant site) between the upper left premolars. During treatment, adequate diastemas were opened mesially and distally on the central incisors to allow resin buildups on those teeth. I, An implant was inserted into the orthodontically regenerated alveolar bone during orthodontic treatment. J–L, The canines were extruded and the first premolars in canine position were intruded. D and H, The maxillary arch form was corrected and the symmetry was reestablished. M, A 3-mm overjet was left intentionally after the orthodontic treatment, to be filled by restorations of the small central incisors: (N) two different porcelain veneers in the palatal and buccal side. O–Q, Four years post-treatment, with porcelain restorations on the implant and on the six upper front teeth, the result was stable. T–W, The anterior occlusal guidance is a group function and was ideal after the restoration of upper central incisors. O–W, With no retention in the upper arch, the upper space closure remained stable with no reopening of the spaces. X, The overall smile is better than what could have been possible with two restorations replacing the missing laterals because of the ideal size of the central incisors, which are in good balance with the face. The long-term prognosis is more predictable because of the presence of natural roots instead of foreign bodies. (Prosthodontist: Giovanni Manfrini, Riva del Garda, Italy; Ceramist: Antonio Bertoni; Brescia, Italy.)
• Ideal frontal exposure. Compared to the lateral incisor width, the central incisors should be about 160% and the canines 70%.33
• Leveling with torque control of the upper six front teeth to achieve natural “high-low-high” gingival margins. The new canines (i.e., the first premolars) are at the same level as the central incisors and the new lateral incisors (i.e., the canines) are at a lower level (see Fig. 23-6). Such adjustments can be made using archwire bends or, more easily, by bonding the canine brackets higher than normal and the first premolar brackets in an incisal position.5–8 The gingival leveling is particularly important in patients who show much gingiva when smiling.
Restorations
The goals of the restoration phase for canines and first premolars (and possibly central incisors) are:
Six-Step Clinical Procedure (Box 25-1)
Step 1: Space Closure and Correction of the Malocclusion
The extraction of two premolars in the mandibular arch is sometimes necessary, depending on the extent of lower arch crowding, incisor protrusion, lip posture, and expected growth pattern. Typically, a normal mandibular arch form should not be expanded and should maintain the pre-treatment shape. The maxillary archwires should be coordinated with the lower ones.
The space closure in the upper arch may be performed without major problems in crowded cases and in Class II malocclusions. If the diagnosis is made in the early mixed dentition, a serial extraction strategy may sometimes be effective to shorten the treatment time stage with fixed appliances (see Fig. 25-3).
The problems become more relevant when treatment must be achieved with maximum anterior anchorage. In such cases, conventional biomechanics (Fig. 25-10, A and B) are usually sufficient to close the spaces.3 However, moving each tooth individually is time consuming and the patient’s compliance with intermaxillary elastics is essential to achieve the treatment goal in a reasonable time span. Usually space closure is made with a heat-treated 0.016-inch × 0.022-inch stainless steel archwire, using brackets of different slot sizes: 0.018-inch on the central incisors and canines and 0.022-inch on the premolars and molars.
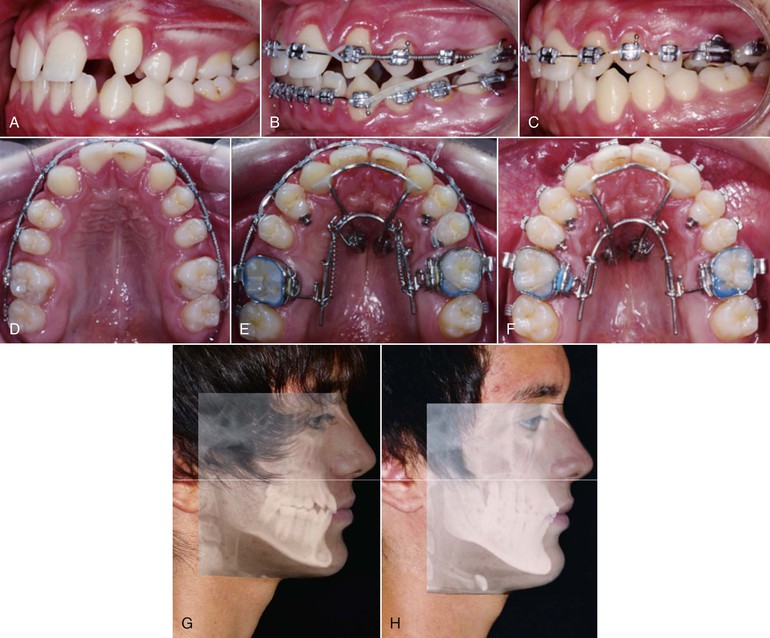
Figure 25-10 Noncompliance space closure. A, A 15-year-old boy presented with missing maxillary lateral incisors. The lower arch was not crowded and the lower incisors were well positioned on the A-Pogonion line. B, The upper space closure was difficult due to poor cooperation in wearing Class III elastics. Two mini-screws were inserted in the palatal vault at the level of the first premolars. C, Appliances were removed in the lower arch and (D–F) a sliding structure, which acted as absolute anchorage in supporting the mesial movement of the premolars and molars with pulling springs for 14 months, was tied to the mini-screws. G and H, It was possible to move the whole posterior dentition in the upper arch mesially while maintaining a good interincisal angle and lip posture and profile.
With recent technical advances, including absolute skeletal anchorage with two connected palatally inserted mini-screws,34–38 maximum anchorage problems can be overcome and all posterior teeth can be moved simultaneously forward without compliance problems. This system allows mesial movement of molars and premolars with no extra anchorage and/or Class III elastics39 (Fig. 25-10, C-H).
The mesial movement of the first premolar may be complicated in the presence of two divergent roots. It may be indicated to slightly rotate such premolars to prevent the buccal root from moving into the cortical plate, which would slow down the movement and potentially produce a risk for periodontal tissue breakdown.
Furthermore, the curve of Spee should be flattened to allow proper orthodontic finishing. Fixed appliances are necessary in the mandibular arch, at least in the final stages of treatment. A correct cusp to fossa relationship should be achieved on the upper second premolars, together with a solid stable occlusion with no notable CO-CR discrepancy. Sometimes slight selective grindings are necessary.
Another possible alternative treatment plan for agenesis patients who show much gingiva when smiling is to close the spaces anteriorly and open up space for a third premolar in the posterior areas (see Fig. 25-9; Fig. 25-11).

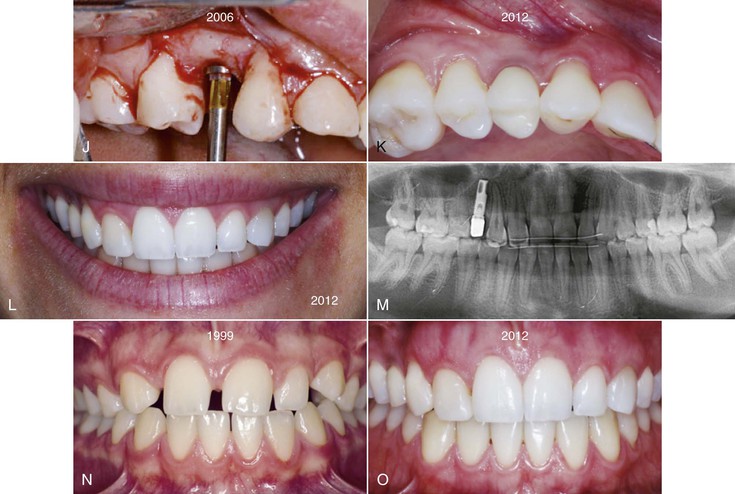
Figure 25-11 Atrophy of the orthodontically regenerated alveolar bone in the interim between orthodontic treatment and the implant, after unilateral space closure and space reopening in the back. A, C, F, and N, A 13-year-old girl presented with a gummy smile and unilaterally missing upper right lateral incisor. B, D, E, and G, She was treated with space closure while a space was reopened between the premolars. At the end of the orthodontic treatment, the implant site was adequate in (E) width, (G) height, and (B and H) thickness. Since the patient was then 15 years old, the final restoration was delayed until the “end of growth” and a lingual retainer was bonded on the six upper front teeth. Placement of an osseointegrated implant was planned for when the patient was 21 years old. I, During the 6-year interim the thickness of the alveolar crest decreased due to bone atrophy (arrow). J, The implant was placed at age 21 years. K, L, M, and O, Six years after the implant restoration, further bone loss and bluish gingival discoloration was evident. The composite buildups on the right premolar and canine were substituted with porcelain restorations. L and O, The upper right lateral incisor (the canine) looked healthy, with the gingival margin at the same level as the left lateral incisor. L, The loss of periodontal tissue thickness was evident in the buccal side of the implant area and created a severe esthetic impairment in this “gummy smile” woman, who was not satisfied with the final result after a very long and expensive treatment. The long-term prognosis is uncertain and it is not possible to exclude the necessity of maintenance, adjustments, periodontal procedures, or possible remaking of the implant crown. (Periodontist: Dr. Francesca Manfrini, Riva del Garda, Italy; Prosthodontist: Dr. Giovanni Manfrini, Riva del Garda, Italy; Ceramist: Mr. Antonio Bertoni, Brescia, Italy.)
Step 2: Orthodontic Finishing in the Maxillary Anterior Region
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


