22
Regional anaesthesia
Regional anaesthesia involves the injection of local anaesthetic (LA) and sometimes other drugs (e.g. opioids) targeted at a specific nerve(s) or nerve plexus to numb the area that the nerve innervates, including the spinal cord and its nerve roots. Indications for a nerve block include:
- sole form of anaesthesia during an operation;
- combined with general anaesthesia or sedation;
- postoperative analgesia;
- chronic pain conditions.
Central (neuraxial) blockade
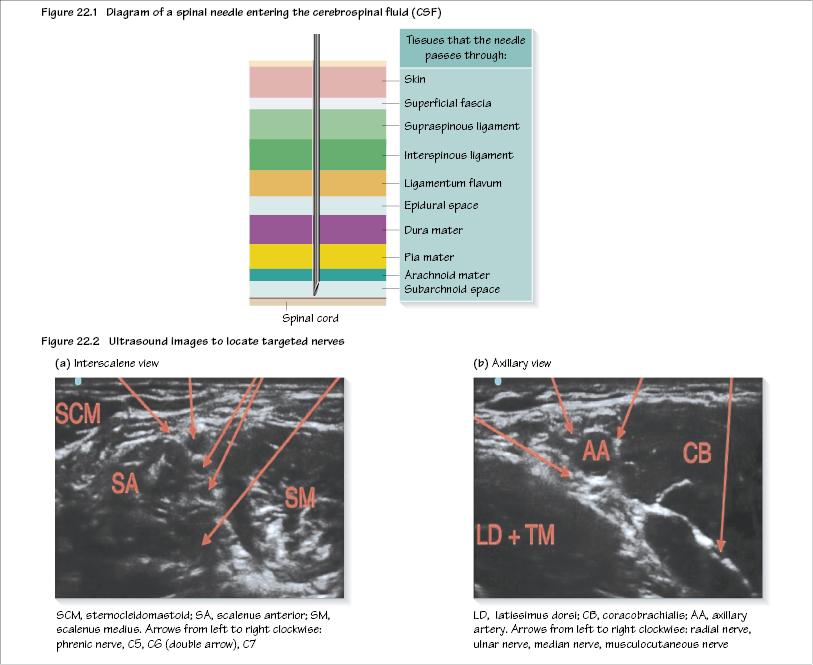
Central blockade is the introduction of drugs into the CSF within the subarachnoid space (spinal blockade; Figure 22.1) or the surrounding epidural space (epidural blockade). Anaesthesia is provided for surgery below the level of the umbilicus (T10).
Advantages of central blockade are:
- avoidance of GA in at-risk patients, e.g. severe respiratory disease, difficult intubation, diabetic, myopathies, pregnant, malignant hyperthermia;
- good postoperative analgesia;
- avoids sedation/nausea and vomiting, e.g. by morphine;
- reduction in pulmonary thromboembolism due to sympathetic block;
- reduced blood loss;
- reduced stress response to surgery.
Side effects of central blockade are:
- hypotension (sympathetic block);
- nausea and vomiting (hypotension, opiates);
- lower limb motor block;
- post dural puncture headache (more likely with large needle, non-pencil-point tip, inadvertent Tuohy needle puncture of dura, young age);
- high block can effect upper limb power and respiration (C3–5);
- loss of consciousness (total spinal);
- nerve damage (rare).
Contraindications to central blockade include patient refusal, no i.v. access, severe CVS disease, hypovolaemia, sepsis, LA allergy, coagulopathy (e.g. INR needs to be <1.5). Caution must be exercised if there has been previous major spinal surgery or ongoing CNS disease.
Spinal block
The spinal cord terminates at the lower border of L1 or upper border of L2. A spinal needle must be introduced at or below the L2/L3 interspace. Tuffier’s line is a useful landmark, that is a line drawn between the iliac crests corresponding to the level of L4/5.
Spinal needles are narrow gauged (25 or 27 G) so as to make as small a hole in the dura mater as possible. The most commonly used needle has a blunt ‘pencil-point tip’, which separates the dural fibres rather than cutting, reducing the incidence of CSF leak-related headache.
To perform a s/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


