CHAPTER 25 Considerations for the Use of Dental Implants With Removable Partial Dentures
This chapter presents basic considerations in the selection of implants to improve prosthesis performance by increasing functional stability. Prosthesis instability, a commonly stated problem with removable prostheses, is presented as a potentially confounding and unique component of oral sensory-motor function at issue when patients are challenged with removable prostheses. When all the relevant information necessary to adequately address how best to manage a patient’s tooth loss is considered,* one aspect that should be kept in mind is that among the various prostheses from which we choose (conventional fixed partial denture, implant-supported partial denture, and removable partial denture), the removable partial denture is the most unique. Exactly how we describe this uniqueness to our patients is critical to their appropriate prosthesis selection and provides a clue to us as to how dental implants can best be used in conjunction with removable partial dentures (RPDs).
Physiologic Distinction Between Prostheses
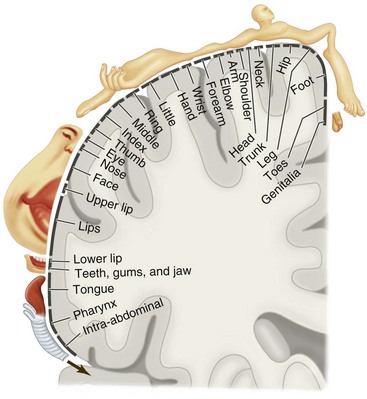
Given this support and rigid connection difference, it is easy to recognize that one distinguishing difference between fixed prostheses (tooth or implant supported) and tooth-tissue–supported RPDs is the potential for movement under function. The impact that such movement will have on related oral sensory and oral functional expectations of patients is potentially critical to understand. These patient-specific perspectives are variable because some of our patients are better at distinguishing oral sensory input than others and some are more functionally capable than others. The importance of sensory-functional considerations is evident when it is realized that the oral cavity is unique from a sensory perception standpoint, because the sensory input from the mouth regions involved in the task of mastication represents one of the largest collections of sensory information processed for a single functional act in the body, rivaled closely by the multifunctional hand (Figure 25-1).
Replacing Anatomy and Functional Ability
With this relative importance of oral sensory function associated with mastication in mind, it would be helpful to consider what exactly we are attempting to replace when we discuss with our patients the management of missing teeth. This involves both the physical tools for mastication and the oral ability for precise and stable neuromuscular functions to manipulate a bolus of food. Analysis of chewing studies shows that the oral receptor feedback that guides movement of the mandible comes from various sources. The most sensitive input (i.e., the input that provides the most refined and precisely controlled movement) comes from the periodontal mechanoreceptors (PMRs), with additional input coming from the gingiva, mucosa, periosteum/bone, and temporomandibular joint (TMJ) complex. Loss of teeth leads to loss of guidance precision, which may be caused by the deficit in PMRs. No artificial replacements reestablish the same ability inherent in the PMR guidance. Yet prostheses may vary in their ability to affect the deficit on the basis of sensory-related dynamics. This notion of variable prosthesis impact suggests that either the prostheses are not the same or patients may vary in terms of neuromuscular* ability.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses