24
Anaesthetic emergencies in the wider hospital
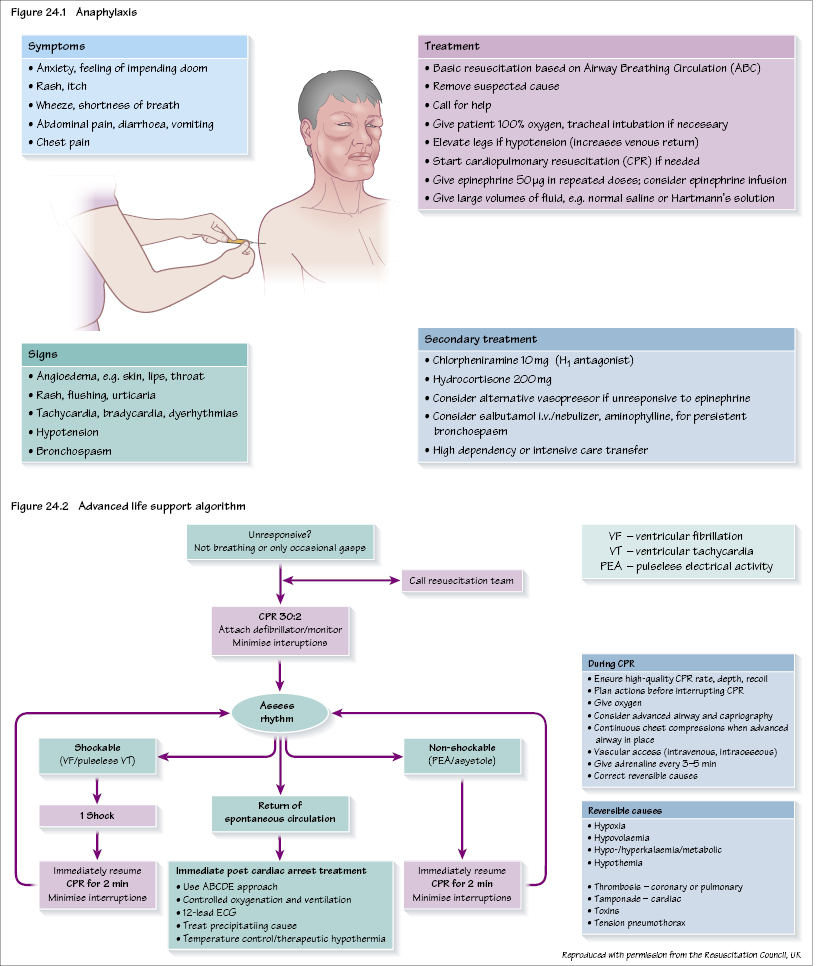
Anaphylaxis
This is an acute severe type 1 hypersensitivity reaction when an antigen (trigger) reacts with immunoglobulin IgE bound to histamine-rich mast cells and basophils. The clinical features are some or all of: oedema, rash, wheeze, shortness of breath and circulatory collapse (Figure 24.1). The incidence during anaesthesia is approximately 1/10 000–1/20 000. On allergen exposure (after previous exposure which will have sensitized the patient) there is a large IgE-mediated release of histamine, complement and other inflammatory mediators. Within anaesthesia the commonest causative agents are neuromuscular blocking agents (60%), latex (20%) and antibiotics (15%). Most reactions occur soon after administration but can be delayed by up to an hour. Although intravenous drugs are the commonest cause in anaesthesia, skin cleaning preparations (e.g. iodine or chlorhexidine) are also well-recognized causes.
Follow-up and investigation of suspected anaphylaxis is important. It should also be considered in unexpected perioperative critical incidents (e.g. unexplained perioperative cardiac arrest, unexplained hypotension or bronchospasm, widespread rash, angioedema).
Three blood samples should be taken for mast cell tryptase:
Later investigation includes referral to an allergy specialist, skin prick testing and intradermal testing (more sensitive but less specific). Specific IgE can be detected by using a metho/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


