CHAPTER 21
Maxillary Surgery
Christopher Choi,1 Brian B. Farrell,2 and Myron R. Tucker2
1Inland Empire Oral and Maxillofacial Surgeons, Rancho Cucamonga, California, USA
2Private Practice, Carolinas Center for Oral and Facial Surgery, Charlotte, North Carolina, Department of Oral and Maxillofacial Surgery, Louisiana State University Health Science Center, New Orleans, Louisiana, USA
Le Fort 1 Osteotomy (Single Piece)
A means of repositioning an intact maxilla to correct congenital and acquired dentofacial deformities.
Indications
- Correction of maxillary dentofacial deformities in all three planes of space
- Access to pathologic lesions located within the maxillary sinus, nasal cavity, and/or skull base
- Interpositional bone grafting for the atrophic, edentulous maxilla
Contraindications
- Surgery performed prior to the complete eruption of the maxillary permanent dentition
- Medical conditions prohibiting surgery
Surgical Anatomy
The vasculature supply of the maxilla is abundant and is supplied via the terminal branches of the maxillary (posterior superior alveolar, infraorbital, descending palatine, and sphenopalatine arteries), the ascending pharyngeal (branch of external carotid artery), and the ascending palatine (branch of facial artery) arteries via the soft palate.
The maxilla is composed of three vertical buttresses: the zygomaticomaxillary, nasomaxillary, and pterygomaxillary buttresses. The zygomaticomaxillary buttress laterally and the nasomaxillary buttress (piriform rim) medially form the periphery of the maxillary sinus and serve as areas for fixation after Le Fort procedures. The pterygoid plates comprise the pterygomaxillary buttress located just posterior to the maxilla.
The infraorbital nerve is the terminal branch of the second division (V2) of the trigeminal nerve. The infraorbital nerve supplies sensation to the lower eyelid, lateral aspect of nose, and upper lip and is encountered during subperiosteal elevation of the lateral wall of the maxilla.
Technique
- The patient is placed supine on the operating room table and nasally intubated. The anesthesia tube is secured, all extremities are padded, and a urinary catheter is placed for procedures exceeding 150 minutes. Lacrilube is placed within the orbits, and opsites are placed to protect the periorbital regions during the procedure. A throat pack is placed within the posterior oropharynx, and the oral cavity is prepped with betadine solution and/or chlorhexidine gluconate 0.12% oral rinse and a toothbrush to include all teeth, the gingiva, the tongue, and the palate. The maxillofacial skeleton is prepped with betadine scrub from the hairline to the clavicles, and the patient is draped in a sterile fashion to allow for exposure of and access to the oral cavity, nasal bridge, and orbits.
- Local anesthesia containing a vasoconstrictor is placed circumferentially within the maxillary vestibule. Additionally, the nasal floor, nasal septum, and inferior turbinates are injected to assist in hemostasis.
- A Kirschner wire may be inserted within the nasofrontal suture (Figure 21.1 [all figures cited in this section appear in Case Report 21.1, unless otherwise noted]) to establish a vertical reference for the maxilla. A Boley gauge is utilized to measure from the Kirschner wire to an anterior maxillary reference point (the anterior maxillary orthodontic arch wire, the orthodontic brackets of teeth #8 and #9, or the incisive edges of teeth #8 and 9), and the measurement is recorded.
- In select cases, enameloplasty is performed with a large diamond bur and copious irrigation on selected tooth surfaces that are determined preoperatively.
- A maxillary vestibular incision is initiated through mucosa from the maxillary premolar to the midline (Figure 21.2). The incision is positioned 10 mm cephalic to the mucogingival junction and parallels the mucogingival junction. A mucosal releasing incision may be incorporated at the first molars to allow for increased flap elevation. The incision is extended through subcutaneous tissue, muscle, and periosteum.
- A subperiosteal dissection exposes the lateral maxillary wall, the zygomaticomaxillary and nasomaxillary buttresses, and the piriform aperture (Figure 21.3). The identical incision and dissection is performed on the contralateral side.
- Sharp, subperiosteal dissection is used to enter the nasal cavity and to elevate the nasal mucosa from the piriform aperture. A periosteal elevator is used to elevate the nasal mucosa from the lateral nasal walls and the nasal floor. Careful elevation and reflection of the nasal mucosa will minimize nasal mucosal tears during downfracture of the maxilla.
- A retractor is placed posterior to the maxilla to expose the pterygomaxillary junction (the junction of the maxillary tuberosity and the pterygoid plates) and to reflect the overlying tissue. An elevator is placed along the lateral nasal wall of the nasal cavity within the submucosal plane to protect the nasal mucosa during the osteotomy (Figure 21.3).
- A reciprocating saw is utilized to create a horizontal osteotomy from a point just posterior to the maxillary tuberosity to a point just superior to the nasal floor (Figure 21.4). The osteotomy is placed superior to the apices of the maxillary teeth. The osteotomy is mirrored on the opposite side.
- A double guarded vomer osteotome is used to separate the nasal septum and vomer bone from the nasal crest of the maxilla (Figure 21.5).
- A curved pterygoid osteotome is used to divide the pterygomaxillary junction. The osteotome is placed between the maxillary tuberosity and the pterygoid plates and is directed medially and inferiorly, away from the pterygoid plexus and internal maxillary artery (Figure 21.6). A finger can be placed on the palate at the hamular notch region to palpate the separation.
- A single guarded osteotome is used to separate the lateral nasal wall (Figure 21.7). A change in sound is audible posteriorly as the thicker, perpendicular plate of the palatine bone is engaged. Partial sectioning of the palatine bone minimizes unfavorable fracture patterns during downfracture, which may cause disruption of the orbits and/or cranial base.
- After the completion of all maxillary osteotomies, the downfracture of the maxilla is performed with digital pressure. Tessier mobilizers are placed posterior to the maxillary tuberosities (Figure 21.8) in order to distract the maxilla forward and laterally to complete the bony separation and to stretch the posterior soft tissue pedicle. The maxilla should be capable of mobilization of 1.5 cm in all directions.
- The greater palatine arteries should be identified and preserved or ligated (surgeon’s preference).
- Interferences within the areas of the nasal crest of the maxilla, the lateral nasal wall, and the posterior and lateral aspects of the maxillary sinus are removed (Figure 21.9).
- The anterior nasal spine may be reduced, especially in cases of maxillary advancement and superior repositioning.
- The field is irrigated, and all debris is suctioned.
- Inferior turbinectomies and inferior septoplasty are adjunctive procedures that may be indicated in cases of significant superior repositioning or when nasal obstruction is apparent. A vertical incision is made through the nasal mucosa overlying the inferior turbinates, and the inferior turbinates are identified. A Kelley or Allis clamp is used to grasp the inferior turbinate at its base, and electrocautery or heavy scissors are used to transect the turbinate. The nasal mucosa is closed using chromic gut sutures.
- In cases of superior maxillary repositioning, the inferior portion of the cartilaginous nasal septum is resected to prevent septal deviation against the superiorly repositioned and fixated maxilla.
- The patient is placed in maxillomandibular fixation (MMF) with the use of a surgical splint. The maxillomandibular complex is rotated into position, ensuring that the condyles are seated ideally within the glenoid fossa. Any interferences are removed to achieve even passive contacts and the appropriate preplanned vertical dimension of the maxilla. For surgery designed to alter the vertical dimension of the maxilla, the prerecorded measurements from the Kirschner wire are used to determine the amount of maxillary repositioning based on the presurgical workup.
Fixation is applied to the zygomaticomaxillary buttress and the nasomaxillary buttress (piriform rim) bilaterally (Figure 21.10; see also Figure 21.17, Case Report 21.2). Bone grafts may be placed within the osteotomy gaps for large advancements or inferior repositioning (Figure 21.11).
- After the application of rigid fixation, the patient is removed from MMF to assess occlusion, mandibular movements, and overall facial symmetries. Any occlusal or midline discrepancies, jaw movement asymmetries, nasal deviations, or areas of excessive bleeding should be corrected with the release of fixation and ensuring the removal of all bony interferences, complete condylar seating, the correction of septal deviation and achieving tissue hemostasis.
- An alar cinch suture is placed to minimize unaesthetic widening of the alar base.
- Mucosal closure is initiated with a V–Y closure (Figure 21.12) to avoid thinning of the upper lip. A single-prong skin hook is used to form the vertical leg of the closure, and is closed with several passes of chromic gut in a running fashion. The vertical leg is connected to the gingiva and closure is completed in a continuous, horizontal mattress fashion with chromic sutures (Figure 21.13).
- Prior to extubation, an orogastric tube is passed to empty contents of the stomach.
- The patient is placed into guiding elastics to help guide the jaw into occlusion.
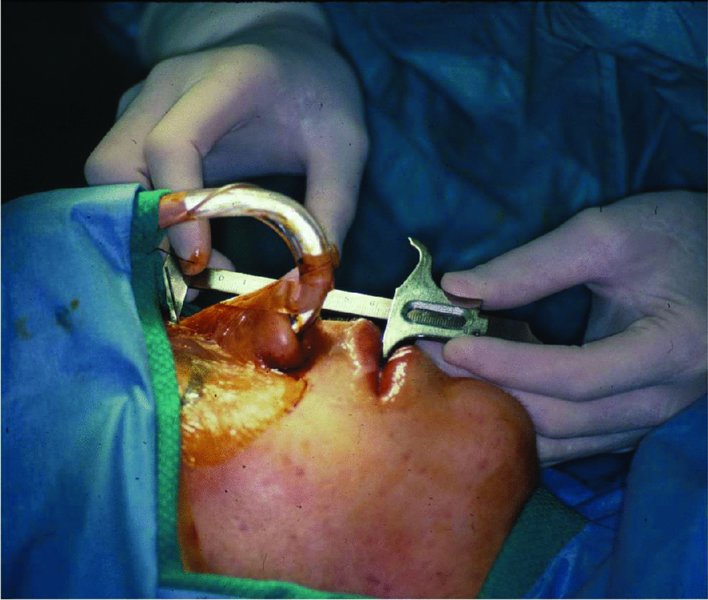
Figure 21.1. Patient prepped and draped. A midline vertical measurement is taken from a Kirschner wire placed within the nasofrontal suture to an anterior maxillary reference point (orthodontic brackets or incisal edges of the central incisors or the maxillary arch wire).
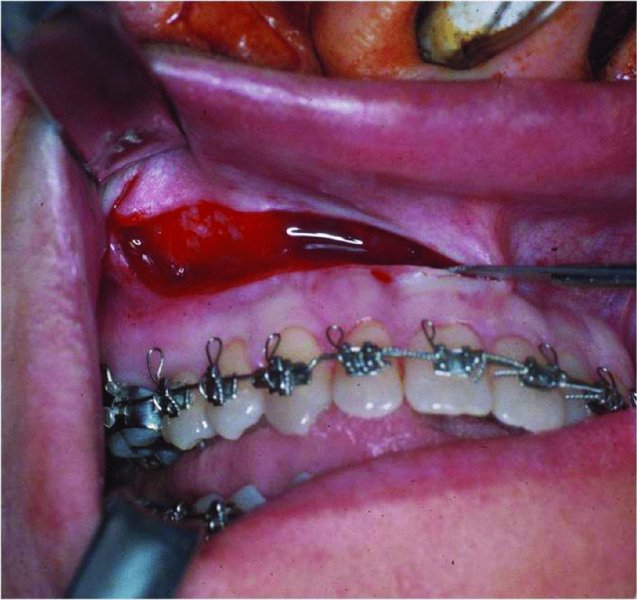
Figure 21.2. A vertical releasing incision is created anterior to the zygomaticomaxillary buttress in the area of the premolars and the incision is carried anteriorly to the midline.
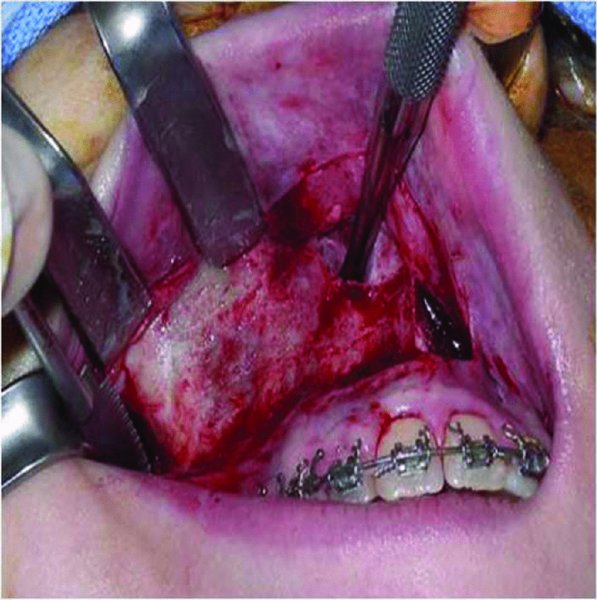
Figure 21.3. Subperiosteal elevation and exposure of the lateral wall of the maxilla. A subperiosteal pocket is made posteriorly to the pterygoid plates and along the lateral nasal wall. An elevator is placed to protect the nasal mucosa during the osteotomy.
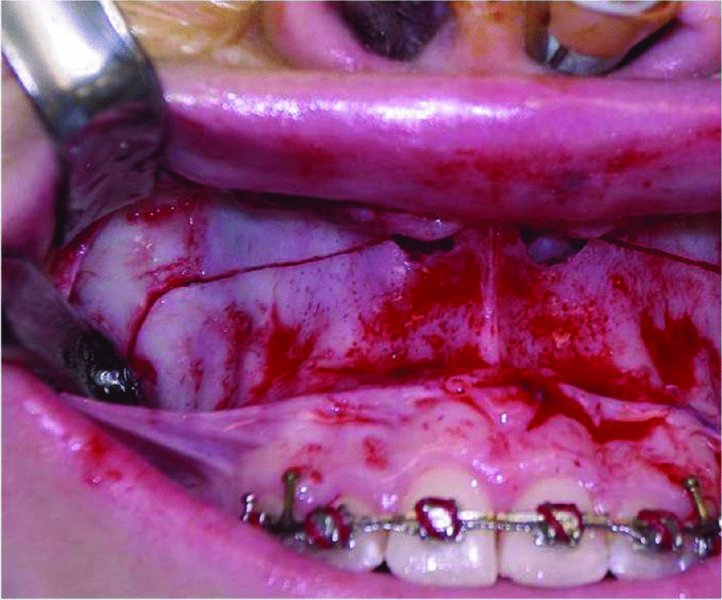
Figure 21.4. A reciprocating saw is used to create an osteotomy from the zygomaticomaxillary buttress to the lateral nasal wall at a point just superior to the nasal floor.
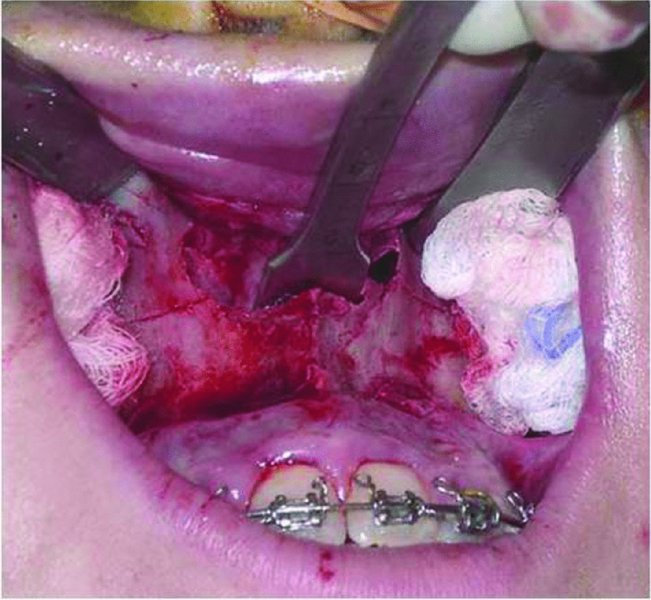
Figure 21.5. A vomer osteotome is used to separate the nasal septum and vomer from the nasal crest of the maxilla.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


